Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.4 Pretoria abr. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i4.313
RESEARCH
The state of kidney replacement therapy in Eastern Cape Province, South Africa: A call to action
L Mtingi-NkonzombiI, II; K ManningIII; T du ToitIV; E MullerV; A D ReddVI, VII, VIII; R FreercksIX, X
IMB ChB, IMVACC; Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIMB ChB, IMVACC; Department of Internal Medicine, Faculty of Health Sciences, Walter Sisulu University and Nelson Mandela Academic Hospital, Mthatha., South Africa
IIIMSc (Med); Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IVMB ChB, MMed (Surg); Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VMD, PhD; Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIBSc, PhD; Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, Md., USA
VIIBSc, PhD; Department of Medicine, School of Medicine, Johns Hopkins University, Baltimore, Md., USA
VIIIBSc, PhD; Institute of Infectious Disease and Molecular Medicine, University of Cape Town, South Africa
IXMB ChB, MPhil (Int Med); Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
XMB ChB, MPhil (Int Med); Department of Medicine, Faculty of Health Sciences, Nelson Mandela University and Livingstone Hospital, Gqeberha, South Africa
ABSTRACT
BACKGROUND: South Africa (SA) is one of the most financially unequal countries in the world. This situation is highlighted by disparate access to healthcare, particularly provision of kidney replacement therapy (KRT). Unlike the private sector, public sector access to KRT is highly rationed, and patient selection is based on suitability for transplantation and capacity
OBJECTIVES: To investigate the state of the KRT service in Eastern Cape Province, SA, by analysing access to and provision of KRT in the province for individuals with end-stage kidney disease, as well as disparities between the private and public healthcare systems
METHODS: This was a retrospective descriptive study to examine KRT provision and temporal trends in the Eastern Cape. Data were obtained from the South African Renal Registry and the National Transplant Waiting List. KRT provision was compared between the three main referral centres, in Gqeberha (formerly Port Elizabeth), East London and Mthatha, and between the private and public healthcare systems
RESULTS: There were 978 patients receiving KRT in the Eastern Cape, with an overall treatment rate of 146 per million population (pmp). The treatment rate for the private sector was 1 435 pmp, compared with 49 pmp in the public sector. Patients treated in the private sector were older at initiation of KRT (52 v. 34 years), and more likely to be male, to be HIV positive, and to receive haemodialysis as their KRT modality. Peritoneal dialysis was more commonly used in Gqeberha and East London as the first and subsequent KRT modality, compared with Mthatha. There were no patients from Mthatha on the transplant waiting list. There were no waitlisted HIV-positive patients in the public sector in East London, compared with 16% of the public sector patients in Gqeberha. The kidney transplant prevalence rate was 58 pmp in the private sector and 19 pmp in the public sector, with a combined prevalence of 22 pmp, constituting 14.9% of all patients on KRT. We estimated the shortfall of KRT provision in the public sector to be ~ 8 606 patients
CONCLUSION: Patients in the private sector were 29 times more likely to access KRT than their public sector counterparts, who were on average 18 years younger at initiation of KRT, probably reflecting selection bias in an overburdened public health system. Transplantation rates were low in both sectors, and lowest in Mthatha. A large public sector KRT provision gap exists in the Eastern Cape and needs to be addressed urgently
The burden of end-stage kidney disease (ESKD) continues to increase worldwide. The prevalence of chronic kidney disease (CKD) in South Africa (SA) is estimated to range from 6% to 17%[1-3] and is predicted to worsen in the future, for several reasons.[4-7] Despite being considered an upper middle-income country,[8] SA is ranked as the most unequal country in the world, with a Gini index of 63.[9] The country also has a dual burden of non-communicable diseases, including hypertension and diabetes mellitus, and communicable diseases such as HIV, that are risk factors for CKD.[5,10] Poor infrastructure, absence of screening and prevention programmes for kidney disease and the recent COVID-19 pandemic are systemic factors that further accentuate this risk.[11,12]
