Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.5 Pretoria may. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i5.16602
RESEARCH
Operating theatre efficiency at a tertiary eye hospital in South Africa
M Tsimanyane; K Koetsie; A Makgotloe
FC Ophth (SA), MMed (Ophth); Department of Ophthalmology, Charlotte Maxeke Johannesburg Academic Hospital and Faculty of Health Sciences, University of the Witwatersrand., Johannesburg, South Africa
ABSTRACT
BACKGROUND: South Africa (SA) is a resource-limited country that needs efficient operating theatres in order for surgical care to function cost-effectively. Regular assessment of theatre efficiency in our setting is therefore needed
OBJECTIVES: To describe ophthalmology theatre efficiency at a central hospital in SA and compare this with international benchmarks
METHODS: St John Eye Hospital is the ophthalmology section of Chris Hani Baragwanath Academic Hospital in Soweto, SA. It has three operating theatres. A cross-sectional study was done of the theatres' registry of surgical procedures over a 6-month period. Data analysed included the starting and finishing times of theatre lists, surgical cases that were cancelled on the day of surgery, and theatre utilisation rates. These data were compared with international benchmarks
RESULTS: A total of 1 482 surgical procedures in 229 theatre lists were included in the study. Sixty-five percent of these theatre lists started late, accounting for 4 236 minutes of lost theatre time, significantly more than the maximum of 10% recommended by the Royal College of Anaesthetists. Of theatre lists, 23% and 30% finished after 16hl5 (theatre overrun) and before 16h00 (theatre underrun), respectively. This is more than double the 10% recommended by the Royal College of Anaesthetists. The theatre utilisation rate was 62%, which is significantly lower than the ideal utilisation rate of 80%. The cancellation rate was 16%, which is significantly higher than the international benchmark of 2% recommended by the New South Wales guidelines. The most common reasons for cancellations were medical unfitness of the patient and lack of operating theatre time
CONCLUSION: All theatre efficiency parameters at St John Eye Hospital were below international benchmarks
The South African (SA) public health system has limited resources and long surgical waiting lists. Efficient running of operating theatres is therefore particularly crucial given the limited budget. Operating theatre inefficiency is a significant cause of wasted resources.[1] In the USA, the cost of operating time has been estimated at USD22 -80 per minute.[1] In a 2018 study in SA, Samuel and Reed[2] found that theatre time costs ZAR32 per minute in a regional state hospital. In their costing model, they included as many relevant costs as they could, preferring to over-estimate costs in order to be as inclusive as possible. Although this figure gives an estimate of theatre costs in regional state hospitals, it is likely to be an underestimation for operating theatres in a central hospital.
Operating theatres are specialised facilities requiring highly specialised equipment as well as a high staff-to-patient ratio,[2] both of which account for a large proportion of a hospital's budget. Theatre inefficiency will therefore increase the operating costs of the hospital.
There is no clear definition of theatre efficiency, as it is measured by a variety of parameters. In public hospital operating theatres, theatre efficiency depends on the appropriate use of the limited resources and time to complete as many cases as possible, resulting in the reduction of long waiting lists. In the private sector, theatre efficiency can be defined as the use of the theatre to generate earnings, since money is earned only if the theatre is in use.[3]
Theatre efficiency can be measured by a variety of parameters. These include theatre utilisation rate, changeover time and cancellation rates, as well as procedure start times and overrun times.[3,4] Theatre utilisation measures the optimal use of the available operating theatre capacity. Short cases have a high turnover time and therefore tend to have low utilisation rates compared with long cases.[4] Ophthalmology theatres usually have shorter cases compared with other specialties, so they may have a lower utilisation rate compared with other specialties.
Theatre lists starting late result in time wasted at the beginning of the lists, and can result in theatre finishing later than the scheduled time, resulting in an increase in unbudgeted overtime costs and unplanned cancellation of cases.[5] The Royal College of Anaesthetists has suggested that a maximum of 10% of theatre lists should start later than 10 minutes after the scheduled starting time.[5] Estimation of theatre starting time and duration of the theatre case is important to avoid the underrunning and overrunning of theatre.[6]
Case cancellations can lead to delays in the operating theatre and contribute to low theatre utilisation. It is estimated that 60% of daily theatre cancellations are avoidable.[4,6] Cancellation of cases not only disrupts operating theatre lists, but also causes emotional stress and anxiety to patients and their families, disrupts their work, wastes their money, and affects trust in the health system.[1,4]
Theatre efficiency is particularly important in SA, where there are limited resources available in the public health sector. It is against this background that we decided to study ophthalmology theatre efficiency in a large tertiary eye hospital in SA, over a period of 6 months.
