Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.5 Pretoria Mai. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i5.16764
RESEARCH
The incidence and outcomes of high-risk acute coronary syndromes in Western Cape Province, South Africa: A prospective cohort study
J D CilliersI; L JoubertII; B BeyersIII; E NgarandeIV; P HerbstV; A DoubellVI; A PecoraroVI
IMB ChB; Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University, and Tygerberg Hospital, Cape Town, South Africa
IIMMed (Int), MPhil; Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University, and Tygerberg Hospital, Cape Town, South Africa
IIIMB ChB; Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University, and Tygerberg Hospital, Cape Town, South Africa
IVBSc Hons (Medical Biochemistry), PhD; Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University, and Tygerberg Hospital, Cape Town, South Africa
VMB ChB, MMed (Int); Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University, and Tygerberg Hospital, Cape Town, South Africa
VIMMed (Int), PhD; Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University, and Tygerberg Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND: Tygerberg Hospital (TBH) is a tertiary-level hospital in Western Cape Province, South Africa, that provides healthcare to a large low- to middle-income population with services including centralised advanced cardiac care. Acute coronary syndrome (ACS) remains an important cause of death in the region despite a high burden of communicable diseases, including HIV
OBJECTIVES: To describe the incidence of ST-elevation myocardial infarction (STEMI) and high-risk non-ST-elevation ACS (HR-NSTEACS) in the TBH referral network, describe the in-hospital and 30-day mortality of these patients, and identify important high-risk population characteristics
METHODS: The Tygerberg Acute Coronary Syndrome Registry database is an ongoing prospective study that enrols all STEMI and HR-NSTEACS patients in the TBH referral network. All patients aged >18 years presenting with STEMI or HR-NSTEACS were treated in accordance with current European Society of Cardiology guidelines and were included prospectively over a 9-month surveillance period. A waiver of consent was granted to include patients who died before giving informed consent. Data collected included a demographic profile, risk factors for cardiovascular disease, in-hospital therapy and 30-day mortality
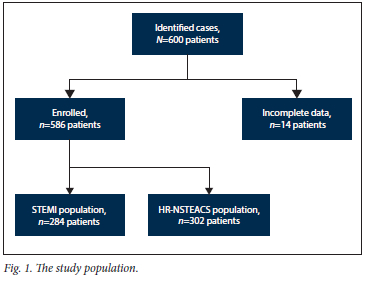
RESULTS: A total of 586 patients were enrolled, with a male predominance (64.5%) and incidence rates of STEMI and HR-NSTEACS of 14.7 per 100 000 and 15.6 per 100 000, respectively. The mean patient age was 58 years, and STEMI patients tended to be younger than HR-NSTEACS patients (56 v. 58 years; p=0.01). Cardiovascular risk factors were prevalent overall, but hypertension (79.8% v. 68.3%; p<0.01) and pre-existing IHD (29.1% v. 7.0%; p=0.03) were more prevalent in the HR-NSTEACS group. HIV was present in 12.6% of patients tested, similar to the background population rate. The overall 30-day all-cause mortality rate was 6.1%, with an in-hospital mortality rate of 3.9%. The 30-day mortality rates were similar for STEMI (1.8%) and HR-NSTEACS (2.6%) (p=0.75). HIV did not affect mortality rates
CONCLUSION: Use of a guideline-based approach to treating ACS in a low- to middle-income country setting yields mortality rates comparable to those in high-income countries. However, the lower-than-expected incidence rates of both STEMI and HR-NSTEACS in a relatively young population with a high prevalence of traditional cardiovascular risk factors, and a relatively high proportion of STEMI, suggest potential under-recording of ischaemic heart disease in the region. The rate and outcomes of coronary artery disease (CAD) in people living with HIV were similar to those in people without HIV, suggesting that traditional risk factors still drive CAD outcomes in the region