In SA, CKD is often diagnosed at an advanced stage, when kidney replacement therapy (KRT) (dialysis and/or kidney transplantation) is essential to maintain life.[13] Kidney transplantation is widely recognised as the best KRT for ESKD in terms of both health metrics and cost-effectiveness.[14-16] However, there are many challenges to KRT provision. Owing to the high costs involved, low- and middle-income countries that are able to institute KRT programmes often have to ration the provision of treatment, sometimes resulting in inequitable allocation. [16,17] In SA, selection for KRT is based on suitability for kidney transplantation.[12,18-21] The country uses guidelines aimed at achieving equitable access to KRT, yet different regions of the country have adapted local variants of this rationing policy that reflect local resource constraints and disparate access to healthcare.[22,23] Only 14.8% of SAs population have health insurance that provides access to the private sector where the provision of KRT is mandated by law[19] This leaves the majority (85.2%) of South Africans reliant on the public sector healthcare system, and for those with ESKD, limited access to rationed KRT[24] In 2020, according to the South African Renal Registry (SARR), the prevalence rate for the provision of KRT was 729 per million population (pmp) in the private sector compared with 44 pmp in the public sector, which is lower than the 70 pmp reported in 1994.[25] While an exact comparison may not be accurate, the private sector KRT rate could be used as a surrogate marker for the true required KRT burden in the public sector. Overall, the national kidney transplant rate in SA is low at 4.6 pmp, compared with 38.1 for European Union member states reported in 2016.[26]
Inequalities in KRT provision in SA exist within and between provinces. Eastern Cape Province is ranked as the most unequal province in SA.[27] The province has the highest prevalence of HIV infection, ranging between 28% and 34%,[28] and suffers a critical shortage of medical specialists. According to a survey conducted in 2018, there were only six nephrologists in the province (density of 0.6 pmp), while in the neighbouring Western Cape Province there were 37 nephrologists and a corresponding density of 6 pmp, highlighting the disparity between provinces.[29] Three cities in the Eastern Cape have public tertiary healthcare facilities, which service an area of 168 966 km2 with a population of 6 676 590 people.[8] Only 7% of the provinces population have private healthcare insurance.[24] Furthermore, the Eastern Cape has only three public sector facilities that provide dialysis and pre- and postoperative support for kidney transplant recipients, viz. Gqeberha, formerly Port Elizabeth (western region), East London (central region) and Mthatha (eastern region). For kidney transplantation, waitlisted patients must travel large distances (~1 000 km) to quaternary transplant centres in the Western Cape.
This study aimed to investigate the state of the KRT service platform in the Eastern Cape by analysing access to and provision of KRT in the province for individuals with ESKD, as well as the disparities between the private and public healthcare systems. The results of this study will be used as a foundation to facilitate the investigation of potential barriers to KRT and the initiation of appropriate solutions in the province.
Methods
The study was a cross-sectional study examining the current KRT provision and retrospectively reviewing temporal trends in the Eastern Cape from 2012 to 2020. The University of Cape Town Human Research Ethics committee (HREC) granted permission for this study (ref. no. HREC 401/2022). Current and retrospective data on KRT provision were obtained from the SARR on 3 August 2022.[30] The SARR collects data on all patients in SA with ESKD who are treated with KRT at public and private facilities providing KRT that are registered with the SARR. Facilities submit data to the registry upon registration and then annually, to provide follow-up information during the month of December each year. The following data on adults and children are included in the registry and were obtained and analysed in this study: baseline demographic data including age and gender, number of years on dialysis, first and current modality of KRT, HIV status, transplants received, province of residence, treatment facility, and date of initiation of KRT. The current point prevalence of patients on the kidney transplant waiting list was described according to data extracted from the National Transplant Waiting List maintained by the Organ Donor Foundation.
Aggregated data for both private and public sector patients were collated according to the drainage areas of the three tertiary centres that provide KRT and compared. Patients who had died or who were no longer receiving KRT (either withdrew from dialysis or kidney function was regained) at the time of the study were excluded from the analysis.
The estimated prevalence of KRT was determined using the denominators for public and private facilities according to mid-year
population estimates from Statistics South Africa (Stats SA) for 2021[8] and the Council for Medical Schemes 2020/2021 report,[24] respectively. These are presented as a pmp rate of KRT provision as per the methodology in previous SARR reports.[25] The shortfall in KRT provision was calculated as the product of the public sector population in millions and the difference between the public and private sector KRT provision rate. The number of practising nephrologists in the province was defined as per Hassen et aL.,[29] and data in this regard were collected online as at 3 August 2022 from the Health Professions Council of South Africa and the South African Nephrology Society database, as well as from personal knowledge and contacts.
