Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.3b Pretoria mar. 2023
http://dx.doi.org/10.7196/SAMJ.2022.v113i3b.16831
RESEARCH
The severe presentation and poor outcomes of rheumatic heart disease in Namibia: Lessons from the REMEDY study
T AualaI, II; L ZühlkeIII, IV; L SikwayaV; H du ToitVI; G KarthikeyanVII; K TeoVIII; S YusufIX; M E EngelX; B M MayosiXI, *; C T Hugo-HammanXII, XIII
IMB ChB; Cardiac Unit, Windhoek Central Hospital, Ministry of Health and Social Services, Namibia
IIMB ChB; Department of Medicine, Groote Schuur Hospital and University of Cape Town, Cape Town, South Africa
IIIMB ChB, PhD; Division ofPaediatric Cardiology, Department of Paediatrics and Child Health, Red Cross War Memorial Children's Hospital and University of Cape Town, Cape Town, South Africa
IVMB ChB, PhD; Department of Cardiology, All India Institute of Medical Sciences, New Delhi, India
IXMD, D Phil; Population Health Research Institute, Hamilton Health Sciences and McMaster University, Hamilton, ON, Canada
VMB ChB; Cardiac Unit, Windhoek Central Hospital, Ministry of Health and Social Services, Namibia
VIMB ChB; Cardiac Unit, Windhoek Central Hospital, Ministry of Health and Social Services, Namibia
VIIMD, DM; Department of Cardiology, All India Institute of Medical Sciences, New Delhi, India
VIIIPhD; Population Health Research Institute, Hamilton Health Sciences and McMaster University, Hamilton, ON, Canada
XPhD; Department of Medicine, Groote Schuur Hospital and University of Cape Town, Cape Town, South Africa
XIMB ChB, DPhil; The Deanery, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa
XIIMA, MB ChB, for the REMEDY investigators; Cardiac Unit, Windhoek Central Hospital, Ministry of Health and Social Services, Namibia
XIIIMA, MB ChB, for the REMEDY investigators; Division ofPaediatric Cardiology, Department of Paediatrics and Child Health, Red Cross War Memorial Children's Hospital and University of Cape Town, Cape Town, South Africa
ABSTRACT
BACKGROUND: This paper reports the baseline characteristics and outcomes of 266 Namibian patients in the Global Registry of Rheumatic Heart Disease
OBJECTIVE: To describe clinical findings and outcomes in a cohort of children and adults with rheumatic heart disease in Namibia
METHODS: Prospective study of all patients with rheumatic heart disease at Windhoek Central Hospital between January 2010 and November 2012
RESULTS: A total of 266 patients were enrolled; median age was 22 years, 72.6% were <30 years old and 60.5% female. The majority (62.8%) had moderate-severe disease; 48.9% were in congestive cardiac failure. Secondary antibiotic prophylaxis was used by 34.2%. Warfarin was used by 75.3% («=64/85) with clinical indications. Forty-seven (17.6%) had previous valve interventions, of whom 40 (15.0%) had mechanical valve replacements. Over a 2-year follow-up period 19.1% of patients died. Severe valve involvement at enrolment was independently associated with mortality (24.6% v. 5.1% in those without severe disease; hazard ratio 4.9; 95% confidence interval 1.50 -15.98). Sixty-five (29.8%) of the 218 without previous intervention had valvular intervention after enrolment
CONCLUSIONS: In Namibia rheumatic heart disease affects young people who present with severe disease and have a high case fatality rate. Rates of secondary prevention were low. These findings have informed the National Programme for Prevention and Control of Rheumatic Heart Disease in Namibia
Rheumatic heart disease is the consequence of acute rheumatic fever, which is caused by pharyngeal infection with Group A beta-haemolytic streptococcus.[1] The 2015 Global Burden of Disease Study estimates that more than 33 million persons living with rheumatic heart disease contribute to 319 400 deaths in every year.[2,3] It is the most common form of acquired heart disease among children and young adults in developing countries and affects ~ 0.5 - 3% of school-aged children in Africa.[3,4] Rheumatic heart disease is no longer a public health problem in most developed countries.[5] Historical studies from these countries describing clinical features, natural progression and outcomes may not be applicable to developing nations like Namibia, where rheumatic heart disease remains a major cause of cardiovascular morbidity and mortality[6,7]
Namibia is a large country in sub-Saharan Africa (824 292 km2) with a population of only 2.3 million people.[9] There were no cardiology services prior to 2008, and without capacity to manage patients with established rheumatic heart disease, there were no data on prevalence or incidence and no programme for the prevention of acute rheumatic fever or control of rheumatic heart disease.
