Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.4 Pretoria abr. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i4.833
RESEARCH
The impact of a decentralised orthopaedic service on tertiary referrals in Cape Town, South Africa
T MacQueneI; J du ToitII; D HugoIII; M AlexanderIV; S RamasarV; M LetswaloVI; M SwanepoelVII; C BrownVIII,*; K ChuIX, X,*
IBMedSci, MSc; Centre for Global Surgery, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIMB ChB, FC (Orth) SA; Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town South Africa
IIIMB ChB, FC (Orth) SA; Department of Orthopaedic Surgery, Khayelitsha District Hospital, Cape Town, South Africa
IVMB ChB; Department of Orthopaedic Surgery, Khayelitsha District Hospital, Cape Town, South Africa
VMB ChB; 6th-year medical student, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIMB ChB; 5th-year medical student, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIIMB ChB; 6th-year medical student, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIIIMB ChB, FRACS (Orth); Department of Orthopaedic Surgery, Khayelitsha District Hospital, Cape Town, South Africa
IXMD, MPH; Centre for Global Surgery, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
XMD, MPH; Department of Surgery, Faculty of Medicine, University of Botswana, Gaborone, Botswana
ABSTRACT
BACKGROUND: In South Africa (SA), district hospitals (DHs) have limited capacity to manage the high burden of traumatic injuries. Scaling up decentralised orthopaedic care could strengthen trauma systems and improve timely access to essential and emergency surgical care (EESC). Khayelitsha township in Cape Town, SA, has the highest trauma burden in the Cape Metro East health district
OBJECTIVES: The primary objective of this study was to describe the impact of Khayelitsha District Hospital (KDH) on acute orthopaedic services in the health district, with a focus on the volume and type of orthopaedic services provided without tertiary referral
METHODS: This retrospective analysis described acute orthopaedic cases from Khayelitsha and their management between 1 January 2018 and 31 December 2019. Orthopaedic resources and the proportion of cases referred to the tertiary hospital by all DHs in the Cape Metro East health district are described
RESULTS: In 2018 - 2019, KDH performed 2 040 orthopaedic operations, of which 91.3% were urgent or emergencies. KDH had the most orthopaedic resources and the lowest referral ratio (0.18) compared with other DHs (0.92 - 1.35). In Khayelitsha, 2 402 acute orthopaedic cases presented to community health clinics. Trauma (86.1%) was the most common mechanism of injury for acute orthopaedic referrals. Of clinic cases, 2 229 (92.8%) were referred to KDH and 173 (7.2%) directly to the tertiary hospital. The most common reason for direct tertiary referral was condition related (n=157; 90.8%
CONCLUSION: This study outlines a successful example of a decentralised orthopaedic surgical service that increased EESC accessibility and alleviated the high burden of tertiary referrals compared with other DHs with fewer resources. Further research on the barriers to scaling up orthopaedic DH capacity in SA is needed to improve equitable access to surgical care
Traumatic injury is a leading cause of disability and is associated with an annual estimated 5.8 million deaths worldwide, with 90% of the deaths occurring in low- and middle-income countries (LMICs).[1] The burden of death due to intentional and unintentional injury is disproportionately high in LMICs, where economic growth often outpaces the development of road safety infrastructure and trauma care systems.[2,3] The vast majority of acute orthopaedic conditions in LMICs are traumatic fractures, which can result in excess morbidity and mortality due to infection, malunion or disability if left untreated.[4,5] Sub-Saharan Africa (SSA) has limited capacity to manage its large burden of traumatic fractures and other acute orthopaedic conditions, as many hospitals lack surgical providers with orthopaedic training and formal emergency departments.[6]
Individuals with traumatic injury often present at district hospitals (DHs), but decentralised orthopaedic surgery services in many LMICs are limited.[7,8] A previous review reported that acute musculoskeletal injuries needing urgent attention are among the most common conditions treated at DHs.[2] In Uganda, road traffic accidents disproportionately present to DHs compared with higher-level facilities.[9] The specific package of acute orthopaedic care at DHs has not been well defined. As such, definitive surgical care for acute orthopaedic conditions is usually provided at regional and tertiary hospitals, leading to long wait times and considerable strain on the surgical services at these facilities.[10,11] The Lancet Commission on Global Surgery stated that all DHs should be able to stabilise open femur fractures,[12] but did not offer additional guidance as to what other acute orthopaedic care should be included in a DH surgical package. In addition, the World Health Organization recommended that DHs provide the backbone of surgical care, including services for essential and emergency surgical care (EESC), of which the provision of surgical services for acute orthopaedic conditions forms an integral part.[13] Describing current models of decentralised orthopaedic services in SSA will help provide recommendations to policymakers on how these services can be scaled up across the region.