Statistical analysis
Descriptive statistics and temporal trends were used to summarise data on age, gender, KRT modality and HIV status. Variables were summarised using means with standard deviations (SDs) or medians with interquartile ranges, as appropriate. Categorical variables are presented as frequencies and percentages. Comparison between the public and private sectors was performed using the Wilcoxon rank-sum test for continuous variables and the x2 test or Fisher's exact test for comparison of categorical data, as appropriate. Analysis was performed in Stata 16.1 (StataCorp, USA).
Results
As of 3 August 2022, there were 978 patients receiving KRT in the Eastern Cape, with an overall treatment rate of 146 pmp. There were 50 patients in the provincial data whom we were unable to assign to a specific treatment centre owing to missing data. The treatment rate for the private sector was 1 435 pmp, compared with 49 pmp in the public sector. The predicted shortfall in public sector KRT provision was 8 606 patients. The demographics of patients receiving KRT in the province for both sectors are shown in Table 1. Patients treated in the private sector were older and more likely to be male, to be HIV positive and to receive haemodialysis as their KRT modality. The number of people with a functioning kidney transplant was 58 pmp in the private sector and 19 pmp in the public sector, with a combined prevalence of 22 pmp constituting 15% of all patients on KRT.
The distribution of patients and public and private dialysis centres in the Eastern Cape is shown in Fig. 1. There were 32 private and 3 public dialysis centres in the province. The private dialysis centres were more evenly distributed throughout the province. There was a low prevalence of KRT in the public sector in East London and Mthatha. Even though the proportion of public v. private KRT provision was similar between East London and Mthatha, the Mthatha region provided KRT for 96 patients compared with 418 in East London. KRT provision in Gqeberha was similar between sectors, reflecting higher transplant rates in the public sector.
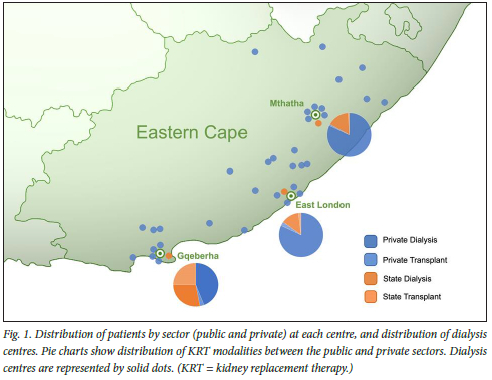
Comparisons of demographics and treatment rates between the geographical centres and by sector are shown in Table 2. There were marginal differences in age between the centres, but patients in the public sector were older in Mthatha than in Gqeberha and East London. East London had a more equal gender distribution between sectors, while the other two centres had more males on KRT, particularly in the private sector. There were significant differences in terms of dialysis modalities used. In both Gqeberha and East London, peritoneal dialysis (PD) was more commonly employed as the first and subsequent KRT modality, but very little PD was used in Mthatha. The HIV infection rate among KRT patients was 10 -11% in Gqeberha and 15% in the East London and Mthatha private sector. Only one patient in the public sector in East London was known to be HIV positive, while there were none in Mthatha. However, HIV status was not known in a high proportion of patients in East London and Mthatha (14% and 64%, respectively). A higher number of patients with a functioning transplant was observed in the public sector in Gqeberha (n=105) compared with East London (n=10) and Mthatha (n=1).
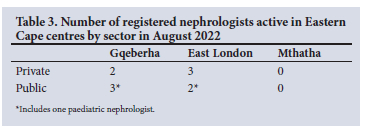
The numbers of registered nephrologists working in the various areas of the province in August 2022 are presented in Table 3. Eight were adult and two were paediatric nephrologists.