Cardiovascular disease (CVD) is the leading cause of death worldwide.[1] Despite a high burden of communicable disease, ischaemic heart disease (IHD) is the 10th most common cause of death in South Africa (SA), and recent data suggest that it is on the rise.[2] IHD was ranked as the most common cause of death in a recent survey in Western Cape Province, at 90 per 100 000.[3] SA is an upper-middle-income country (UMIC) as defined by the 2021 World Bank summary.[4] However, although SA is an UMIC, because of inequality in resource distribution a large proportion of its population face challenges characteristic of a low- to middle-income country (LMIC).[4]
Acute coronary syndrome (ACS), particularly ST-elevation myocardial infarction (STEMI) and high-risk non-ST-elevation ACS (HR-NSTEACS), is a major contributor to the mortality associated with IHD. Prospective registries from high-income countries in Europe (Euro Heart Survey)[5] and the USA (GRACE survey)[6] report in-hospital mortality rates for STEMI of 7% and 8%, respectively, with lower in-hospital mortality rates reported for non-ST elevation ACS (NSTEACS) (2.4% and 5%). The Euro Heart Survey reported 30-day mortality rates of 8.5% for STEMI and 3.5% for NSTEACS.[5,6] It should be noted that the NSTEACS groups in these studies were not limited to HR-NSTEACS patients. The outcomes of ACS have not been prospectively studied in SA, and the only available information comes from death notifications reported by the SA statistical services.[2]
European registries suggest a STEMI incidence of 50 - 60 per 100 000 patient-years of the population, with the incidence of HR-NSTEACS being almost double that of STEMI.[1,7] Data from our own unit suggest that STEMI is less common than reported in these high-income countries,[8] with no data available on the incidence of HR-NSTEACS in SA.[8] Whether this finding reflects a truly lower incidence of the condition or under-reporting and/or undertreatment of the population remains unknown. A prevalence of traditional risk factors for CVD similar to that in high-income countries has been reported in SA,[9] although the specific risk factor profile of the ACS population in SA remains unknown.[9] The prevalence of HIV, a possible additional risk factor for premature coronary artery disease (CAD) and ACS, is close to 10% in the Western Cape, with a treatment rate of ~30%.[10] A recent study from our institution reported an HIV prevalence of 3.4% in patients presenting with ACS.[11]
Protocolised management of ACS, and in particular patients with STEMI, has been shown to improve patient outcomes.[12] All patients in the Tygerberg Hospital (TBH) referral network presenting with STEMI and HR-NSTEACS are referred to TBH for definitive care, ultimately resulting in protocolised management of patients presenting with ACS, in keeping with current European Society of Cardiology (ESC) guidelines, throughout the region.[13]
Our objective was to describe the incidence, mortality rates and cardiovascular risk factor profile of patients presenting with STEMI and HR-NSTEACS in the TBH referral network and compare these with published cohorts.
Methods
The Tygerberg Acute Coronary Syndrome Registry is an ongoing prospective cohort study of patients with HR-NSTEACS and STEMI presenting to healthcare facilities in the TBH referral network. The Division of Cardiology at TBH, Cape Town, is a public sector tertiary referral centre that serves a population of ~2.4 million people. All patients with STEMI/HR-NSTEACS presenting to healthcare facilities in our referral network are referred to TBH for definitive care.[8]
All patients aged >18 years diagnosed with either STEMI or HR-NSTEACS were included in this prospective study for the period July 2020 - March 2021. A waiver of consent was granted to include patients who died before giving informed consent.
