Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.4 Pretoria abr. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i4.16505
RESEARCH
Understanding the impact of the COVID-19 pandemic on healthcare services for adults during three waves of COVID-19 infections: A South African private sector experience
N NematsweraniI; L SteenkampII; S HaneefIII; R M NaidooIV; S FonnV, VI
IMB ChB, MSc Clin Epidemiol; Strategic Risk Management and Data Science Unit, Discovery Health, Johannesburg, South Africa
IIMComm (Statistics); Strategic Risk Management and Data Science Unit, Discovery Health, Johannesburg, South Africa
IIIBSc (Hons) (Actuarial Science), PASSA; Strategic Risk Management and Data Science Unit, Discovery Health, Johannesburg, South Africa
IVMB ChB, MBA; Strategic Risk Management and Data Science Unit, Discovery Health, Johannesburg, South Africa
VMB BCh, PhD; School of Public Health, University of the Witwatersrand, Johannesburg, South Africa
VIMB BCh, PhD; School of Public Health and Community Medicine, University of Gothenburg, Sweden
ABSTRACT
BACKGROUND: Since the onset of the COVID-19 pandemic, healthcare resources have been repurposed to focus on COVID-19. Resource reallocation and restrictions to movement that affected general access to care may have inadvertently resulted in undue disruptions in the continuum of care for patients requiring non-COVID-19 healthcare services
OBJECTIVES: To describe the change in pattern of health service use in the South African (SA) private sector
METHODS: We conducted a retrospective study of a nationwide cohort of privately insured individuals. An analysis of claims data was performed for non-COVID-19 related healthcare services provided from April 2020 to December 2020 (year 1 of COVID-19) and April 2021 to December 2021 (year 2 of COVID-19) relative to the same period in 2019 prior to the COVID-19 pandemic in SA. Over and above plotting the monthly trends, we tested for statistical significance of the changes using a Wilcoxon test given the non-normality of all the outcomes
RESULTS: Between April and December 2020, relative to the same period in 2021, and also relative to the same period in 2019, we found a 31.9% (p<0.01) and a 16.6% (p<0.01) reduction in emergency room visits, respectively; a 35.9% (p<0.01) and 20.5% (p<0.01) reduction in medical hospital admissions; a 27.4% (p=0.01) and 13.0% (p=0.03) reduction in surgical hospital admissions; a 14.5% (p<0.01) and 4.1% (p=0.16) reduction in face-to-face general practitioner consultations for chronic members; a 24.9% (p=0.06) and 5.2% (p=0.54) reduction in mammography for female members; a 23.4% (p=0.03) and 10.8% (p=0.09) reduction in Pap smear screenings for female members; a 16.5% (p=0.08) and 12.1% (p=0.27) reduction in colorectal cancer registrations and an 18.2% (p=0.08) and 8.9% (p=0.07) decrease in all oncology diagnoses. Uptake of telehealth services throughout the healthcare delivery system increased by 5 708% in 2020 compared with 2019, and 36.1% for 2021 compared with 2020
CONCLUSION: A significant reduction in emergency room visits, hospital admissions and utilisation of primary care services was observed since the start of the pandemic. Further research is required to understand if there are long-term consequences of delayed care. An increase in the use of digital consultations was observed. Research on their acceptability and effectiveness may open new modalities of care, which may have cost- and time-saving benefits
COVID-19 infections were first reported on 31 December 2019 by the World Health Organization, and the disease was declared a global pandemic on 11 March 2020.[1]
As at 31 December 2021, over 280 million people globally were confirmed to have contracted the infection, with over 5.5 million deaths reported.[2] South Africa (SA) reported its first COVID-19 case on 5 March 2020, and as at 31 December 2021, over 3.5 million people had been confirmed COVID-19 positive and over 91 000 deaths recorded.[3]
Countries across the globe implemented strategies to slow the spread of the infection, including the enforcement of varying degrees of lockdowns (stay-at-home orders, movement restrictions and curfews), and only allowing essential services to continue. Delivery of healthcare services was among the essential services allowed to operate even during the strictest lockdowns.[4]
Healthcare systems re-organised. Elective (planned) surgeries, considered less urgent, were paused to create the needed capacity in the healthcare delivery system for the management of COVID-19 cases, particularly during the peaks of the repeated waves of the pandemic. In-hospital patient admissions reduction was significant, and extended universally across geographic regions.[5-9]
Fear of exposure to infection when accessing care at healthcare facilities resulted in patients avoiding healthcare providers. This fear was reported to be as high as 37% in the SA National Income Dynamics Study (NIDS) - Coronavirus Rapid Mobile Survey (CRAM).[10]
This paper describes the impact of the COVID-19 pandemic on non-COVID-19-related healthcare services utilisation for an adult population, as observed in the Discovery Health Medical Scheme (DHMS) data. DHMS is the largest open medical plan in SA, covering approximately 2.8 million beneficiaries.