A dedicated specialist-driven rheumatic heart disease clinic was established in 2010 and Namibia was one of the sites in the Global Rheumatic Heart Disease Registry (REMEDY), a multicentre, international prospective registry of patients with rheumatic heart disease conducted in 14 countries.[10] The objectives were to comprehensively describe patient demographics, pattern and severity of disease, measure outcomes and complications, assess risk factors, audit contemporary practice (prevention and treatment) and evaluate public health control activities.[6] The baseline characteristics and 2-year follow-up of individuals with rheumatic heart disease enrolled at the Namibia REMEDY site are reported here.
Methods
The study was conducted between July 2010 and November 2012 in the rheumatic heart disease clinic at the Windhoek Central Hospital, the national referral centre for patients with rheumatic heart disease. All patients with a diagnosis of rheumatic heart disease (confirmed with echocardiography) were invited to participate in the study, and this was done during their routine clinical visits. Enrolled patients were assessed and treated according to standard practices. This study was approved by the Permanent Secretary of the Ministry of Health and Social Services and informed consent was obtained from subjects or their guardians in the case of children (<18 years). The study design, data collection and statistical considerations of REMEDY were applied to the Namibian patients as described previously[10,11]
Results
Baseline characteristics
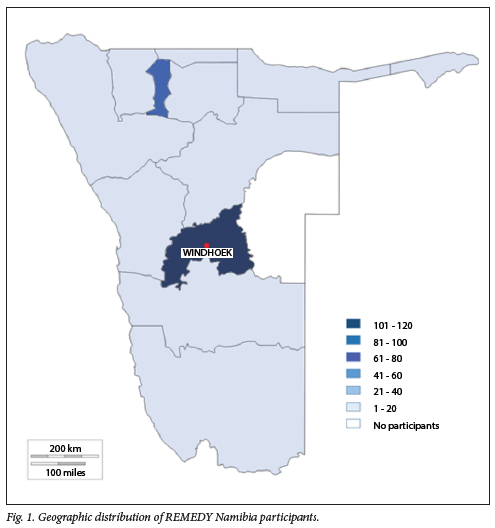
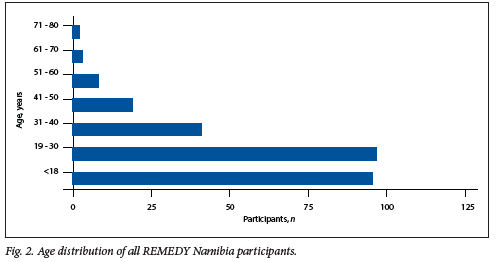
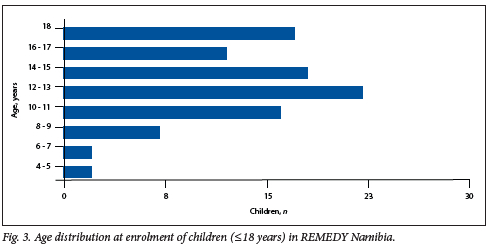
There were 266 patients enrolled in REMEDY Namibia between January 2010 and November 2012. The geographic distribution indicated that the majority of patients were referred from regions in excess of 700 km from the referral centre (Fig. 1). The patients were young, 96 (36.1%) were children <18 years of age, and 72.6% were <30 years of age (Fig. 2). The median age was 22 (interquartile range (IQR) 15 - 32) years. One hundred and sixty-one (60.5%) were female, a great proportion (87.6%) of whom were of childbearing age (between 12 and 51 years); of those 4 were pregnant. Among the children, 7 (2.8%) were <5 years old (Fig. 3). Only 32 (12.0%) were >40 years old (Fig. 2).