STEMI and HR-NSTEACS were defined using established definitions as outlined by current guidelines.[1,7] A STEMI diagnosis required patients to present with typical chest pain consistent with myocardial ischaemia, associated with ST-segment elevation in two contiguous leads of at least 1 mm on an electrocardiogram (ECG).[2,7] HR-NSTEACS was diagnosed in patients presenting with typical chest pain consistent with myocardial ischaemia without ST elevation, but with one of the following high-risk features: ongoing chest pain, haemodynamic or electrical instability, dynamic ST-or T-wave changes on the ECG, mainstem pattern on the ECG, ECG suggestive of a left anterior descending artery syndrome, or elevated troponin T level, TIMI score or Grace score, as per the ESC guidelines.[1,7] All patients were managed by a cardiologist and the diagnosis was independently verified by the study investigators. Prospective data collected included baseline demographic profile, risk factors for CVD, and in-hospital treatment outcome in terms of survival. All patients were offered guideline-directed therapy including coronary angiography with percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) as indicated.[1,7] Patients were contacted telephonically a month after discharge to confirm survival, evaluate their symptoms and assess compliance with medication.
In terms of treatment of patients with STEMI, a pharmaco-invasive strategy is followed. Patients receive fibrinolysis at their presenting hospital (spoke), provided no contraindication is present, followed by referral to TBH (hub) for angiography and consideration for PCI.[8] All patients with HR-NSTEACS are transferred to the hub for
angiography and further intervention. A forced referral pathway is therefore in place to ensure that all patients in our geographical service
area who present with STEMI and HR-NSTEACS are referred to TBH. The SUNHEART Cardiology Outreach Programme, established in 2013, created a hub-and-spoke model to deliver cardiovascular care in the TBH referral network in the Western Cape.[13]
Statistical analysis
Data were analysed using using SPSS Statistics version 27 (IBM Corp., USA). Data are expressed as means with standard deviations, medians with interquartile ranges and numbers with percentages, according to the order of the variables and distribution of data. Categorical variables were compared using cross-tabulation and the χ2 test. Comparisons between groups with normal distributions were performed using Student's f-test. Groups that were not normally distributed were compared using the Mann-Witney (7-test. A p-value of <0.05 was used to ascribe statistical significance.
The most recent census data report the population living within the TBH referral network to be 3 million.[8] Approximately 20% of this population has access to private healthcare, so the population used to calculate incidence rates was 2.4 million.[14]
Ethics approval
The study was approved by the Health Research Ethics Committee of the Faculty of Medicine and Health Sciences, Stellenbosch University (ref. no. N20/03/030), and performed in accordance with the Declaration of Helsinki (2013 version). All patients signed written informed consent. A waiver of consent was granted to include patients who died before being able to give informed consent.
Results
A total of 586 patients were enrolled over the 9-month study period (Fig. 1), with a male predominance (64.5%) and incidence rates for STEMI and HR-NSTEACS of 14.7 per 100 000 and 15.6 per 100 000, respectively (Table 1). The mean patient age was 58 years, with STEMI patients younger than HR-NSTEACS patients (56 v. 58 years; p=0.01).
The prevalences of the major cardiovascular risk factors diabetes mellitus, dyslipidaemia and smoking were similar in the two groups (Table 1). However, hypertension (79.8% v. 68.3%; p<0.01) and pre-existing IHD (29.1% v.7.0%; p=0.03) were significantly more prevalent in the HR-NSTEACS group.
HIV status was available for 183 patients (31.2%), with 12.6% of these patients being HIV positive. Nearly three-quarters of the patients in this cohort were on treatment with combination antiretroviral therapy, none of whom received protease inhibitors. People living with HIV (PLHIV) in this study were younger than those who were HIV negative (47 v. 58 years; p<0.01) and were more likely to present with a STEMI than with HR-NSTEACS (73.9% v. 26.1%; p<0.01), although their major cardiovascular risk profile was similar to that of HIV-negative patients (Table 2).
A total of 23 patients died in hospital, and a further 13 within 30 days of diagnosis. The all-cause mortality rate was 6.1% (n=36/586) at 30 days post admission, with an in-hospital mortality rate of 3.9% (n=23/586) and an out-of-hospital mortality rate of 2.2% (n=13/586) (Table 3). The in-hospital and out-of-hospital mortality rates were similar for the STEMI and HR-NSTEACS patients (Table 3).