DHMS members diagnosed with chronic conditions may register on the Chronic Illness Benefit (CIB), while those who are diagnosed with cancer may enrol on the oncology programme. Registration for CIB is initiated by the member and their treating clinicians, and must meet the scheme's defined set of clinical entry criteria. The list of chronic conditions that form part of the CIB includes those that appear on the Council for Medical Schemes' Chronic Disease List (CDL).[n Disease management benefits for chronic diseases and oncology provide members with access to specific procedures, pathology and radiology services, medication and health professional consultations.'121 DHMS cancer-screening benefits include those for breast, cervical and colorectal cancers. These screening benefits are made available to eligible members, typically defined by age groups.
Service providers that deliver care to members registered on these programmes submit medical claims that allow the scheme to pay for the services rendered. DHMS is administered by Discovery Health, which has consented to access to demographic, claims and disease registration data, and is able to triangulate between different data categories to derive meaningful insights.
Similarly, when members are admitted to hospital, all claims pertaining to clinical services rendered are submitted to Discovery Health for payment. These include ward and theatre fees, medications, pathology and radiology, and relevant health professional fees.
Research objectives and methods
Study design
This is a retrospective descriptive study with statistical validation from a Wilcoxon test for significance, in which claims data for all adult DHMS members were analysed to evaluate and quantify the impact of the COVID-19 pandemic on the utilisation of non-COVID-19-related private healthcare services in SA. Ethics approval was not required as consent to use anonymised aggregated claims and administrative data for research purposes is obtained from all scheme members as part of the scheme membership process.[13]
Study objectives
To describe the pattern of utilisation of non-COVID-19-related services in three categories, namely, hospital utilisation (as measured by emergency room (ER) visits and general hospital admissions for medical and surgical purposes separately), primary care utilisation (as measured by out-of-hospital general practitioner (GP) visits for the DHMS scheme population who are registered as patients receiving care for chronic conditions and uptake of virtual consultations) and the trends in uptake of preventive screening (specifically focusing on oncology screenings and subsequent oncology registrations).
Setting
This study was conducted using anonymised DHMS members' data, which includes demographic and claims information, as well as data pertaining to those registered for chronic illness benefits, and the oncology programmes.
Study cohort
The study includes all adult members on DHMS at any point between 1 January 2019 and 31 December 2021.
Study definitions
Members who were identified in the data as having chronic conditions were those registered on the CIB.
ER visits were identified through claims and billing information. ER doctors bill a combination of a consultation code and an emergency code that distinguishes a typical out-of-hospital GP visit from an ER visit. Furthermore, there are additional tariff codes that relate directly to ERs, e.g. hospital facility fees, ward stock or pharmacy codes that are solely billed by emergency departments. A visit to the emergency department is defined as a unique patient-doctor interaction on a particular service date.
The definition of a facility admission included admissions to private hospitals, day clinics, rehabilitation centres and psychiatric hospitals.
Case mix is defined as a measure of the average severity of hospital admissions, considering both the mix of admissions (e.g. a heart transplant v. a pneumonia admission) and the complexity of the admission (e.g. a pneumonia admission for a patient with HIV v. a pneumonia patient without HIV). Case mix indices are lower for people with fewer concomitant health problems and for people with admissions that require less complicated care.
Preventive screening tests for cancer include mammograms and Pap smears.