In South Africa (SA), the rate of trauma is seven times higher than the global average, and trauma is a leading cause of morbidity[14] Cape Town is one of the largest cities in SA, with a population of ~5 million in 2021. Khayelitsha is a densely populated urban township in Cape Town, home to over half a million persons, and served by Khayelitsha District Hospital (KDH). KDH treats 3 000 patients a month, of whom almost half have trauma-related injuries.[15-17] The primary objective of this study was to describe the contribution of a decentralised orthopaedic service developed at KDH for the treatment of acute orthopaedic conditions in the Cape Metro East health district. The orthopaedic case volume and its impact on tertiary referrals of all DHs in the health district are described.
Methods
Study design
This was a retrospective review of operative and referral data from 1 January 2018 to 31 December 2019.
Study site
Khayelitsha township has 11 community health clinics (CHCs) and one DH (KDH), and refers to the Metro East tertiary hospital, Tygerberg Academic Hospital (TAH), as needed. TAH has 24-hour operative services for acute orthopaedic conditions, but also long waiting operative lists for EESC. KDH started an orthopaedic service in 2015. Initially only staffed by family physicians and medical officers, since 2019 it has been led by two orthopaedic surgeons working with two medical officers, a community service doctor and an intern. The other three DHs in the Metro East health district namely Karl Bremer Hospital (KBH), Helderberg Hospital (HH) and Eerste River Hospital (ERH), do not have full-time orthopaedic surgeons.
Data sources
Orthopaedic resources (staffing and operating theatre time) for each DH at the end of 2019 were obtained from hospital key informants. Operative volumes for orthopaedic cases for all Cape Metro East DHs between 1 January 2018 and 31 December 2019 were obtained from operating theatre registries. Tertiary referrals from all DHs to TAH were obtained from the Vula Mobile App, a secure medical referral app established in 2016 and endorsed by the SA National Department of Health for interfacility referrals between public sector hospitals. Condition type and volume for acute orthopaedic conditions from Khayelitsha CHCs and KDH were also extracted from Vula Mobile.
Data collection and analysis
Data extracted from the Vula Mobile database via Google Query were imported into Stata 15 SE (StataCorp, USA) for analysis. Variables included patient age, gender, acute orthopaedic condition, trauma (yes/no), referring facility, referral facility, mechanism of injury and anatomical location. Referral outcomes were categorised as advice only, inpatient, and outpatient transfer. Conditions were categorised as closed fracture, open fracture, soft-tissue injury, infection, dislocation, and other. For conditions that arose from trauma, the mechanism of injury was categorised as intentional and unintentional. Intentional injury was further classified as gunshot wound, stab (use of sharp penetrating object) and assault (use of blunt object). Unintentional injuries were defined as injuries resulting from falls, road traffic accidents (motor and pedestrian) and other. Reasons for referrals to TAH from CHCs and KDH were documented as condition related or no after-hours/theatre time. Categorical data were presented as frequencies with percentages, and continuous data were checked for normal distribution and presented as medians and interquartile ranges (IQRs). The x2 test was used for categorical data The referral ratio was defined as the total number of tertiary referrals made divided by the total number of operations done by each DH.
Ethical considerations
Ethics approval was obtained from the Health Research Ethics Committee of Stellenbosch University (ref. no. N20/01/008) and the Western Cape Provincial Department of Health (ref. no. WC202006_023), which gave a waiver of patient consent. All data were deidentified prior to analysis.
Results
Orthopaedic resources and referral ratio of Cape Metro East DHs
During the study period, none of the DHs performed after-hours operations. KDH did the highest number of operations (n=2 040), referred the fewest patients to the tertiary hospital (n=364), and had a referral ratio of 0.18; in other words, KDH operated on five times as many patients as it referred. KDH also had the most orthopaedic resources, including two full-time orthopaedic surgeons, two medical officers, and four operating lists per week. In contrast, ERH had no orthopaedic human resources and no theatre time, and referred all its cases to TAH. KBH and HH each had some orthopaedic resources and had referral ratios >0.9 (Table 1).