Methods
A cross-sectional study of surgical operations was performed over a 6-month period at St John Eye Hospital, a tertiary academic eye hospital in Diepkloof, Soweto. It serves a large population of Soweto and surrounding areas in Gauteng Province, and receives referrals from six secondary hospitals, two of which are the main referral hospitals in North West Province. It has three operating theatres, and elective lists run from Monday to Friday from 08h00 until 16h00 (8 hours/480 minutes). It has no dedicated emergency theatre, so emergencies are added onto the elective theatre list as they arise. This situation potentially results in cancellations of elective cases or an overrun of the list beyond the allocated 8 hours. The information recorded in the theatre register routinely includes the time the patient enters theatre, the time the patient is transferred onto the operating table, anaesthesia starting and finishing times, surgery starting and ending times, and the time the patient exits the operating theatre.
Data for this study were collected from the theatre register for surgical procedures performed from December 2018 to May 2019. Records for January 2019 were missing and could not be found at the time of collecting data. Elective lists during the month of December run from 1 to 14 December, when the elective lists for the hospital stop for the national festive holidays and resume on 15 January. All records with incomplete data for the study were excluded. Surgical procedures that were cancelled during this period were included in the study. The study data were de-identified and entered onto the REDCap (Research Electronic Data Capture) programme, which is hosted by the University of the Witwatersrand, and exported into Excel 2010 (Microsoft, USA).
Variables used to describe theatre efficiency in this study were:
• Theatre utilisation. Defined as the proportion of theatre time used to perform surgical operations as a percentage of the available theatre time (total theatre time used/total theatre time available). The time used is the time patients spend in the operating theatre, the recorded time indicating the period from the time when the patient enters the operating theatre to the time when they exit the operating theatre. This time includes the surgical and anaesthetic time. The time available refers to the normal hospital working hours, from 08h00 to 16h00 (480 minutes).
• Starting time. The time the patient is transferred onto the operating theatre bed.
• Finishing time. The time the patient exits the operating theatre.
• Cancellation rate. The proportion of cases booked on the list that are cancelled on the day of surgery.
• Theatre list 'late start'. When the first surgery case of the day is transferred onto the theatre table after 08hl5.
• Theatre list 'overrun'. When the last surgery case of the day exits the operating theatre after 16hl5.
• Theatre list 'underrun'. When the last surgery case of the day exits the operating theatre before 16h00.
Reasons for the cancellation of cases were categorised as either patient related or hospital related. Reasons for patient-related cancellations included being medically unfit, not arriving for surgery refusing surgery, incomplete surgical work-up, change in treatment plan, and others. Reasons for hospital-related cancellations were unavailability of theatre time, unavailability of the surgeon or nursing staff, equipment breakdown, power outage, theatre scheduling error, unavailability of beds, and others.
Statistical analysis
Statistical analysis was performed using Stata version 17 (StataCorp, USA). The Shapiro-Wilk test showed that the data were not normally distributed. Medians with interquartile ranges (IQRs) were therefore used to describe starting and finishing times and analysed using the Mann-Whitney (7-test. Categorical data were analysed using the χ2 test.
Ethics considerations
Ethics clearance was obtained from the Human Research Ethics Committee, University of the Witwatersrand (ref. no. M1911133).
Results
A total of 1 527 patient theatre records were collected. Twenty-nine of these records had incomplete data and 16 operations were performed on public holidays and were therefore excluded. These included some first and last cases on the lists (an attrition rate of 3%). A total of 1 482 cases in 229 surgery lists were included in the study. One hundred and thirty-five lists were under local anaesthesia and 94 were under general anaesthesia. The patients comprised 796 females (54%) and 686 males (46%), with a median (IQR) age of 52 (26 - 67) years (Table 1). Of the operations, 550 (37%) were performed under general anaesthesia and 932 (63%) under local anaesthesia (Table 1).