The majority of patients underwent coronary angiography (n=571/586; 97.4%) (Table 4). Of these, 434 (76.0%) underwent revascularisation procedures, with the majority undergoing PCI (n=364; 63.7%) and 70 (12.3%) undergoing CABG. A relatively high proportion of patients (n=57/302; 18.9%) in the HR-NSTEACS group met the criteria for emergency angiography (5 of these patients had haemodynamic instability and 52 ongoing chest pain). Not having an angiogram was the only statistically significant factor influencing poor outcome (p<0.01). PCI was more frequently performed in STEMI patients than in those with HR-NSTEACS, with similar CABG rates across the groups (Table 4). Of the 15 patients who did not undergo angiography, 9 died before the intervention could be performed and 2 had severe renal failure.
COVID-19 status was available for 372/586 patients, with only 3.1% having a positive polymerase chain reaction (PCR) test. COVID-19 status did not influence the presenting diagnosis, with an equal distribution between STEMI and HR-NSTEACS (p=0.984). One patient with COVID-19 died within 30 days of admission, but there was no association between COVID-19 PCR positivity and 30-day mortality (p=0.81).
Discussion
This study demonstrates that the use of a contemporary guideline-based approach to treating ACS in an LMIC setting, as practised in our institution, can yield mortality rates comparable to outcomes from high-income countries. However, the lower-than-expected incidence rates of both STEMI and NSTEACS in a relatively young population with a high prevalence of traditional CAD risk factors, and a relatively high proportion of STEMI in the population, suggest potential under-recording of IHD in the region. The rate and outcomes of CAD in PLHIV were similar to those in HIVnegative people. However, PLHIV presented at a younger age with predominantly STEMI.
Similar in-hospital (4.9% v. 3.0%; p=0.46) and 30-day mortality rates (1.8% and 2.6%; p=0.75) for patients presenting with STEMI and HR-NSTEACS were observed, with the mortality rate in the STEMI group similar to published cohorts utilising a pharmaco-invasive strategy.[15] NSTEACS is traditionally associated with lower in-hospital and 30-day mortality compared with STEMI.[1,7] Our cohort only included the high-risk subgroup of NSTEACS patients, which may account for the similar mortality in the two groups. This finding is further supported by the similarity of our mortality data to reported mortality rates for HR-NSTEACS.[16,17] Mortality rates for both STEMI and NSTEACS have decreased with advances in medical therapy and improved access to angiography and revascularisation.[1,7] Access to healthcare services, in particular timeous angiography and PCI in the setting of ACS, is an important determinant of outcome. The availability of these services varies among countries, with high-income countries having easier and more equal access to angiography and PCI.[18]
The paucity of data from SA and Africa makes comparison with previously published data difficult. Previous data from our unit[8] reported a 30-day mortality rate of 6.4% for STEMI patients, while data from the SA private sector, which is considerably better resourced, showed a 30-day mortality rate of 4.1%.[19] Other studies from resource-limited countries in Africa, where access to healthcare, specifically angiography and PCI, may be more limited, have reported significantly higher mortality rates ranging from 22% to 28%.[20,21]
The majority of patients in our cohort underwent angiography with subsequent revascularisation (as per guideline indication), despite the typical constraints associated with cardiovascular care in the public healthcare sector in SA.[13,22] The ability to provide this service was made possible by centralising regional care in a hub-and-spoke model with a protocolised treatment approach to ACS.[13] Angiography with subsequent PCI or CABG is well established as an important strategy to lower the mortality and morbidity associated with both STEMI and HR-NSTEACS.[1,7] The high rate of access to angiography and subsequent revascularisation in our cohort is likely to have contributed to the lower-than-expected mortality rate (similar to developed-world cohorts) observed.