Data for patients who were waitlisted for a kidney transplant are presented in Table 4. There were no patients from Mthatha on the waiting list. Patients in the private sector were older than public sector patients. Gender disparity was most evident in private Gqeberha patients. The mean (SD) waiting time for waitlisted patients to receive a transplant was 5 (2 - 7) years. There were no waitlisted HIV-positive patients in the public sector in East London, compared with 16% of the public sector patients in Gqeberha. Only 40 (6%) of the 644 patients receiving dialysis in the private sector were currently waitlisted for a transplant, compared with 126 (67%) of 188 in the public sector Patients in East London waited a median of 3 - 6 years longer for a kidney transplant than those in Gqeberha.
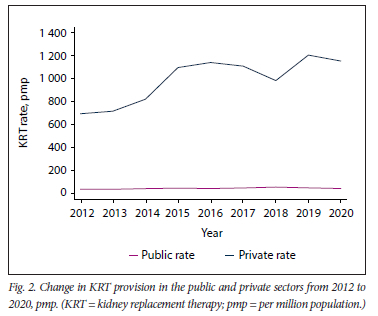
The change in KRT provision by the private and public sectors since the inception of the SARR is shown in Fig. 2. The rate of KRT provision in the public centre remained consistently <60 pmp, while there was a gradual increase in KRT in the private sector between 2013 and 2020.
Discussion
This study highlights the geographical and health sector disparities in access to KRT in the Eastern Cape. Patients in the private sector were 29 times more likely to access KRT than their public sector counterparts, and this inequality increased over time. Patients in the public sector were on average 18 years younger at initiation of KRT and less likely to have HIV, probably reflecting a marked selection bias in the province's overburdened public health system. There is also a geographical difference in access to transplantation, with patients progressively less likely to be waitlisted and transplanted the further east they are located, despite these being the more populous areas in the province. There were fewer patients on dialysis who were waitlisted for a transplant in the private sector compared with the public sector, and very few in either sector were transplanted pre-emptively, prior to initiation of dialysis. The prevalence of patients with a functioning kidney graft was very low at 22 pmp, and considerably lower than prevalence rates in Brazil (125 pmp)[31] and Spain (748 pmp).[26] Finally, public sector patients with HIV appeared to be largely excluded from receiving KRT in East London and Mthatha, reflecting regional differences in patient selection for KRT. However, this finding needs to be interpreted in the context of the large proportion of patients with unknown status. In the past, HIV was considered an exclusion for KRT in the public sector,[32] although recent SA data have shown equivalent outcomes after transplantation for HIV-positive recipients compared with HIV-negative recipients,[33] and no evidence of sustained superinfection.[34] Patients with HIV infection who are well controlled on ART should therefore be considered as candidates for kidney transplantation.[35]
We observed a very high rate of KRT in the private sector of the Eastern Cape, which is well above the national average of 729 pmp and could reflect an increased burden of kidney disease in this province. If the private sector KRT rate of 1 435 pmp is used as a proxy for similar need in the public sector, provincial authorities would need to progressively increase the numbers of public sector patients on KRT by >8 000 to align with the private sector KRT rate. Moreover, the distribution of dialysis services in the province is problematic in the public sector, where much of the population live large distances from the only three centres providing KRT services. This is in contrast to the much wider distribution of dialysis units in the private sector. These findings are important for policymakers to note, given the impending introduction of National Health Insurance (NHI) in SA. Due consideration should also be given to involving the private sector in partnerships to ramp up service provision progressively, as recently noted by the National Department of Health in view of experience with the COVID pandemic.[36]
The reasons for the overall disparate healthcare and KRT in the Eastern Cape are in part historical, resulting from the lack of provision of services and infrastructure in rural provinces during the apartheid era.[37] Other potential barriers to increasing KRT in the province are geographical distance from the KRT services, inadequate resource allocation, loss of skills to migration, stigmatisation regarding HIV or inadequate access to its treatment, inadequate training, lack of community education, lack of transparency, religious and cultural beliefs, and lack of government will.[11,38,39] At present, the geographical distance between the Eastern Cape treatment centres and the transplant units in the neighbouring Western Cape is a major challenge. In addition, travelling between sites has been hampered by the limited number of flight options from the Eastern Cape. Currently there is no direct flight from Mthatha to the transplant centres in Cape Town, and the distance by road is > 1 000 km. These circumstances are likely to hinder transplantation in the Mthatha region.