The clinical features and investigations at enrolment are shown in Table 1. Less than half the patients (40.2%) reported a history of acute rheumatic tever. Of the participants 28.7% were in New York Heart Association (NYHA) Class III or IV. Chest radiographs taken at baseline demonstrated cardiomegaly in two-thirds, pulmonary oedema in 8.3% and pleural effusions in 6.8%. At baseline there were 9 patients with a past history of infective endocarditis. In total, 47 patients had atrial fibrillation and 19 had cerebrovascular accidents (stroke).
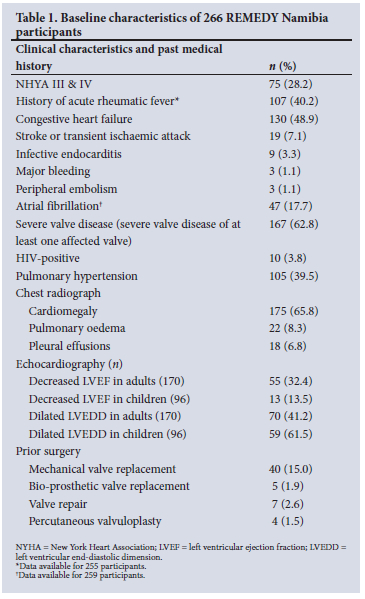
The mitral valve was the most commonly affected valve, with mitral regurgitation in n=192/266 (72.2%) and mitral stenosis in n=95/266 (35.7%). Mixed mitral valve disease was described in 29 (10.9%). Aortic valve disease manifested as regurgitation in 133 (50.0%) and stenosis in 17 (7%). Mitral and aortic valve disease were found in combination in 101 (37.9%) while only 2 patients had isolated aortic valve disease. The majority of cases had moderate to severe disease in respect of all valvular lesions (i.e. mitral regurgitation 69.8%, mitral stenosis 79.0%, aortic regurgitation 62.4% and aortic stenosis 58.8%). In total, 167 (62.8%) were assessed as having severe disease. Myocardial function was impaired with decreased ejection fraction in 26.3%; 5% were children.
Of 266 patients, 47 (17.7%) had previous surgery, with 85.1% (n=40/47) having mechanical valve replacements. Only 7/47 (14.9%) had bio-prosthetic or tissue valve replacements and 5 had mitral valve annuloplasty with valve repair. Percutaneous valvuloplasty was performed for mitral stenosis in 4 patients.
At baseline, secondary penicillin prophylaxis had not been prescribed in 65.8% (n=173/263) of patients. Of those on prophylaxis, intramuscular benzathine long-acting penicillin was the most common mode of administration, n=63/90 (70.0%). Oral anticoagulation (OAC) therapy (coumarin) was prescribed to 75.3% (n=64/85) of patients with clinical indications for anticoagulation; 31/35 (88.6%) with mechanical valves and n=33/50 (66.0%) with atrial fibrillation or flutter. Of patients taking OAC regardless of indication, less than half (41.5%) had international normalised ratio (INR) measured in the preceding 6 months. The INR at enrolment was recorded for 38.5% (n=25/65) of patients on anticoagulation in whom 8 were sub-therapeutic, 13 were within therapeutic range and 4 above the therapeutic range. There was no INR result available for 40/65 of patients on coumarin. The majority of participants (67.9%) were unaware of the therapeutic range of INR values.