The prevalence of the major cardiovascular risk factors, including hypertension, diabetes mellitus and dyslipidaemia, was comparable to that in patients in other registries in the developed world as well as retrospective data from sub-Saharan Africa.[1,5,7,19,21,23] However, smoking was more prevalent in our population (69.1%) compared with developed-world cohorts (40 - 50%) and other cohorts from sub-Saharan Africa (20%).[7,23] Systemic hypertension was more prevalent in the HR-NSTEACS population than in the STEMI population (79.8% v. 68.3%; p<0.01), possibly owing to the more advanced age of the HR-NSTEACS population. Overall, our cohort of patients was younger, with a mean age of 58 years, compared with developed-world cohorts, which report a mean age of 65 - 68 years.[5,6]
In PLHIV, the incidence of STEMI was significantly higher than that of HR-NSTEACS (73.9% v. 26.1%; p=0.05), and patients with STEMI were younger at presentation (Table 3). Although we did not detect a difference in risk factor profile, the younger age of presentation with predominantly STEMI may be due to the chronic inflammation associated with HIV infection, but this finding requires further investigation.[23]
We found the incidence of STEMI and HR-NSTEACS to be 14.7 and 15.6 per 100 000, respectively, amounting to a total of 30.3 events per 100 000 patient-years. This figure is considerably lower than the incidence reported from high-income countries, where the incidence of STEMI is reported as 40 - 60 per 100 000, and that of NSTEACS as 80 - 120 per 100 000.[1,7]
The STEMI incidence in the present study is also lower than reported from a retrospective STEMI cohort identified in our unit over 12 months in 2018, where the incidence was 25 per 100 000.[8]
A number of factors should be considered as explanations for the lower-than-expected incidence observed. The average age of our population and patient cohort is lower than in developed countries.[2] However, despite this younger population, the prevalence of traditional risk factors for IHD is similar to that in developed countries. For this reason, a truly lower incidence of atherosclerotic disease and ACS in SA is unlikely. A decline in the incidence of ACS in cohorts from high-income countries over the past 2 - 3 decades has been associated with a greater decrease in the proportion of STEMI compared with NSTEACS. The STEMI-to-NSTEACS ratio has therefore been suggested as an important barometer of where along the IHD burden curve a population finds itself.[24] The relatively high rate of STEMI in the present study lends further support to the idea of underreporting rather than a true lower incidence of the disease. The lower incidence is probably at least in part explained by referral bias. Only patients referred to our facility were included, and poor health-seeking behaviour, under-detection of ACS at referral facilities,[9,25] pre-referral mortality and inappropriate discharge of patients diagnosed with ACS may therefore have affected the size of the cohort.[9] While it could be argued that the developed-world cohorts are subject to similar biases, the attrition rate may be higher in our cohort owing to the resource-limited nature of our healthcare system.
An additional explanation for the lower incidence may be the SARS-CoV-2 pandemic, which coincided with our enrolment period.[26,27] Local and international data indicated a decline in the number of ACS admissions during the pandemic, and this may be a significant contributor to the lower incidence observed.[27]
Study limitations
Although a protocolised referral system is employed in our referral network, we only captured data from the patients who were referred to our hospital, and this study is therefore limited by the usual factors associated with referral bias.
The study took place during the COVID-19 pandemic. During this period the incidences of both STEMI and NSTEACS were lower than normal. It is not possible to quantify the impact of the COVID-pandemic on all-cause mortality reported in this study.
Conclusions
The use of a contemporary, guideline-based approach to treating ACS in an LMIC setting yields mortality rates comparable to those in high-income countries. However, the lower-than-expected incidence rates of both STEMI and NSTEACS in a relatively young population with a high prevalence of traditional CAD risk factors, and a relatively high proportion of STEMI, suggest potential under-recording of IHD in the region. The rate and outcomes of CAD in PLHIV were similar to those in people without HIV, suggesting that traditional risk factors still drive CAD outcomes in the region.