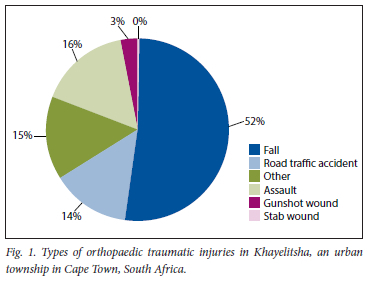
Khayelitsha community acute orthopaedic conditions
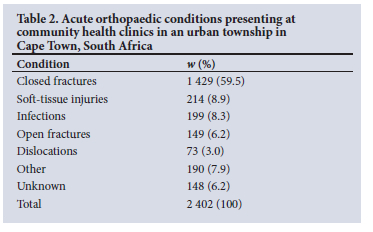
During the study period, 2 402 acute orthopaedic cases presented to 11 CHCs in Khayelitsha. The median (IQR) patient age was 32 (18 - 46) years, and 1 055 (43.9%) were female. The most common conditions were closed fractures (n=l 429; 59.5%), soft-tissue injuries (n=214; 8.9%) and infections (n=199; 8.3%) (Table 2). The most common anatomical locations of acute orthopaedic conditions were the upper extremities (n=l 045; 43.5%) and lower extremities (n=796; 33.2%), followed by the head and torso (n=92; 3.8%) and unknown referrals (n=469; 19.5%). Of the 2 402 acute orthopaedic cases, 608 (25.3%) were given advice only, 1 265 (52.7%) were sent to outpatient clinics, and 349 (14.5%) were referred for inpatient care. The referral outcome was unknown for 180 (7.5%). Trauma was the most common mechanism of injury (n=2 066; 86.0%). In the trauma category, the most common intentional injuries were those resulting from assault (n=326; 15.8%), followed by gunshot wounds (n=55; 2.7%). The most common unintentional injuries resulted from falls (n=1081; 52.3%) (Fig. 1).
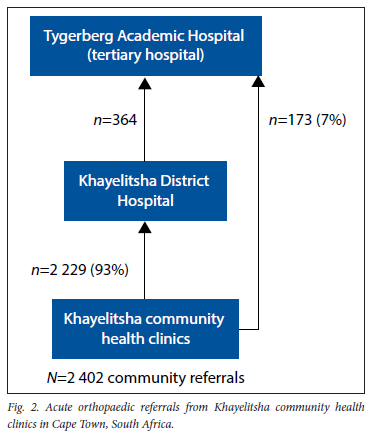
Management of acute orthopaedic conditions by KDH
The vast majority of community acute orthopaedic conditions were referred to the DH, KDH (n=2 229; 92.8%), rather than the tertiary hospital, TAH (n=173; 7.2%). Direct tertiary referrals were related to the condition (n=158; 90.8%) or lack of after-hours orthopaedic services at the district level (n=15; 9.2%). Of the 2 229 patients referred to KDH, 364 (16.3%) were subsequently referred to TAH (Fig. 2). Referrals from KDH to TAH were related to condition complexity ()1=181; 49.7%), lack of after-hours diagnostic and theatre availability ()1=146; 40.0%), or other reasons ()1=37; 10.3%). The KDH orthopaedic service performed 2 040 operations, mostly for fractures (62.4%), wound debridement (9.2%) and hand infection (8.5%) (Fig. 3); 91.3% were urgent or emergency cases.
Discussion
DHs are frontline healthcare facilities and play a critical role in the time-sensitive management of traumatic injury. Types of acute orthopaedic conditions, including traumatic fractures, that should be managed by DHs in SA and other LMICs are not well defined. This study is one of the first to describe the impact of a decentralised DH orthopaedic service in an urban township in SA.
During the study period, 84% of this urban townships ~2 000 acute traumatic orthopaedic cases were managed at the DH through 2 040 operations without referral to the tertiary hospital. This has two important benefits. Firstly, it provides orthopaedic care closer to the community, directly reducing delays to care but also delivering timely EESC. While we did not measure time to care, other studies have demonstrated DH surgical care to be more timely than transfer to tertiary hospitals.[18] Secondly, it offloads the trauma burden that would otherwise be treated at the tertiary hospital, which is often overburdened with long waiting lists for complex and elective orthopaedic operations. KDH therefore plays a massive role in releasing this bottleneck, strengthening district trauma services, and delivering definitive orthopaedic care.