A major impediment to effective CKD care in the province is the lack of an estimate for the incidence and prevalence of CKD in SA. There are no published data specific to the Eastern Cape, although the authors' impression is that there has been an overwhelming increase in the number of young patients with advanced CKD who require KRT, and that the current resources are inadequate to manage this ever-growing disease burden. For example, SAs average starting age of KRT is 34 years compared with 53 years in Brazil, a country with a similar gross domestic product.[40] Furthermore, patients on KRT reflect a small proportion of those who have CKD, but do not yet require dialysis. With this in mind, primary- and secondary-level healthcare services need to be strengthened in order to screen for and treat these patients, because effective treatment can delay or even prevent progression of CKD to ESKD.[7,41] Poor communities remain at the highest risk owing to diminished health-seeking behaviour, and therefore need to be more actively screened.[42]
Nephrology and specialist medical professionals are pivotal in the provision of KRT. In the Eastern Cape, the lack of registered nephrologists in the Mthatha region is probably associated with the lack of access to KRT in that region. Patients rely on experienced physicians for kidney-related care, and there is an urgent need to establish sustainable nephrology services and appoint a transplant co-ordinator to facilitate the work-up and listing of patients for transplantation. On a positive note, there has been a small increase in the number of registered nephrologists in the province in recent years. Specific challenges to KRT have been identified on the broader African continent. These include severe workforce limitations, low government funding for kidney care, poor-quality data on CKD, and absence of national strategies and advocacy for kidney disease.[43] Hassen et al.[29] have highlighted the need to develop nephrology human resource services in under-served areas of SA, but this requires significant support from the public sector, including provision of posts, support from hospital management, improved workplace conditions for employees, and a need to address the difficulties encountered by nephrologists in the rationing of KRT resources. Globally, factors found to increase the number of trained nephrologists include flexible working programmes, novel recruitment strategies, and enhanced opportunities for research.[44] Training nephrologists who live in the under-served areas has been shown to be a successful approach to improve the provision of nephrology in a given area.[45]
Compared with Mthatha, the Gqeberha and East London regions use more PD as a first and subsequent KRT modality. This strategy was recently shown to be associated with good outcomes in SA and is therefore a favoured approach given that there is no need for reliable water and electricity infrastructure to perform PD.[46] This finding is therefore especially pertinent for the Eastern Cape, where large numbers of the population live in remote rural areas with insufficient infrastructure and therefore would ideally be more suited to PD as a modality. The number of patients on PD in the province could therefore be relatively easily increased without the need for investment in new infrastructure required for HD. However a successful PD programme will require the oversight of PD-trained nurses and nephrologists.[43]
Our study has some limitations. The SARR will be subject to the limitation of all databases, namely quality of data entry. However, the database is now in its 9th year of publication, and data entry and management have improved. We have relied on population estimates and the Council for Medical Schemes report to obtain the denominator for populations in the province. These estimates are subject to the accuracy of such data collection, although it is unlikely to affect the conclusions of this study in any material way. There was no population split by region available for 2021, so we used the last available data from the 2016 Stats SA community survey[47] to estimate the drainage populations in the various treatment centres, which could introduce a small error in the calculated KRT rate per centre. Similarly, our inability to assign 50 of the 978 patients (5%) to a specific treatment centre may have affected treatment centre KRT rates. We used the same percentage of patients with medical insurance across the entire province, and it is likely that there are small variations between geographical areas. Finally, there are a number of private sector independent dialysis units in the Eastern Cape that have not been logged on the SARR. However, including these patients in the registry would only marginally affect our private sector KRT treatment rate estimates.
Conclusion
KRT in the Eastern Cape reflects significant disparities in healthcare between the public and private sectors, with a large and concerning gap in dialysis provision. In order to address disparities, the incidence and prevalence of CKD in the province need to be estimated to better quantify the burden of kidney disease and forecast KRT provision. The systemic causes of low transplantation rates in both sectors warrant further investigation. Public health education and awareness programmes for the general public and healthcare workers are necessary to facilitate and increase screening for CKD. Nephrology human resources remain severely constrained and efforts to boost skilled training and collaboration are needed, especially with the anticipated implementation of NHI.
Declaration. The research for this study was done in partial fulfilment of the requirements for LM-N's MPhil (Int Med) degree at the University of Cape Town.