Declaration. The research for this study was done in partial fulfilment of the requirements for JDC's MMed (Internal Medicine) degree at Stellenbosch University.
Acknowledgements. None.
Author contributions. JDC: investigation, writing original draft. LJ: conceptualisation, formal analysis, reviewing and editing. AP: conceptualisation, methodology, reviewing and editing. AD: conceptualisation, methodology, reviewing and editing. PH: reviewing and editing. EN: data capture, reviewing and editing. BB: reviewing and editing.
Funding. None.
Conflicts of interest. None.
References
1. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39(2):119-177. https://doi.org/10.1093/eurheartj/ehx393 [ Links ]
2. Statistics South Africa. Mortality and causes of death in South Africa, 2016: Findings from death notification. Statistical release P0309.3. Pretoria: Stats SA, 2018. https://www.statssa.gov.za/publications/P03093/P030932016.pdf (accessed 22 September 2022). [ Links ]
3. Sheik S, Evans J, Morden R, Coetzee D. Non-communicable diseases in the Western Cape: Burden of disease update. Epidemiology and Surveillance sub-directorate, Health Impact Assessment Unit, Western Cape Government: Health, 2016. https://www.westerncape.gov.za/assets/departments/health/burden_of_disease_update_ncds.pdf (accessed 21 October 2022). [ Links ]
4. World Bank. South Africa: Social assistance programs and systems review. 2021. https://documents1.worldbank.org/curated/en/238611633430611402/pdf/South-Africa-Social-Assistance-Programs-and-Systems-Review.pdf (accessed 20 October 2022). [ Links ]
5. Hasdai D, Behar S, Wallentin L, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin: The Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur Heart J 2002;23(15):1190-1201. https://doi.org/10.1053/euhj.2002.3193 [ Links ]
6. Steg PG, Goldberg RJ, Gore JM, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE). Am J Cardiol 2002;90(4):358-363. https://doi.org/10.1016/s0002-9149(02)02489-x [ Links ]
7. Roffi M, Patrono C, Collet J-P, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37(3):267-315. https://doi.org/10.1093/eurheartj/ehv320 [ Links ]
8. Beyers BD, Doubell AF, Griffiths B, Jalavu T. ST-segment elevation myocardial infarction: Evaluating the time interval from diagnosis to fibrinolysis at centres in the drainage area of Tygerberg Hospital, Cape Town, South Africa. S Afr Med J 2020;110(4):327-331. https://doi.org/10.7196/SAMJ.2020.v110i4.14330 [ Links ]
9. Stassen W, Kurland L, Wallis L, Castren M, Vincent-Lambert C. Barriers and facilitators to implementing coronary care networks in South Africa: A qualitative study. Afr Health Sci 2020;20(1):338-350. https://doi.org/10.4314/ahs.v20i1.39 [ Links ]
10. Western Cape Government: Health. Burden of disease. https://www.westerncape.gov.za/assets/departments/health/bod_a5_booklet_0.pdf (accessed 23 March 2023). [ Links ]
11. Pennefather C, Esterhuizen T, Doubell A, Decloedt EH. The 12-month period prevalence and cardiac manifestations of HIV in patients with acute coronary syndrome at a tertiary hospital in Cape Town, South Africa: A retrospective cross-sectional study. BMC Infect Dis 2021;21(1):657. https://doi.org/10.1186/s12879-021-06367-2 [ Links ]
12. Hertz JT, Reardon JM, Rodrigues CG, et al. Acute myocardial infarction in sub-Saharan Africa: The need for data. PLoS ONE 2014;9(5):e96688. https://doi.org/10.1371/journal.pone.0096688 [ Links ]