Follow-up
Vital status was known for 241 (90.6%) participants, and clinical outcomes after 27 months follow-up are shown in Table 2. Forty-six patients (19.1%) died. The majority of deaths occurred in the first year of enrolment; 29 during the first 12 months (mortality rate 129.8/1 000 patient years) compared with 17 in the subsequent 15 months (mortality rate 76.7/1 000 patient years). The median age of death was 21.3 years (IQR 15.3 - 27.1), with the youngest recorded death a 6-year-old. The only risk factor at enrolment that was independently associated with mortality was severe valve involvement (24.6% v. 5.1% in those without severe disease; hazard ratio 4.9; 95% confidence interval 1.50 - 15.98).
During follow-up, there were no recurrences of acute rheumatic fever. Eight patients developed congestive heart failure (18.1/1 000 patient years), 4 atrial fibrillation (9.03/1 000 patient years), 3 stroke and 3 infective endocarditis. Seven pregnancies were reported during follow-up. Sixty-five (27%) patients had intervention over the 27-month period. Seven received percutaneous valvuloplasty for mitral stenosis and 58 had valve repair or replacement surgery.
Discussion
The major findings from this sub-study are firstly, that the demographic, clinical and outcomes data presented in the REMEDY study concealed very important disparities between Namibia and South Africa (SA). Secondly, patients present at a young age and with advanced valvular heart disease. Thirdly, there is a low use of secondary prophylaxis or of anticoagulation where indicated. Fourthly, the majority of patients live a great distance from the national referral centre.
The baseline and outcomes data for REMEDY grouped the 14 participating countries into three income categories according to the 2011 World Bank definitions of low-, lower-middle and upper-middle-income countries (which includes Namibia and SA).[10-12] The presentation of the data in this manner masked several important differences between Namibia and SA. The median age at presentation for all patients from upper-middle-income countries was 39 whereas the median age for Namibia was 22 years, which is more congruent with that of low-income countries in REMEDY[10] Similarly, children <18 years of age represented 36% of Namibian patients compared with 19.4% in the upper-middle-income group, again more in keeping with low-income countries.[10] The proportion of women of childbearing age in Namibia was 87%, vastly in excess of that for upper-middle income countries (66.9%) and even exceeding that for low-income countries.[10] Most importantly, the case fatality rate at the end of follow-up was 12.5% for the upper-middle income cluster; however, in Namibia, the reported rate of 19.1% is higher even than that observed in lower-middle-income countries (16.8%) and closer to the rate observed in low-income countries (20.8%).[11] The demographic, clinical and outcomes data presented in the REMEDY study have concealed these very important disparities between Namibia and SA.
Patients presented young and with advanced disease; almost half had a past history of congestive cardiac failure, a third were in NYHA Class III or IV, the majority with moderate to severe valvular heart disease, and a quarter had objective evidence of impaired left ventricular function. Severe disease impacts survival where a staggering number, almost one-fifth of patients enrolled and followed-up, died (19.1%) These patients were very young (median age of 21.3 years (IQR 15.3 - 27.1)). Whereas life expectancy in Namibia is 63.1 years for men and 68.5 years for women, only 10% of patients at baseline were older than 40 years.[13] The significant drop in number of patients over the age of 40 suggests early death could be a characteristic of rheumatic heart disease in Namibia. The number of patients that developed congestive heart failure, atrial fibrillation, infective endocarditis, were hospitalised or that received surgical intervention reflects significant morbidity from rheumatic heart disease.