Acknowledgements. The authors are most grateful to Prof. Razeen Davids and his team for supplying required data from the SARR and for maintaining the database.
Author contributions. LM-N, RF, KM and EM conceptualised the study. LM-N, RJF, TdT and KM developed the protocol. KM performed the data analysis. ADR contributed to study design and final manuscript review. LM-N and RJF wrote the first manuscript draft and interpreted the data. All authors contributed to and approved the final manuscript.
Funding. This project is funded by the Division of Intramural Research. National Institute of Allergy and Infectious Diseases, National Institutes of Health (grant no. 1U01AI152153).
Conflicts of interest. None.
References
1. Adeniyi AB, Laurence CE, Volmink JA, Davids MR. Prevalence of chronic kidney disease and association with cardiovascular risk factors among teachers in Cape Town, South Africa. Clin Kidney J 2017;10(3):363-369. https://doi.org/10.1093/ckj/sfwl38 [ Links ]
2. Matsha TE, Yako YY, Rensburg MA, Hassan MS, Kengne AP, Erasmus RT. Chronic kidney diseases in mixed ancestry South African populations. Prevalence, determinants and concordance between kidney function estimators. BMC Nephrol 2013;14:75. https://doi.org/10.1186/1471-2369-14-75 [ Links ]
3. Fabian J, Gondwe M, Mayindi N, et al. Chronic kidney disease (CKD) and associated risk in rural South Africa. A population-based cohort study Wellcome Open Res 2022;7:236. https://doi.org/10.12688/wellcomeopenres.l8016.2 [ Links ]
4. Mayosi BM, Benatar SR Health and health care in South Africa - 20 years after Mandela. N Engl J Med 2014;371(14):1344-1353. https://doi.org/10.1056/NEJMsrl405012 [ Links ]
5. Stanifer JW, Jing B, Tolan S, et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: A systematic review and meta-analysis. Lancet Glob Health 2014;2(3):e174-e181. https://doi.org/10.1016/S2214-109X(14)70002-6 [ Links ]
6. Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease - a systematic review and meta-analysis. PLoS ONE 2016;11(7):e0158765. https://doi.org/10.1371/journal.pone.0158765 [ Links ]
7. Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease. Global dimension and perspectives. Lancet 2013;382(9888):260-272. https://doi.org/10.1371/journalpone.0158765 [ Links ]
8. Statistics South Africa. Mid-year population estimates 2022. Statistical release P0302. Pretoria. Stats SA, 2022. https://www.statssa.gov.za/publications/P0302/P03022022.pdf (accessed 8 August 2022). [ Links ]
9. World Population Review. Gini coefficient by country 2022. https://worldpopulationreview.com/country-rankings/gini-coefficient-by-country (accessed 8 August 2022). [ Links ]
10. Muller E. Transplantation in Africa - an overview. Clin Nephrol 2016;86(7):90. https://doi.org/10.5414/CNP86S125 [ Links ]
11. Naicker S. End-stage renal disease in sub-Saharan Africa. Ethn Dis 2009;19(1 Suppl 1):S 1-13-5. [ Links ]
12. Swanepoel CR, Wearne N, Okpechi IG. Nephrology in Africa - not yet uhuru. Nat Rev Nephrol 2013;9(10):610-622. https://doi.org/10.1038/nrneph.2013.168 [ Links ]
13. Naicker S. End-stage renal disease in sub-Saharan Africa. Kidney Int Suppl 2013;3(2):161-163. [ Links ]
14. Davidson B, du Toit T, Jones ESW, et al. Outcomes and challenges of a kidney transplant programme at Groote Schuur Hospital, Cape Town. A South African perspective. PLoS ONE 2019;14(1):e0211189. https://doi.org/10.1371/journal.pone.0211189 [ Links ]
15. Garcia GG, Harden P, Chapman J, for the World Kidney Day Steering Committee. The global role of kidneytransplantation. Nephron Clin Pract 2012;120(2):c101-c106.https://doi.org/10.1159/000337043 [ Links ]