13. Van Deventer JD, Doubell AF, Herbst PG, et al. Evaluation of the SUNHEART Cardiology Outreach Programme. SA Heart 2015;12(2):82-86. https://doi.org/10.24170/12-2-1723 [ Links ]
14. Western Cape Government. Socio-economic profile (SEP): City of Cape Town, 2017. https://www.westerncape.gov.za/assets/departments/tre asury/Do cuments/Socio-economic-profiles/2017/city_of_cap e_town_2017_socio-economic_profile_sep-lg_-_26_january_2018.p (accessed 23 November 2023). [ Links ]
15. Armstrong PW, Gershlick AH, Goldstein P, et al.; STREAM Investigative Team. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med 2013;15:1379-1387. https://doi.org/10.1056/NEJMoa1301092 [ Links ]
16. Antman EM, Cohen M, Bernink PJLM, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA 2000;284(7):835-842. https://doi.org/10.1001/jama.284.7.835 [ Links ]
17. Van Leeuwen MAH, Daemen J, van Mieghem NM, et al. Comparison of long-term outcomes in STEMI and NSTE-ACS after coronary stent placement: An analysis in a real world BMS and DES population. Int J Cardiol 2013;167(5):2082-2087. https://doi.org/10.1016/j.ijcard.2012.05.064 [ Links ]
18. Gurm HS, Eagle KA. Channelling regional registries for optimisation of cardiac care: Lessons from around the world. Eur Heart J 2013;34(2):83-85. https://doi.org/10.1093/eurheartj/ehs328 [ Links ]
19. Schamroth C; ACCESS South Africa Investigators. Management of acute coronary syndrome in South Africa: Insights from the ACCESS (Acute Coronary Events - a Multinational Survey of Current Management Strategies) registry. Cardiovasc J Afr 2012;23(7):365-370. https://doi.org/10.5830/CVJA-2012-017 [ Links ]
20. Desta DM, Nedi T, Hailu A, et al. Treatment outcome of acute coronary syndrome patients admitted to Ayder Comprehensive Specialised Hospital, Mekelle, Ethiopia; A retrospective cross-sectional study. PLoS ONE 2020;15(2):e0228953. https://doi.org/10.1371/journal.pone.0228953 [ Links ]
21. Fanta K, Daba FB, Asefa ET, et al. Management and 30-day mortality of acute coronary syndrome in a resource-limited setting: Insight from Ethiopia. A prospective cohort study. Front Cardiovasc Med 2021;8:707700. https://doi.org/10.3389/fcvm.2021.707700 [ Links ]
22. Pecoraro AJK. Delivering cardiac care: The next frontier. SA Heart 2016;13(3):148-149. https://doi.org/10.24170/13-3-1595 [ Links ]
23. Onen CL. Epidemiology of ischaemic heart disease in sub-Saharan Africa. Cardiovasc J Afr 2013;24(2):34-42. https://doi.org/10.5830/CVJA-2012-071 [ Links ]
24. Alexander T, Mullasari AS, Kaifoszova Z, et al. Framework for a National STEMI Program: Consensus document developed by STEMI India, Cardiological Society of India and Association Physicians of India. Indian Heart J 2015;67(5):497-502. https://doi.org/10.1016/j.ihj.2015.05.017 [ Links ]
25. Maharaj RC, Geduld H, Wallis LA. Door-to-needle time for administration of fibrinolytics in acute myocardial infarction in Cape Town. S Afr Med J 2012;102(4):241-244. [ Links ]
26. Joubert LH, Herbst PG, Doubell AF, Pecoraro AJK. Clinical v. laboratory-based screening for COVID-19 in asymptomatic patients requiring acute cardiac care. S Afr Med J 2020;110(11):1064. https://doi.org/10.7196/SAMJ.2020.v110i11.15306 [ Links ]
27. Pecoraro AJK, Herbst PG, Joubert LH. Dwindling myocardial infarctions. Eur Heart J 2020;41(37):3497-3499. https://doi.org/10.1093/eurheartj/ehaa282 [ Links ]
 Correspondence:
Correspondence:
J D Cilliers
jdcilliersl23@gmail.com
Accepted 24 October 2022