Starting time
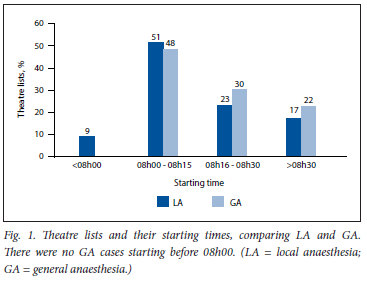
Of the operations, 224 were done as first case on the list. The overall median (IQR) starting time was 15 (5 - 30) minutes later than the scheduled start time (08h00), with lists under local anaesthesia 12.5 (0 - 30) minutes later and those for general anaesthesia 20 (10 - 30) minutes later than the scheduled start time. Of the lists, 124 (54%) started on time (by 08hl5); 81 (65%) of these lists were under local anaesthesia and 43 (35%) were under general anaesthesia. The list starting time was not statistically different between general anaesthesia and local anaesthesia (p=0.061). There were 4 236 minutes of total theatre time lost due to starting late. Fig. 1 shows the proportions of theatre list starting times.
Finishing time
There were 221 cases done as last case on the list. Overall, the median (IQR) finishing time was 30 (15 - 50) minutes later than the scheduled finishing time (16h00), with local anaesthesia cases finishing 30 (15 -30) minutes later and general anaesthesia cases 23 (10 - 40) minutes later than the scheduled finishing time.
Fifty lists (23%) overran (finished after 16hl5). Nine lists (18%) that overran did so by >60 minutes (finished after 17h00). Forty (80%) of the lists that overran were under local anaesthesia. The difference in finishing times between general and local anaesthesia was not statistically significant (p=0.324). Fig. 2 shows finishing times of theatre lists.
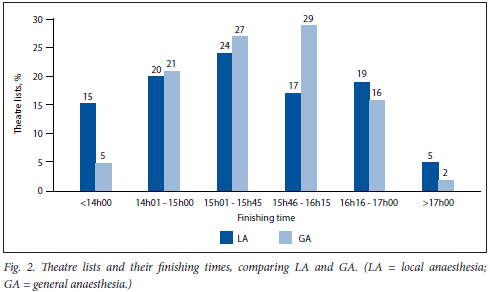
Of the lists, 136 (59%) underran (finished before 16h00); 66 (49%) underran by >60 minutes, accounting for a total of 8 275 minutes of lost theatre time.
Theatre utilisation
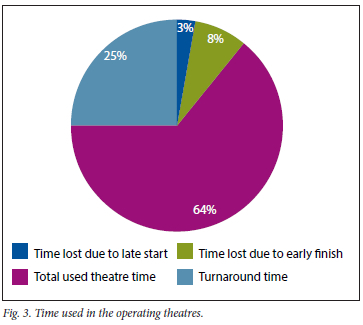
There were 128 640 minutes of theatre time available during the study period. Overall theatre utilisation was 82 330 minutes (64%).
Overrun theatre time can overestimate theatre utilisation, because it includes time outside of the available theatre time. To adjust for this potential overestimation of theatre utilisation rate, we removed the overrun time from our calculation, giving an overall theatre utilisation rate of 62%.
The turnaround time (time between patients, when the operating theatre has no patient in it) was 31 935 minutes, accounting for 25% of available total theatre time. Fig. 3 illustrates the use of available theatre time.
Cancellations
A total of 241 theatre cases were cancelled, giving a cancellation rate of 16%. Reasons for cancellation are listed in Table 2. One hundred and twenty-eight (53%) of the cancellations were patient initiated and 113 (47%) were hospital initiated. The most common reasons for patient-initiated cancellations were patients' medical unfitness (n=60; 47%) and patients' failure to come for surgery (n=43; 34%). The most common reasons for hospital-initiated cancellations were unavailability of theatre time (n=63; 56%) and lack of theatre equipment (n=30; 27%).
Medical unfitness was the most common reason for patient-initiated cancellations in both local (n=41; 68%) and general (n=19; 32%) anaesthesia lists. The most common reasons for hospital-initiated cancellations in general anaesthesia and local anaesthesia lists were unavailability of theatre time (n=27; 79%) and lack of theatre equipment (n=30; 54%), respectively.