Rheumatic heart disease is known to show a female preponderance and this is confirmed in Namibia.[14] Almost 90% of female participants were of childbearing age. Heart failure is an added risk factor for pregnancy.[15] There is high morbidity and mortality associated with rheumatic heart disease in pregnancy.[16] Work from Senegal has shown that rheumatic heart disease is associated with a maternal mortality rate of 34% in pregnancy and a high rate of fetal loss among survivors.[17] Official figures reveal maternal mortality is 265/100 000 live births in Namibia and the contribution of rheumatic heart disease to maternal morbidity and mortality requires further investigation.[18]
There is evidence that long-acting benzathine penicillin administered every 3-4 weeks by intramuscular injection reduces recurrent episodes of acute rheumatic fever in people with established rheumatic heart disease. [19] It is also superior to twice daily oral penicillin.[20] The administration of and adherence to penicillin therapy is in many ways a barometer for prevention strategies within a health system.[19,21] At baseline, penicillin had been prescribed in only one-third of patients with rheumatic heart disease. Low use of penicillin prophylaxis suggests a lack of awareness that penicillin prophylaxis is imperative for secondary prevention. These data reflect health system weaknesses which demand enquiry and comprehensive intervention.[10]
Patients with atrial fibrillation or with prosthetic mechanical heart valves ought to be using OAC medication to prevent left atrial thrombus and prosthetic valve thrombosis.[22] The low numbers of patients on OAC and the lack of knowledge about target INRs reflect a lack of awareness about good clinical practice and difficulty with INR monitoring in remote areas. The fact that a third of patients on coumarin had not had an INR for over 6 months shows significant non-compliance and a poor penetration of highly relevant clinical knowledge among health professionals. These data point the way to much-needed targeted health education interventions.
The study was based in a tertiary referral hospital and in this context the severity of disease is not unexpected but reflects a great number of late presentations of severely affected patients. The geographic distribution of patients mimics the population distribution of Namibia. Although the majority of the patients were enrolled in Windhoek more than half (60%) were referred from the northern regions (700 km away). Large distances bring significant health service challenges relating to access to care, surgery and follow-up.
There are important implications for clinical practice and health policy revealed in this study, with red flags raised, including suboptimal utilisation of penicillin prophylaxis for secondary prevention and inadequate OAC use. With adequate medical care rheumatic heart disease is preventable. The persistence of this disease is a mirror for the effectiveness of the primary health care system. This study has contributed to the development of a national programme for the prevention and control of rheumatic heart disease using the Pan-African Society of Cardiology (PASCAR)-driven A.S.A.P. Programme, which calls for efforts to increase awareness of rheumatic fever and rheumatic heart disease among the general public and practitioners; the establishment of surveillance programmes to measure the burden of disease in the population; advocacy to increase allocation of resources for the treatment of affected children and young adults; and the implementation of primary and secondary prevention schemes.[23,24] REMEDY has been used in Namibia as a foundation for a national prospective surveillance tool for all patients with rheumatic heart disease in the country, thus becoming one of the few countries in the world where all patients with rheumatic heart disease are enrolled in a register. The importance of needs-driven health systems research cannot be underestimated. REMEDY has proven that by documenting the burden and severity of disease, research is in itself an agent for change.
Conclusion
In Namibia patients with rheumatic heart disease present at an early age yet manifest with severe valve involvement, require costly high-end surgical interventions and have a high mortality rate comparable with other low-middle-income or low-income countries. The REMEDY study in Namibia has highlighted the gaps existing in current health services and the urgent need for more robust application of known evidence-based solutions to prevent and manage the complications of rheumatic heart disease.