Mapping of tertiary referrals showed that KDH had a lower referral ratio compared with other DHs, but more orthopaedic resources. One important contributing factor was that KDH had the most consultant orthopaedic surgeons. Most SA DHs do not have specialist surgeons and are staffed by family physicians, medical officers and community service doctors.[19] A recent SA study demonstrated that the lack of adequately trained healthcare providers at DHs contributed to delays in accessing surgical care.[20] DHs need to identify the minimum number of healthcare providers required to create core surgical teams in order to increase capacity and reduce delays at this level of care. There is a need for greater human resource capacity, particularly as the trauma burden grows while resources remain constrained and unevenly distributed.[20] Lack of dedicated operating theatre time may have also been an independent contributor to the lower operative volumes at the other three DHs compared with KDH. Other studies have found that the lack of physical and infrastructural resources at DHs, and not only lack of specialists, were crucial factors constraining surgical capabilities.[21,22] In addition, Pittalis et al.[23] found that lack of resources was the highest driver of referrals to higher-level hospitals. While KDH can be a successful decentralised model, it may not be replicable for every health district. However, increasing decentralised orthopaedic capacity would contribute to health system strengthening by decreasing the need for referral to the tertiary hospital, which then can offer more elective and complex services.
Equitable and timely access to EESC for all people in SA can only be achieved with increased decentralised surgical capacity.[13] Firstly, tertiary hospitals are usually located in urban areas far from rural communities. Secondly, the large burden of surgical disease presenting at these facilities can surpass operating capacity. If more EESC can be provided at district level, such as care for acute orthopaedic conditions, this may decrease morbidity and mortality. Also, higher-level hospitals would have greater ability to address complex and elective surgical conditions requiring surgical specialists.[24,25]
This study had several limitations. The analysis was based on secondary data that may contain missing, incomplete or conflicting information. Walk-ins, ambulance and telephone referrals were not included, so referral volume may have been underestimated. We did not report on patient outcomes or the quality of care. Finally, a specialised orthopaedic team such as the one at KDH might not be achievable at other DHs, so increasing other available resources, such as medical officers and theatre time, and adding after-hours orthopaedic services, could help address the increasing burden of traumatic injury in SA. With the COVID-19 pandemic having increased surgical backlogs in SA, decentralised and timely EESC is essential.
Conclusion
This study has shown that robust decentralised orthopaedic services at KDH increased the accessibility of EESC and alleviated the high burden of referrals to its tertiary hospital. Further research on the barriers to scaling up orthopaedic DH capacity in LMICs is needed to improve equitable access to surgical care.
Declaration. None.
Acknowledgements. The authors would like to acknowledge Vula Mobile for their assistance in data extraction, as well as the key informants at KBH and HH.
Author contributions. KC, JdT, DH and CB conceived the study. MA, SR, ML, MS and TM contributed to data collection and extraction. TM and KC contributed to the study design, analysis and interpretation of the data. TM wrote the first draft of the manuscript. TM, KC, JdT and CB critically reviewed the manuscript. All authors contributed to the review of the manuscript and approved the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries. The neglected burden in developing countries. Bull World Health Organ 2009;87(4):246. https://doi.org/10.2471/BLT.08.052290 [ Links ]
2. Mock C, Cherian MN. The global burden of musculoskeletal injuries. Challenges and solutions. Clin Orthop Relat Res 2008;166(10):2306-2316. https://doi.org/10.1007/s11999-008-0416-z [ Links ]
3. Mock C, Quansah R, Krishnan R, Arreola-Risa C, Rivara F. Strengthening the prevention and care of injuries worldwide. Lancet 2004;363(9427):2172-2179. https://doi.org/10.1016/S0140-6736(04)16510-0 [ Links ]
4. Bauhahn G, Veen H, Hoencamp R, Olim N, Tan E. Malunion of long-bone fractures in a conflict zone in the Democratic Republic of Congo. World J Surg 2017;41(9):2200-2206. https://doi.org/10.1007/S00268-017-4008-5 [ Links ]
5. Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury. Incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev 2016;22(1):13-18. https://doi.org/10.1136/injuryprev-2015-041616 [ Links ]
6. Chokotho L, Jacobsen KH, Burgess D, et al. A review of existing trauma and musculoskeletal impairment (TMSI) care capacity in East, Central, and Southern Africa. Injury 2016;47(9):1990-1995. https://doi.org/10.1016/j.injury.2015.10.036 [ Links ]
7. Chu K, Naidoo M, Klopper JH, Kloppers JC, Navsaria R Reed A. The contribution of first-level hospitals to 6 essential surgical procedures in a South African health district. A retrospective, cross-sectional study East Central Afr J Surg 2020,25(3).1-15. https://doi.org/10.4314/ecajs.v25i3.1 [ Links ]
8. Voss M, Duvenage R Operative surgery at the district hospital. S Afr Med J 2011;101(8):521-522. [ Links ]
9. Kisitu DK, Eyler LE, Kajja I, et al The role of Ugandan district hospital orthopedic units in the care of vulnerable road users. A cross-sectional study. Inj Epidemiol 2016;3(1):27-34. https://doi.org/10.1186/S40621-016-0092-5 [ Links ]
10. David BR, Gabrielle AJ. Analysis of referral appropriateness in the Western Cape, South Africa, and implications for resource allocation. Afr J Emerg Med 2012;2(2):53-58. https://doi.org/10.1016/j.afiem.2012.03.006 [ Links ]
11. Hsu EY, Schwend RM, Julia L. How many referrals to a pediatric orthopaedic hospital specialty clinic are primary care problems? J Pediatr Orthop 2012;32(7):732-736. https://doi.org/10.1097/BPO.0b013e31826994a4 [ Links ]
12. Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030. Evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386(9993):569-624. https://doi.org/10.1016/S0140-6736(15)60160-X [ Links ]
13. Price R Makasa E, Hollands M. World Health Assembly Resolution WHA68.15: 'Strengthening Emergency and Essential Surgical Care and Anesthesia as a Component of Universal Health Coverage - addressing the public health gaps arising from lack of safe, affordable and accessible surgical and anesthetic services. World J Surg 2015;39(9):2115-2125. https://doi.org/10.1007/s00268-015-3153-y [ Links ]
14. Marszalek J, de Villiers P. Morbidity profile of admissions to G F Jooste Hospital, Manenberg, Cape Town. S Afr Fam Pract 2014;(48):15-15e. https://doi.org/10.1080/20786204.2006.10873402 [ Links ]
15. Molyneaux A, Harrison A. True grit. What it takes to be a trauma physician in SA. Eyewitness News, 14 June 2016. https://ewn.co.za/2016/06/13/True-grit-working-the-weekend-shift-in-a-South-African-trauma-unit (accessed 1 March 2021). [ Links ]
16. Ahiable E, Lahri S, Bruijns S. Describing the categories of people that contribute to an emergenc centre crowd at Khayelitsha Hospital, Western Cape, South Africa. Afr J Emerg Med 2017;7(2):68-73. https://doi.org/10.1016/j.afiem.2017.04.004 [ Links ]
17. Bateman C. The smell of coffee, blood and disinfectant.... S Afr Med J 2014;104(11):727-729. https://doi.org/10.7196/SAMJ.9004 [ Links ]
18. Bentounsi Z, Sheik-Ali S, Drury G, Lavy C. Surgical care in district hospitals in sub-Saharan Africa. A scoping review. BMJ Open 2021;11(3):e042862. https://doi.org/10.1136/bmjopen-2020-042862 [ Links ]
19. Dell AJ, Gray S, Fraser R Held M, Dunn R. Orthopaedic surgeon density in South Africa. World J Surg 2018;42(12):3849-3855. https://doi.org/10.1007/s00268-018-4709-4 [ Links ]
20. Dell AJ, Klopper J. Surgical resources in South Africa. An analysis of the inequalities between the public and private sector. S Afr J Surg 2018;56(2):16-20. https://doi.org/10.17159/2078-5151/2018/v56n2a2397 [ Links ]
21. Li Z, Yang J, Wu Y, et al. Challenges for the surgical capacity building of township hospitals among the Central China. A retrospective study. Int J Equity Health 2018;17(1):55. https://doi.org/10.1186/S12939-018-0766-4 [ Links ]
22. Cheelo M, Brugha R, Bijlmakers L, Kachimba J, McCauley T, Gajewski J. Surgical capacity at district hospitals in Zambia: From 2012 to 2016. World J Surg2018;42(11):3508-3513. https://doi.org/10.1007/S00268-018-4678-7 [ Links ]
23 Pittalis C, Brugha R, Gajewski J. Surgical referral systems in low- and middle-income countries. A review ofthe evidence. PLoS ONE 2019;14(9):e0223328. https://doi.org/10.1371/journal.pone.022332? [ Links ]
24. Laing GL, Skinner DL, Bruce JL, et al. Auditing surgical service provision at a South African tertiary institution. Implications for the development of district services. S Afr J Surg 2017;55(4):31-35. [ Links ]
25. Van Straten S, Stannard C, Bulabula J, et al. A third of patients treated at a tertiary-level surgical service could be treated at a secondary-level facility. S Afr Med J 2017;107(9):788-790. https://doi.org/10.7196/SAMJ.2017.vl07i9.12090 [ Links ]
 Correspondence:
Correspondence:
K Chu
kchu@sun.ac.za
Accepted 19 September 2022
* Joint last authors