16. Moosa M. The state of kidney transplantation in South Africa. S Afr Med J 2019;109(4):235-240. https://doi.org/10.7196/SAMJ.2019.vl09i4.13548 [ Links ]
17. Moosa MR, Kidd M. The dangers of rationing dialysis treatment. The dilemma facing a developing country. Kidney Int 2006;70(6):1107-1114. https://doi.org/10.1038/sj.ki.5001750 [ Links ]
18. Kilonzo KG, Jones ESW, Okpechi IG, et al. Disparities in dialysis allocation. An audit from the new South Africa. PLoS ONE 2017;12(4):e0176041. https://doi.org/10.1371/journal.pone.0176041 [ Links ]
19. Etheredge H, Fabian J. Challenges in expanding access to dialysis in South Africa - expensive modalities, cost constraints and human rights. Healthcare (Basel) 2017;5(3):38. https://doi.org/10.3390/healthcare5030038 [ Links ]
20. Moosa MR Priority setting approach in the selection of patients in the public sector with end stage kidney failure for renal replacement treatment in the Western Cape Province. ProPublica, 2010. www.propublica.org/documents/item/dialysis-selection-guidelines-western-cape-province (accessed 8 August 2022). [ Links ]
21. Moosa MR Maree JD, Chirehwa MT, Benatar SR. Use of the 'accountability for reasonableness' approach to improve fairness in accessing dialysis in a middle-income country. PLoS ONE 2016;11(10):e0164201. https://doi.org/10.1371/journal.pone.0164201 [ Links ]
22. Molaoa TT, Bisiwe FB, Ndlovu KC. End-stage kidney disease and rationing of kidney replacement therapy in the Free State province, South Africa. A retrospective study. BMC Nephrol 2021;22(1):174. https://doi.org/10.1186/sl2882-021-02387-x [ Links ]
23. Okpechi IG, Swanepoel CR Rayner BL. Outcomes of rationing dialysis therapy in biopsy-proven end-stage renal disease in South Africa. J Nephrol 2012;25(4):551-557. https://doi.org/10.5301/jn.5000032 [ Links ]
24. Council for Medical Schemes. Annual Report 2020/21. https://www.medicalschemes.co.za/cms-annual-report-2020-21 (accessed 8 August 2022). [ Links ]
25. Davids MR, Jardine T, Marais N, Sebastian S, Jacobs J. South African Renal Registry Annual Report 2020. Afr J Nephrol 2022;25(1):155-166. https://doi.org/10.21804/25-l-5398 [ Links ]
26. Crespo M, Mazuecos A, Dominguez-Gil B. Global perspective on kidney transplantation. Spain. Kidney360 2021;2(11):1840-1843. https://doi.org/10.34067/KID.0002502021 [ Links ]
27. Statistics South Africa. Inequality trends in South Africa. A multidimensional diagnostic of inequality. Pretoria: Stats SA, 2019. https://www.statssa.gov.za/publications/Report-03-10-19/Report-03-10-192017.pdf (accessed 8 August 2022). [ Links ]
28. Hansoti B, Mwinnyaa G, Hahn E, et al. Targeting the HIV epidemic in South Africa. The need for testing and linkage to care in emergency departments. EClinicalMedicine 2019;15:14-22. https://doi.org/10.1016/j.eclinm.2019.08.007 [ Links ]
29. Hassen M, Archer E, Pellizzon A, Chikte UME, Davids MR. Human resources for nephrology in South Africa. A mixed-methods study. PLoS ONE 2020;15(2):e0228890. https://doi.org/10.1371/journalpone.0228890 [ Links ]
30. Davids MR, Marais N, Jacobs JC. 2012. South African Renal Registry Annual Report 2012. Cape Town. South African Renal Society, 2014. https://scholar.sun.ac.za/handle/10019.1/95534 (accessed 8 August 2022). [ Links ]
31. Oliveira MB, Româo JE Jr, Zatz R. End-stage renal disease in Brazil. Epidemiology, prevention, and treatment. Kidney Int 2005;68:S82-S86.https://doi.org/10.1111/j.l523-1755.2005.09714.x [ Links ]