Colorectal cancer registrations are recorded as the number of diagnosed colorectal cases enrolled on the oncology programme.
Statistical analysis
All statistical analyses were performed in R v4.1.2 (R Foundation for Statistical Computing, Austria).
We present trends in utilisation comparing the time periods: hospital utilisation (as measured by ER visits and general hospital admissions for medical and surgical purposes separately), primary care utilisation (out-of-hospital GP visits for a population registered for chronic care and uptake of virtual consultations) and the trends in uptake of preventive screening (specifically focusing on oncology screening and subsequent oncology registration). We compare utilisation for the months of April - December 2020 (year 1 of COVID-19) relative to April - December 2019 (pre-COVID-19), and April - December 2021 (year 2 of COVID-19) relative to April - December 2019 (pre-COVID-19) and test for statistically significant differences using the Wilcoxon signed-rank test, after the Shapiro-Wilk test indicated that non-parametric analytical approaches were appropriate. The level of significance was set at p<0.05.
Analysis of hospital admissions considered both the level of acuity of hospital admissions over the duration of the pandemic, and changes in admissions to hospital facilities. The split of admissions by medical v. surgical is also described.
Results
Key demographics are shown in Table 1.
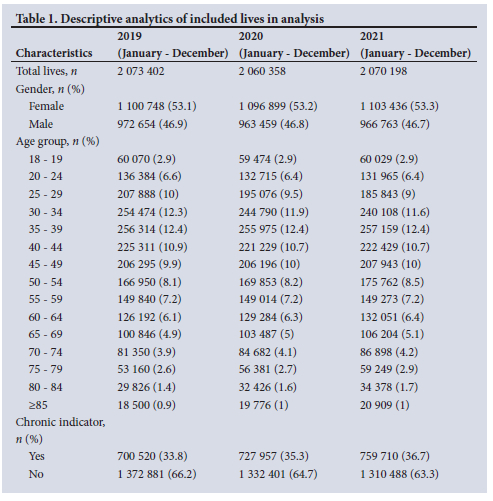
The number of adult members decreased from 2.073 million in 2019 to 2.070 million in 2021. There are more women (53.3%) than men in the scheme, and the percentage of members registered with a chronic illness increased from 33.8% in 2019 to 36.7% in 2021. The demographic profile in terms of age and sex of members remained relatively stable over the period, with the average age increasing from 44.3 in 2019 to 45.1 in 2021.
Emergency room visits
Visits to the ER are generally an indication of immediate care sought to relieve an acute condition or to manage a clinical emergency. DHMS data (Fig. 1) revealed a 31.9% (p<0.01) reduction in ER volumes for April - December 2020 when compared with April - December 2019, and a reduction of 16.6% (p<0.01 ) in ER volumes for April - December 2021 when compared with April - December 2019. The greatest drop was observed during the strictest lockdown level in April 2020. The reduction in ER visits, relative to 2019 (pre-pandemic levels), was sustained until the third wave in July - August 2021.
Hospital admissions
Total hospital admissions decreased during the pandemic, with the deepest drop of 62% observed during the month of April 2020.
compared with April 2019, which coincides with the strictest lockdown level. Admission rates (include for both COVID-19 and non-COVID-19) increased after lockdown restrictions eased; however, they remained low relative to pre-COVID-19 levels in 2019. As of April - December 2021, admission rates were 18.2% lower when compared with the same period in 2019.
Fig. 2 shows a reduction in hospital admissions in 2020 for both medical and surgical admissions, with a 72.3% reduction in surgical admission rate and a 58.2% reduction in medical admission rate during the strictest lockdown level in April 2020. COVID-19 admissions were at 0.5% of the total admissions during this time. Fig. 3 depicts an increase in COVID-19-related admissions as a proportion of total admissions at the peaks of the COVID-19 infections, recorded at 11.3% in July 2020 and 17.8% in January 2021, with the highest proportion of 20.9% recorded in July 2021.
Medical and surgical admissions during April - December 2020 were 35.9% (p<0.01) and 27.4% (p<0.01) lower, respectively compared with the same period in 2019, whereas medical and surgical admissions during April - December 2021 were 20.5% (p=0.01) and 13.0% (p=0.03) lower, respectively, compared with the same period in 2019.