Declaration. The authors dedicate this manuscript to the late Prof. Bongani Mayosi, who was a dear colleague, friend and mentor. He was the inspiration for REMEDY
Acknowledgements. Andreas Wilberg, Angeline Bock, Antoinette Awases, Brenda Kaaya, Gonda Olivier, Progress Mhangami, Sphamandla Nzuza assisted with data collection. Collaborators: The REMEDY Investigators: clinical investigators and sites: Egypt: Benha University: Azza Abul Fadl (Principal Investigator); Cairo University: Sahar S She ta (Principal Investigator). Ethiopia: University of Jimma: Abraham Haileamlak (Principal Investigator); University of Addis Ababa: Senbeta G Abdissa, Dufera M Begna, Wandimu Daniel, Araya G Desta, Dejuma Yadeta Goshu (Principal Investigator), Bekele A Shasho. Kenya: University of Nairobi: Bernard Gitura, Stephen Ogendo (Principal Investigator). Malawi: University of Malawi: Neil Kennedy (Principal Investigator). Mozambique: Eduardo Mondlane University: Albertino Damasceno (Principal Investigator); Instituto Nacional de Saúde: Ana Olga Mocumbi (Principal Investigator). Namibia: Windhoek Hospital: Christopher Hugo-Hamman (Principal Investigator). Nigeria: University of Abuja: Dike Ojji (Principal Investigator); University of Jos: Ganiyu A Amusa, Fidelia Bode-Thomas (Principal Investigator), Christopher C Yilgwan, Olukemi Ige, Basil Okeahialam; Kano University: Mahmoud U Sani (Principal Investigator); University of Ibadan: Okechukwu S Ogah (Principal Investigator); Federal Medical Centre, Abeokuta: Taiwo Olunuga; University College Hospital, Ibadan: Abiodun M Adeoye, Okechukwu Ogah (Principal Investigator). Rwanda: King Faisal Hospital: Joseph Mucumbitsi (Principal Investigator). South Africa: University of Cape Town: Blanche Cupido; University of Limpopo: Phindile Mntla (Principal Investigator), Christopher Sutton (Principal Investigator), Rajeev Misra. Sudan: Alzaiem Alazhari University: Ahmed ElSayed (Principal Investigator), Ahmed S Ibrahim; Ahmed Gasim Teaching Hospital: Huda HM Elhassan (Principal Investigator). Uganda: Makerere University: Peter Lwabi, Charles Mondo (Principal Investigator), Emmy Okello. Yemen: University of Sanaa: Mohammed M Al-Kebsi (Principal Investigator). Zambia: University of Lusaka: John Musuku (Principal Investigator).
Author contributions. TA prepared the first draft of the manuscript. LZ analysed the data. LS was a study doctor engaged with recruitment. HdT was a study doctor and surgeon for most patients needing surgery. GK, KT, SY MEE, LZ and BMM comprised the steering committee for the REMEDY study design. CTH-H was the principal investigator involved in all aspects of this study.
Funding. The REMEDY study is funded by grants from the Canadian Network and Centre for Trials Internationally (CANNeCTIN), South African Medical Research Council, Lily and Ernst Hausmann Trust, the Else Kroner Frasenius Foundation, the University of Cape Town, the National Research Foundation of South Africa, and the World Heart Federation. The Namibian sub-study and the National Registry for Rheumatic Heart Disease is funded by the Harold and Ethel Pupkewitz Heart Foundation.
Conflicts of interest. None.
References
1. Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group a streptococcal diseases Lancet Infect Dis 2005;5(11):685-694. https://doi.org/10.1016/S1473-3099(05)70267-X [ Links ]
2. Watkins DA, Johnson CO, Colquhoun SM, et al. Global regional, and national burden of rheumatic heart Disease, 1990-2015. N Engl J Med 2017;377(8):713-722. https://doi.org/10.1056/NEJMoal603693d [ Links ]
3. Paar JA, Berrios NM, Rose JD, et al. Prevalence of rheumatic heart disease in children and young adults in Nicaragua. Am J Cardiol 2010;105(12):1809-1814. https://doi.org/10.1016/j.amjcard.2010.01.364 [ Links ]
4. Damasceno A, Mayosi BM, Sani M, et al. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries. Arch Intern Med 2012;172(18):1386-1394. https://doi.org/10.1001/archinternmed.2012.3310 [ Links ]
5. Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet 2012;379(9819):953-64. PubMedPMID. 22405798. https://doi.org/10.1016/S0140-6736(11)61171-9 [ Links ]