Discussion
Access to ophthalmology health services in SA is limited, with long waiting lists and limited resources. In 2015, most patients on elective surgery waiting lists at a tertiary hospital in SA were waiting for an ophthalmological procedure, and these lists continue to grow[7]
There is still no consensus on national targets for theatre utilisation, starting times and cancellation rates in SA. Most studies use targets set elsewhere around the world, which are quite variable. Hartmann and Sunjka[3] found a 48% utilisation rate at an SA private hospital, while Asmal et αl.[8] found a 55% utilisation rate at a public SA hospital. In their study, they excluded overrun time in the calculation of utilisation rate, as it has been found to overestimate theatre utilisation. Ford et αl.[9] found a 59.8% utilisation rate in a paediatric theatre complex, where overrun time was also excluded in the calculation of theatre utilisation. A theatre utilisation rate of 80% is considered ideal.[4] We found an overall utilisation rate of 62% in our public facility, which is similar to the results of Asmal et al[8]
The definition of starting time differs between institutions. In an audit of ophthalmology theatre time at a Nigerian hospital, staff members working in the same operating theatre gave three different definitions of what constituted starting time:[10] the time the first patient on the list enters the operating theatre, the time the first patient on the list is anaesthetised, and the time the first patient on the list starts their operation. Similarly, in an audit in a Queensland public hospital, staff members gave different definitions of what they thought constituted theatre starting times.[11] These different definitions of theatre start time contribute to variability in published reports on delays in theatre starts and highlight the need for the definition of theatre start time to be standardised at each surgical unit, so that the staff members of each unit have a uniform definition of starting time recorded. For example, starting time in one unit might be when the patient arrives in the operating theatre, whereas in another unit it might be when the patient is anaesthetised. In our study, we defined start time as the time when the patient is transferred onto the theatre operating bed.
Lewis et al.[12] found that 91.3% of lists in a UK hospital started late, while locally in SA, Asmal et αl.[8] found that 74% of lists started late. Asmal et αl.[8] also defined theatre late starts as lists starting after 08hl5. In our study, 44% started late, which compares favourably with these other studies. Nevertheless, 4 236 minutes of theatre time were lost due to starting late. Our study did not report on the reasons for starting late. In their study, Asmal et al.[3] found that 46% of late starts were avoidable.
Older age and higher American Society of Anesthesiologists status (ASA IV) have been associated with delayed starting times in general anaesthesia lists. A possible strategy to reduce the number of late starts is to start the list with the golden patient'[13] - a young, usually medically well and appropriately investigated patient who is designated to be first on the list to minimise interruptions.
Theatre lists that end before their scheduled completion time also reduce theatre utilisation. In our study, underrunning by 60 minutes resulted in a total loss of 8 275 minutes during the study period, which equates to a 6% reduction in theatre utilisation. Ophthalmological procedures are generally short theatre cases, particularly if they are done under local anaesthesia. Theatre time equivalent to this 'lost time' could accommodate many procedures such as cataract surgery, and have a considerable impact on reducing ophthalmology waiting lists.
Overrunning lists incurs additional costs for work that is done overtime. Overrunning can also overestimate theatre efficiency.[8]
The Royal College of Anaesthetists recommends that fewer than 10% of lists should end over 15 minutes later than the scheduled finishing time.[5] Although specific reasons for overruns were not investigated in the present study, possible contributing factors may include the overbooking of theatre lists and prolonged operating times for procedures done by trainee junior surgeons.
Case cancellations on the day of surgery may lead to underrunning of theatres, resulting in wasted time and adding to the long waiting lists, to which the cancelled patients have to be added. An international benchmark for cancellations is 2%, according to New South Wales guidelines.[4] In our study the cancellation rate was 16%, which is significantly above the recommended rate.
The most common reason for patient-initiated cancellations was medical unfitness of patients. Some of the causes of medical unfitness were uncontrolled hypertension, hyperglycaemia and respiratory tract infections. A possible factor contributing to lack of optimal management of these uncontrolled medical conditions is poor patient compliance, as a direct result of a public primary healthcare system that is not readily accessible to the indigent, such as facilities located far from patients' homes, long queues at the point of care, and a public transport system that is just as inaccessible.
Preoperative assessments are usually done the day before surgery so it should be possible to identify patients who are not medically fit for surgery ahead of time and cancel the operation immediately. Some of the cancellations due to medical unfitness could have been avoided by optimising the patient's condition before surgery.
The most common hospital-initiated reason for cancellation in the present study was lack of theatre time (56%). SA has resource constraints, so it is not surprising that lack of theatre equipment was the second most common reason for hospital-initiated cancellations.
There are several limitations to the study. Its retrospective nature means that the data collected may have inaccuracies, and there may be missing data. The inclusion of December and January in our 6 months of data collection is a major limitation, as neither of these months is busy, with minimal elective surgery performed during this period. The theatre registry did not have reasons recorded for the delayed starting times, which could have given more information on specific causes of theatre inefficiencies.
Conclusions
This study adds to the understanding of factors affecting theatre efficiency. Although the theatre efficiency parameters are suboptimal, with large room for improvement, theatre utilisation of 62% and only 45% late starts are better than those found in other local studies. Scheduling of lists is very important and will improve most of the parameters that make for an efficient theatre. The overall cancellation rate of 16% is also suboptimal. To reduce cancellations and improve overall theatre efficiency, more attention should be paid to preoperative assessments, not only of the patients, but also of the equipment required on the day of surgery.