The case mix for all hospital admissions (which includes COVID-19 and non-COVID-19 admissions), as shown in Fig. 4, increased significantly since the start of the pandemic, indicating that sicker COVID-19 and non-COVID-19 patients were being admitted. The average case mix of 1.32 for April - December 2020 was 12.6% (p<0.01) higher than the corresponding period in 2019, and this elevated case mix level has persisted into 2021, with an even bigger differential of 13.5% (p<0.01).
Doctor visits out of hospital
A 14.5% (p<0.01) reduction in GP consults per 1 000 chronic lives was observed from April to December 2020, as illustrated in Fig. 5. Consultations increased again in 2021, and rates are almost back in line with pre-pandemic trends, with utilisation at only 4.3% (p=0.16) lower for 2021 April - December than the corresponding 2019 levels. The reduction in consultations also extended to specialists including gynaecologists and psychiatrists.
Fig. 6 shows the virtual consultation utilisation trend pre-COVID-19 compared with during the pandemic. The highest utilisation rates coincided with the surge in infections during the various COVID-19 waves. CPs accounted for the highest number of the virtual consults, followed by radiotherapists and general physicians.
Oncology registrations and screening
A non-statistically significant 18.2% (p=0.08) decline in registrations for all cancer care was observed, from around 730 registrations per month prior to the pandemic to around 600 per month between April and December 2020. The steepest decline in registrations was seen in the month of April, with only 374 new registrations recorded. This is illustrated in Fig. 7. The rate of registrations increased in early 2021 after the second wave of infections, but declined once again at the onset of the third wave and remained low when compared with previous years.
The observed decrease in oncology registrations in 2020 occurred in a period where the data indicate a reduction in the number of some of the cancer-screening events recorded during this time. Mammography screenings per 1 000 female lives decreased by 24.9% (p=0.06) between April and December 2020, with partial recovery in 2021 to 5.2% (p=0.54) lower than pre-COVID-19 levels (Fig. 8). A 23.4% (p = 0.03) decrease in Pap smear visits per 1 000 female lives was observed from April to December 2020 relative to the same period in 2019 (Fig. 9). This trend persisted into 2021, with a 10.8% (p=0.09) reduction in visits compared with 2019. Fig. 10 depicts a 16.5% (p=0.08) and 12.1% (p=0.27) reduction in colorectal cancer registrations during this period.
Discussion
Various local and global publications have reported on the impact of the pandemic on healthcare utilisation. Publications that include SA data have reported on the impact of the pandemic on surgical admissions, all-cause admissions and primary care services, limiting the reporting to 2020 public sector data, mainly focusing on the first wave of COVID-19 in SA.[5-9,14-24] The present article offers a broader view of the data and incorporates the impact on both in- and out-of-hospital care and on primary care services from April 2020 to December 2021, covering three COVID-19 waves of infection (ancestral, beta and delta). It is also the first article to report on private sector utilisation trends during the pandemic.
Due to differing healthcare demands and access between public and private sectors in SA, it is important to report on the impact observed in the private sector during this period.
During the study period, certain high-volume hospitals closed due to infections, and movement was strictly regulated, both of which could have contributed to the observed reduction in ER visits. Given that ER visits often generate hospital admissions, a reduction in overall ER visits corresponds with the reduction in overall hospital admissions. We have not investigated whether this was mainly owing to a decrease in trauma admissions, but globally, there was a very significant decrease in motor vehicle accidents during the COVID-19 pandemic.[25]
The overall admission rates in 2020 and 2021 were down compared with 2019. Nonetheless, -80% of admissions were for non-COVID-19 care, and these were recorded during the highest peak of COVID-19 infections, indicating that some degree of care was still available. The patterns of medical and surgical admissions were roughly similar, but during the pandemic the case mix index was higher, reflecting the degree to which people admitted for COVID-19 and non-COVID-19 illnesses had concomitant chronic disease or severe illness. This implies that hospitalisation was appropriately apportioned for people who are less healthy. The impact was most felt during the first wave of COVID-19 in SA when the lockdown was at it strictest and non-urgent and elective care was curtailed. Hospitalisations did increase after that, but not to the same level as the pre-COVID-19 period. Hospital groups started to reopen their theatre facilities to a select list of elective procedures in May 2020, which explains the quicker recovery of surgical admissions relative to medical admissions. There may be risks associated with this delayed care, such as non-urgent care becoming urgent or complicated,[14] and this warrants ongoing research.