32. Muller E, Barday Z, Mendelson M, Kahn D. Renal transplantation between HIV-positive donors and recipients justified. S Afr Med J 2012;102(6):497-498. https://doi.org/10.7196/SAMJ.5754 [ Links ]
33. Durand CM, Zhang W, Brown DM, et al A prospective multicenter pilot study of HIV-positive deceased donor to HIV-positive recipient kidney transplantation. HOPE in action. Am J Transplant 2021;21(5):1754-1764. https://doi.org/10.1111/ajt.16205 [ Links ]
34. Selhorst P, Combrinck CE, Manning K, et al. Longer-term outcomes of HIV-positive-to-HIV-positive renal transplantation. N Engl J Med 2019;381(14):1387-1389. https://doi.org/10.1056/NEJMc1903013 [ Links ]
35. Muller E, Barday Z Mendelson M, Kahn D. HIV-positive-to-HIV-positive kidney transplantation -results at 3 to 5 years. N Engl J Med 2015;372(7):613-620. https://doi.org/10.1056/NEJMoal40889e [ Links ]
36. Solanki G, Blecher M, Cornell J, et al COVID-19. Insights from contracting the private sector for critical care. Im South African Health Review 2021. Durban. Health Systems Trust;2021:83-93. https://journals.co.za/doi/abs/10.10520/ejc-healthr-v2021-n1-all (accessed 8 August 2022). [ Links ]
37. Stuckler D, Basu S, McKee M. Health care capacity and allocations among South Africa's provinces. Infrastructure-ine quality traps after the end of apartheid. Am J Public Health 2011;101(1):165-172. https://doi.org/10.2105/AJPH.2009.184895 [ Links ]
38. Bookholane H, Michaelides A, Prins L, et al. Factors influencing consent rates of deceased organ donation in Western Cape Province, South Africa. S Afr Med J 2020;110(3):204-209. https://doi.org/10.7196/SAMJ.2020.vll0i3.14227 [ Links ]
39. Katz IJ, Gerntholtz T, Naicker S. Africa and nephrology. The forgotten continent. Nephron Clin Pract 2011;117(4):320-327. https://doi.org/10.1159/000321524 [ Links ]
40. Moraes TP, Pecoits-Fiiho R, Ribeiro SC, et al. Peritoneal dialysis in Brazil. Twenty-five years of experience in a single center. Perit Dial Int 2009;29(5):492-498. [ Links ]
41. Grill AK, Brimble S. Approach to the detection and management of chronic kidney disease. What primary care providers need to know. Can Fam Physician 2018;64(10):728-735. [ Links ]
42. Van der Hoeven M, Kruger A, Greeff M. Differences in health care seeking behaviour between rural and urban communiües in South Africa. Int J Equity Health 2012,11.31. https://doi.org/10.1186/1475-9276-11-31 [ Links ]
43. Oguejiofor F, Kiggundu DS, Belio AK, et al. International Society of Nephrology Global Kidney Health Atlas. Structures, organization, and services for the management of kidney failure in Africa. Kidney Int Suppl 2021;11(2):e11-e23. https://doi.org/10.1016/j.kisu.2021.01.009 [ Links ]
44. Sharif MU, Elsayed ME, Stack AG. The global nephrology workforce. Emerging threats and potential solutions! Clin Kidney J 2016;9(1):11-22. https://doi.org/10.1093/ckj/sfvlll [ Links ]
45. Harris DC, Dupuis S, Couser WG, Feehally J. Training nephrologists from developing countries. Does it have a positive impact? Kidney Int Suppl 2012;2(3):275-278. https://doi.org/10.1038/kisup.2012.32 [ Links ]
46. Davidson B, Crombie K, Manning K, Rayner B, Wearne N. Outcomes and challenges of a PD-first program, a South-African perspective. Perit Dial Int 2018;38(3):179-186. https://doi.org/10.3747/pdi.2017.00182 [ Links ]
47. Statistics South Africa. Community survey 2016. Statistical release P0301. Pretoria. Stats SA, 2016. http://cs2016.statssa.gov.za/wp-content/uploads/2016/07/NT-30-06-2016-RELEASE-for-CS-2016-_Statistical-releas_l-July-2016.pdf (accessed 8 August 2022). [ Links ]
 Correspondence:
Correspondence:
R J Freercks
robert.freercks@uct.ac.za
Accepted 30 January 2023