6. Karthikeyan G, Zütüke L, Engel M, et al. Rationale and design of a Global Rheumatic Heart Disease Registry. The REMEDY study Am Heart J 2012;163(4):535-540.el. https://doi.org/10.1016/j.ahj.2012.01.003 [ Links ]
7. Newsholme A. The Milroy Lectures on the Natural History and Affinities of Rheumatic Fever. Delivered before the Royal College of Physicians of London, March, 1895. Br Med J 1895;1(1785):581-583. [ Links ]
8. Bland EF, Duckett Jones T. Rheumatic fever and rheumatic heart disease. A twenty year report on 1000 patients followed since childhood. Circulation 1951;4(6):836-843. [ Links ]
9. Government of Namibia. About Namibia. The Land and Population. http://www.gov.na/population (accessed 23 March 2017). [ Links ]
10. Zütüke L, Engel ME, Karthikeyan G, et al. Characteristics, complications, and gaps in evidence-bast interventions in rheumatic heart disease. The Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J 2015;36(18):1115-1122a. https://doi.org/10.1093/eurheartj/ehu449 [ Links ]
11. Zütüke L, Karthikeyan G, Engel ME, et al. Clinical outcomes in 3343 children and adults with rheumatic heart disease from 14 low- and middle-income countries. Two-year follow-up of the Global Rheumatic Heart Disease Registry (the REMEDY Study). Circulation 2016-;134(19):1456-1466. https://doi.org/10.1161/circulationaha.116.024769 [ Links ]
12. World Bank World Bank Country and Lending Groups. 2016. https://datahelpdeskworldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed 22 September 2022). [ Links ]
13. World Health Organization, Global Health Repository Data. 2016. www.who.int/gho/data (accessed 23 March 2017). [ Links ]
14. Lawrence JG, Carapetis JR, Griffiths K, Edwards K, Condon JR Acute rheumatic fever and rheumatic heart disease. Incidence and progression in the Northern Territory of Australia, 1997 to 2010. Circulation 2013;128(5):492-501. https://doi.org/10.1161/circulationaha.113.001477 [ Links ]
15. Mocumbi AO, Stiwa K. Womens cardiovascular health in Africa. Heart 2012:98(6).450-455. [ Links ]
16. Sliwa K, Mayosi BM. Recent advances in the epidemiology, pathogenesis and prognosis of acute heart faüure and cardiomyopathy in Africa. Heart 2013;99(18):1317-1322. https://doiorg/10.1136/heartjnl-2011-301025 [ Links ]
17. Diao M, Kane A, Ndiaye MB, et at. Pregnancy in women with heart disease in sub-Saharan Africa. Arch Cardiovasc Dis 2011,104(6-7).370-374. PubMed PMID. 21798468. https://doi.org/10.1016/j.acvd.2011.04.001 [ Links ]
18. The World Bank. Indicators. Maternal Mortality Ratio 2015 www.data.worldbankorg/indicator/SH.STA.MMRT (accessed 30 June 2017). [ Links ]
19. Manyemba J, Mayosi BM. Penicilin for secondary prevention of rheumatic fever. Cochrane Database jys Rev 2002(3). PubMed PMID; 12137650 https://doi.org/10.1002/14651858.CD002227 [ Links ]
20. Manyemba J, Mayosi BM. Intramuscular penicillin is more effective than oral penicillin in secondary prevention of rheumatic fever. A systematic review. S Afr Med J 2003;93(3):212-218. [ Links ]
21. Remenyi B, Carapetis J, Wyber R Taubert K, Mayosi BM. Position statement of the World Heart Federation on the prevention and control of rheumatic heart disease. Nat Rev Cardiol 2013;10(5):284-92. https://doi.org/10.1038/nrcardio.2013.34 [ Links ]
22. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease. Executive summary. A report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(23):2440-2492. https://doi.org/10.1016/j.jacc.2014.02.537 [ Links ]
23. Hugo-Hamman C, Forster N. National Advisory Committee for the Prevention and Control of Rheumatic Fever and Rheumatic Heart Disease in Namibia. Cardiovasc J Afr 2015;26(6):251. PubMed PMID: 26659439 [ Links ]
24. Mayosi B, Robertson K, Volmink J, et at. The Drakensberg declaration on the control of rheumatic fever and rheuma tic heart disease in Africa. S Afr Med J 2006;96(3 Pt 2):246. [ Links ]
 Correspondence:
Correspondence:
C Hugo-Hamman
christopher.hugo@gmail.com
Accepted 12 September 2022
* Deceased