The reduction in hospital admissions could have some positive implications for the private sector, a predominantly fee-for-service environment where it is generally accepted that wasteful care (too much service or the wrong kind of services) is prevalent.[26] Inappropriate care also relates to minor conditions that are often self-limiting but are managed at higher acuity settings at higher costs than are clinically required. It is widely accepted that acute delivery capacity in certain regions outstrips demand, for example, general hospitals built in areas where the need is not present. Patients who would traditionally have been admitted to hospital for these low-acuity conditions are vulnerable to exposure to harmful hospital-acquired pathogens, thereby worsening clinical outcomes. Therefore, rationing access for low-acuity conditions, as observed during the pandemic, may have a positive effect by resetting utilisation to more appropriate levels, thereby eliminating waste and enabling constrained resources to be used more appropriately.
A SA publication by Pillay et al.[18]that reported on the impact of COVID-19 on routine primary healthcare services between March 2020 and December 2020 focused on primary healthcare visits, family planning, maternal and child care, HIV and TB testing, and did not report on in-hospital utilisation trends.
Primary care visits to CPs were significantly reduced during the pandemic, especially during the period of April - December 2020, similar to what was observed in primary healthcare facilities in the public sector. This is a concerning trend as it may indicate deferred care, which may result in complicated disease presentations later on. However, the opportunity exists to reset the primary care base to meet individual patient needs, to co-ordinate care across the entire primary care field, and to involve the patient in decision-making.
Oncology services
Pillay et al.[18] did not report on the impact of the pandemic on oncology screening services for patients accessing care in the public sector.
For the most prevalent cancers in this population (breast, cervical and colorectal), screening benefits are widely available tor privately insured patients.[11] A drop in screening claims at the start of the pandemic for cervical and breast cancers and a reduction in colorectal cancer registrations have been observed. In 2021, however, there appears to have been an improvement approaching pre-pandemic levels for cervical and breast cancer screening. While the drop shows no statistical significance for breast cancer screening, this concerning trend has been reported in other countries such as the UK, where their recorded pre-COVID-19 screening rates were previously at >70% uptake for eligible population groups.[27]
In the SA private sector, results from the Health Quality Assessment (HQA) show that the screening rates were significantly low, at just >40% for cervical cancer and <30% for breast cancer in the pre-COVID-19 period.[31] The decrease in screening is therefore coming off an already low base. A non-statistically significant reduction in colorectal cancer registrations was observed during this time, which may indicate a reduction in screenings during this period.
Colorectal cancer has the least mature screening programme, as it was only introduced in 2019 for DHMS members.
The long-term impact of this is not clear but should be monitored. Of concern is the drop in the number of people who registered for oncology benefits overall. If this reflects undiagnosed cancer that manifests in later-stage disease at diagnosis, it will have a negative impact on health outcomes.[19,20,22,24] Late-stage breast cancer at time of diagnosis is associated with poorer 5-year survival rates, at 28%, compared with 100% for women with localised tumours.[22,23,28] For cervical cancer, the 5-year survival rate for women diagnosed at an advanced stage is 17%, compared with 92% if diagnosed when the cancer has not spread.[29] Colorectal cancer, if diagnosed at an early stage before it has spread, has a 5-year relative survival rate of -91%. When the cancer has spread outside of the colon or rectum, survival rates are much lower, at 14%.[24,30] Our data suggest that protecting preventive oncology services during a pandemic is advisable. It is likely that this is true for treatment and palliation, but we have not investigated our data for these impacts yet.
Study limitations
The data are mainly descriptive and generated from medical insurance claims data, implying some selection bias based on affordability, and they may not be generalisable to the broader SA population. It is possible in our analysis that some people with a chronic disease may have been allocated to the wrong category, and that some people who have chronic conditions may not have been registered on the CIB.