Declaration. The research for this study was done in partial fulfilment of the requirements for MT's MMed (Ophth) degree at the University of the Witwatersrand.
Acknowledgements. We thank Ms Zvifadzo Zingoni for her assistance with the statistical analysis.
Author contributions. MT: conception of the work, design of the work acquisition of data and analysis of data; drafting the manuscript and revising the work critically for important intellectual content; final approval of the version to be published; agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. KK: conception of the work, design of the work and analysis of data; revising the work critically for important intellectual content; final approval of the version to be published; agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AM: supervisor of the project; conception of the work, design of the work, acquisition of data and analysis of data; drafting the manuscript and revising the work critically for important intellectual content; final approval of the version to be published; agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding. None.
Conflicts of interest. None.
References
1. Soliman B, Stanton R, Sowter S, Rozen WR Shabaz S. Improving operating theatre efficiency. An intervention to significantly reduce changeover time. ANZ J Surg 2013;83(7-8):545-548. https://doi.org/10.1111/ans.12013 [ Links ]
2. Samuel JR Reed A. The cost of operating theatre time in a secondary-level state sector hospital. A quantitative observational study S Afr Med J 2021;111(6):595-600. https://doi.org/10.7196/SAMJ.2021.v111i6.15345 [ Links ]
3. Hartmann D, Sunjka B. Private theatre utilisation in South Africa. A case study S Afr Med J 2013;103(5):285-287. https://doi.org/10.7196/SAMJ.6460 [ Links ]
4. NSW Agency for Clinical Innovation. Operating theatre efficiency guidelines. A guide to the efficient management of operating theatres in New South Wales hospitals. December 2014. https://aci.healthnsw.gov.au/_data/assets/pdf_file/0004/252436/operating-theatre-efficiency-guidelines.pdf (accessed 8 March 2019). [ Links ]
5. Colvin JR, Peden CJ, eds. Raising the standard. A compendium of audit recipes for continuous quality improvement in anaesthesia. London. Royal College of Anaesthetists, 2012. https://wwwrcoa.ac.uk/sites/default/files/documents/2019-09/CSQ-ARB-2012_0.pdf (accessed 19 March 2022). [ Links ]
6. Balzer C, Raackow D, Hahnenkamp, Flessa S, Meissner K. Timeliness of operating room case planning and time utilisation. Influence of first and to-follow cases. Front Med (Lausanne) 2017;4:49. https://doi.org/10.3389/fmed.2017.00049 [ Links ]
7. South African Government. Gauteng Health on waiting lists for operations. 31 March 2015. https://www.gov.za/speeches/gauteng-health-waiting-list-operations-31-mar-2015-0000 (accessed 17 March 2022). [ Links ]
8. Asmal II, Keerath K, Cronje I. An audit of operatingtheatre utilisation and day-of-surgery cancellations at a regional hospital in the Durban metropole. S Afr Med J 2019;109(10):765-777. https://doi.org/10.7196/SAMJ.2019.vl09il0.13815 [ Links ]
9. Ford S, Brink N, Martin N, et al. Utilisation of paediatric surgical theatres at the Chris Hani Baragwanath Academic Hospital, Johannesburg. S Afr J Child Health 2021;15(4):185-188. https://doi.org/10.7196/SAJCH.2021.v15i4.1774 [ Links ]
10. Mpyet CD. An audit of the use of ophthalmic theatre time. Community Eye Health 2002;15(44):62-63. [ Links ]
11. Queensland Audit Office. Queensland public hospital operating theatre efficiency. 2015. https://www.qao.qld.gov.au/reports-resources/queensland-public-hospital-operating-theatre-efficiency (accessed 16 March 2021). [ Links ]
12. Lewis MA, Hall RD, Okolo S, et al. How time flies. A prospective analysis of theatre efficiency during elective gynaecology fists. Gynecol Surg 2012;9:213-217. https://doi.org/10.1007/s10397-011-0696-2 [ Links ]
13. Halim UA, Khan MA, Alii AM. Strategies to improve start time in the operating theatre. A systematic review. J Med Syst 2018;42(9):1-11. https://doi.org/10.1007/sl0916-018-1015-5 [ Links ]
 Correspondence:
Correspondence:
M Tsimanyane
khlcyn001@gmail.com
Accepted 24 February 2023