Conclusion
A significant reduction in ER visits, hospital admissions and the utilisation of primary care services has been observed since the start of the COVID-19 pandemic. This may have long-term detrimental effects on clinical outcomes. Even in pandemic situations it seems reasonable to recommend that preventive care and screening for cancer be sustained.
These findings raise important questions for future research, which DHMS data would allow us to answer. These include the impact of delayed surgery on health outcomes: does delay in this instance lead to worse outcomes?
Has the health status of people registered on chronic care deteriorated or stayed the same? This will allow us to assess the degree to which patients receive enough guidance from their providers to self-manage. It may also allow some decisions to be made about how often a health worker visit is required, or perhaps indicate markers of high-risk patients.
It is essential to understand the consequences of delayed cancer diagnosis, and further data analysis to try to answer this question is important. Knowing an answer to this would allow better planning for future epidemics, for example, ensuring safe access to oncology services. This also raises the question of introducing self-sampling for cervical cancer screening, which has been shown to be effective and may yield savings for members if self-sampling is effective and the health outcomes are the same.
The importance of this article lies not only in presenting the findings themselves, but also in making clear the kind of future research required to improve health outcomes and efficiency and effectiveness in healthcare provision.
The pandemic has presented both opportunities and challenges in the delivery of non-COVID-19 healthcare services. This means that as stakeholders in the healthcare system, we should look at ways of leveraging these opportunities while also finding innovative ways of addressing the challenges.
Important opportunities that the pandemic has presented are the following:
Scaling digital health: global and local trends already show increased uptake of digital health during this pandemic period, creating an opportunity to firmly embed these trends in the healthcare system.
The burden of change management, a significant hindrance to digital adoption prior to the pandemic, was eased dramatically during the pandemic, when the urgent need to re-engineer practices outweighed the pressure to preserve traditional models of delivering care services. Providers therefore will emerge from the pandemic familiar with the operationalisation and value of digital innovations. There is a need to recognise this opportunity to strengthen digital adoption and address variances in access to digital health, including age, geography and socioeconomic status.
Digital tools need to take into consideration patient and doctor preferences, and must be tailored to improve both the patient and provider care experience.
It is important to establish a regulatory framework that enables access to these tools but still safeguards patient confidentiality and safety.
Private funders must ensure that sustainable funding models are designed and implemented to enable rapid scaling of these tools.
Reporting on the impact of digital tools on clinical outcomes is critical for continued improvement in care delivery.
Shifting care from hospital to outpatient settings, including the home environment: this includes a move towards a higher utilisation of day-care facilities and doctor's rooms for elective and non-complex procedures and the management of low-acuity medical admissions in the out-of-hospital setting. This will significantly drive down healthcare costs relating to in-hospital care. It is likely that care at home will continue to grow, resulting in a shift to home admissions as remote monitoring technologies advance and patients grow accustomed to the convenience of care at home.[33,34]
Providers and patients must continue to see value in this shift for it to be sustained at scale.
Raising awareness of available oncology screening programmes to improve uptake: this requires active commitment from primary care clinicians in driving uptake.
Patient education highlighting the benefits of screening is critical.
Optimisation of available patient and provider incentives needs to be further explored.
Easy access to screening, through mobile screening units, routine screening invitations or seamless booking systems, should be investigated.
The challenges the pandemic has presented include: Deferred care: this may result in more complex clinical presentations that will be associated with higher morbidity and mortality and higher healthcare costs. Longitudinal research needs to be conducted to assess whether deferred care resulted in poorer outcomes. If so, offering virtual care and homecare services and prioritisation of screening and diagnostic services for oncology and other chronic illnesses is warranted.
Research to assess the impact of delayed care is urgently required COVID-19 vaccinations and effective therapeutics provide hope for a return to a new era where the focus can be on reversing the negative impact of the pandemic while entrenching positive healthcare shifts.
Declaration. None.
Acknowledgements. None.
Author contributions. NN conceived the format of the article. NN, RMN and LS drafted the initial manuscript. LS and SH led the actuarial and statistical analysis and provided the tables and figures. SF contributed to essential revisions of the manuscript. All authors reviewed the manuscript and gave final approval.
Funding. None.
Conflicts of interest. None. NN, LS, SH, RMN are all employed by Discovery Health.
References
1. World Health Organization. Rolling updates on coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed 12 October 2021). [ Links ]
2. Coronavirus Statistics. Worldometer, 2022. https://www.worldometers.info/coronavirus/ (accessed 12 October 2022). [ Links ]
3. COVID-19 South African Coronavirus new and information portal. https://sacoronavirus.co.za/ (accessed 12 October 2022). [ Links ]
4. Haider N, Osman AY, Gadzekpo A, et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Global Health 2020;5:e003319. https://doi.org/10.1136/bmjgh-2020-003319 [ Links ]
5. Moustakis J, Piperidis AA, Ogunrombi AB. The effect of COVID-19 on essential surgical admissions in South Africa. A retrospective observational analysis of admissions before and during lockdown at a tertiary healthcare complex. S Afr Med J 2020;110(9):910-915. https://doi.org/10.7196/samj.2020.v110i9.15025 [ Links ]
6. O'Conneli RM, Khan MA, Amir M, et al. The impact of COVID-19 on emergency general surgery admissions and operative volumes. A single centre experience. Surgeon 2020;S1479-666X(20):30168-2. https://doi.org/10.1016/j.surge.2020.09.013 [ Links ]
7. Mcintosh A, Bachmann M, Siedner MJ, et al. Effect of COVID-19 lockdown on hospital admissions and mortality in rural KwaZulu-Natal, South Africa. Interrupted time series analysis. BMJ Open 2021;11:e047961. https://doi.org/10.1136/bmjopen-2020-047961 [ Links ]
8. Pikoulis E, Koliakos N, Papaconstantinou D, et al. The effect of the COVID pandemic lockdown measures on surgical emergencies. Experience and lessons learned from a Greek tertiary hospital World J EmergSurg 2021;16(22):22 https://doi.org/10.1186/s13017-021-00364-1 [ Links ]
9. Levy JF, Wang KY, Ippolito BN, Ficke JR, Jain A. The impact of the COVID-19 pandemic on elective inpatient surgical admissions. Evidence from Maryland. J Surg Res 2021;268:389-393. https://doi.org/10.1016/j.jss.2021.07.013 [ Links ]
10. Spauli N, Ardington C, Bassier I, et aL NIDS-CRAM wave 1 synthesis report. Overview and findings. https://cramsurvey.org/reports/ (accessed 24 February 2023). [ Links ]
11. Council for Medical Schemes. Prescribed Minimum Benefits. CMS, 2021. https://www.medicalschemes.co.za/resources/pmb/ (accessed 1 December 2021). [ Links ]
12. Screening and Prevention Benefit, Discovery Health Medical Scheme 2022. https://www.discovery.co.za/wcm/discoverycoza/assets/medical-aid/benefit-information/2022/screening-and-prevention-benefit (accessed 6 November 2022). [ Links ]
13. Discovery Health Medical Scheme. Applying to become a member of Discovery Health Medical Scheme in 2022 https://www.discovery.co.za/wcm/discoverycoza/assets/medical-aid/benefit-information/2022/applying-to-become-a-member-of-the-dhms.pdf (accessed 12 January 2022) [ Links ]
14. Choi JY, Park IJ, Lee HG, et al. Impact of the COVID-19 pandemic on surgical treatment. Patterns for colorectal cancer in a tertiary medical facility in Korea. Cancers 2021;13:2221. https://doi.org/10.3390/cancers13092221 [ Links ]
15. Chang AY, Cullen MR, Harrington RA, Barry M. The impact of novel coronavirus COVID-19 on non-communicable disease patients and health systems. A review. J Intern Med 2021;289(4):450-462. https://doi.org/10.1111/joim.13184 [ Links ]
16. Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases. A global survey of views from healthcare professionals. Diabetes Metab Syndr 2020;14(5):965-967. https://doi.org/10.1016/j.dsx.2020.06.042 [ Links ]
17. Nikoloski Z, Alqunaibet AM, Alfawaz RA, et al. COVID-19 and non-communicable diseases. Evidence from a systematic literature review. BMC Public Health 2021;21:1068. https://doi.org/10.1186/sl2889-021-11116-w [ Links ]
18. Pillay Y, Pienaar S, Barron P, et al. Impact of COVID-19 on routine primary healthcare services in South Africa. S Afr Med J 2021;111(8):714-719. https://doi.org/10.7196/SAMJ.2021.v111i8.15786. [ Links ]
19. Jones D, Neal RD, Duffy S, et al. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer. The view from primary care. Lancet Oncology 2020;21(6):748-750. https://doi.org/10.1016/S1470-2045(20)30242-4 [ Links ]
20. Part D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care. How the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform 2020;4:1059-1071. https://doi.org/10.1200/CCI.20.00134 [ Links ]
21. Reynolds, R Dennis S, Hasan I, et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 2018;19:11. https://doi.org/10.1186/sl2875-017-0692-3 [ Links ]
22. Caplan L. Delay in breast cancer. Implications for stage at diagnosis and survival. Front Public Health 2014;2:87. https://doi.org/10.3389/fpubh.2014.00087 [ Links ]
23. Freer PE. The impact of the COVTD-19 pandemic on breast imaging. Radiol Clin North Am 2021;59(1):1-11.https://doi.org/10.1016/j.rcL2020.09.008 [ Links ]
24. Del Vecchio Blanco G, Calabrese E, Biancone L, Monteleone G, Paoluzi OA. The impact of COVID-19 pandemic in the colorectal cancer prevention. Int J Colorectal Dis 2020:35(10);1951-1954. https://doi.org/10.1007/S00384-020-03635-6 [ Links ]
25. YasinYJ, Grivna M, Abu-Zidan FM. Global impact of COVID-19 pandemic on road traffic collisions. World J Emerg Surg2021;16:51. https://doi.org/10.1186/sl3017-021-00395-8 [ Links ]
26. Ngcobo S, Form S, Bhengu N, et al. Health Market Inquiry. Final findings and report. Pretoria. Competition Commission of South Africa. 2019. http://www.compcom.co.za/wp-content/uploads/2014/09/Health-Market-Inquiry-Report.pdf (accessed 12 October 2022). [ Links ]
27. Nuffield Trust. Cancer Screening, https://www.nuffieldtrustorg.uk/resource/breast-and-cervical-cancer-screening (accessed 12 October 2022). [ Links ]
28. American Cancer Society. Survival Rates for Breast Cancer. https://www.caneer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html (accessed 6 November 2021). [ Links ]
29. American Cancer Society. Survival Rates for Cervical Cancer. https://www.cancer.org/cancer/cervical-cancer/detection-diagnosis-staging/survival.html (accessed 6 November 2021). [ Links ]
30. American Cancer Society. Survival Rates for Colorectal Cancer. https://www.cancer.org/cancer/colon-rectal-cancer/detection-dia gnosis-staging/survival-rates.html (accessed 6 November 2021). [ Links ]
31. Health Quality Assessment reports. https://www.hqareports.com/app/ (accessed 12 October 2022). [ Links ]
32. Lozar T, Nagvekar R, Rohrer C, et al. Cervical cancer screening postpandemic. Self-sampling opportunities to accelerate the elimination of cervical cancer. Int J Womens Health 2021;13:841-859. https://doi.org/10.2147/IJWH.S288376 [ Links ]
33. Leong MQ, Lim CW, Lai YF. Comparison of hospital at-home models. A systematic review of reviews. BMJ Open 2021;ll:e043285. https://doi.org/10.1136/bmjopen-2020-043285 [ Links ]
34. Arsenault-Lapierre G, Henein M, Gaid D, et al. Hospital-at-h ome interventions vs in-hospital stay for patients with chronic disease who present to the emergency department A systematic review and metaanalysis. JAMA Netw Open 2021;4(6):e2111568. https://doi.org/10.1001/jamanetworkopen.2021.11568 [ Links ]
 Correspondence:
Correspondence:
N Nematswerani
noluthandon@discovery.co.za
Accepted 1 November 2022














