Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.1 Pretoria Jan. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i1.16661
RESEARCH
The utility of mobile telephone-recorded videos as adjuncts to the diagnosis of seizures and paroxysmal events in children with suspected epileptic seizures
K OyiekeI; J M WilmshurstII
IMB ChB, MPhil; Department of Paediatric Neurology, Red Cross War Memorial Children's Hospital, and Neuroscience Institute, University of Cape Town, South Africa
IIMBBS, MD; Department of Paediatric Neurology, Red Cross War Memorial Children's Hospital, and Neuroscience Institute, University of Cape Town, South Africa
ABSTRACT
BACKGROUND. Epilepsy is often diagnosed through clinical description, but inter-observer interpretations can be diverse and misleading.
OBJECTIVE. To assess the utility of smartphone videos in the diagnosis of paediatric epilepsy.
METHODS. The literature was reviewed for evidence to support the use of smartphone videos, inclusive of advantages, ethical practice and potential disadvantages. An existing adult-based quality of video (QOV) scoring tool was adapted for use in children. A pilot study used convenience sampling of videos from 25 patients, which were reviewed to assess the viability of the adapted QOV tool against the subsequent diagnosis for the patients with videos. The referral mechanism of the videos was reviewed for the source and consent processes followed.
RESULTS. A total of 14 studies were identified. Methodologies varied; only three focused on videos of children, and QOV was formally scored in three. Studies found that smartphone videos of good quality assisted the differentiation of epilepsy from non-epileptic events, especially with accompanying history and with more experienced clinicians. The ethics and risks of circulation of smartphone videos were briefly considered in a minority of the reports. The pilot study found that the adapted QOV tool correlated with videos of moderate and high quality and subsequent diagnostic closure.
CONCLUSIONS. Data relating to the role of smartphone video of events in children is lacking, especially from low- and middle-income settings. Guidelines for caregivers to acquire good-quality videos are not part of routine practice. The ethical implications of transfer of sensitive material have not been adequately addressed for this group. Prospective multicentre studies are needed to formally assess the viability of the adapted QOV tool for paediatric videos.
Epilepsy is largely a clinical diagnosis based on the semiology of the seizures.[1,2] The motor, sensory and behavioural signs are key in describing seizure semiology and subsequently, seizure type. However, healthcare workers rarely witness seizures, so the events are often relayed by verbal accounts to physicians during subsequent consultations. The physician makes deductions from caregiver descriptions. The perceived anxiety and potential risks of not treating an affected child with possible epilepsy may result in misdiagnosis and mismanagement. Some 20 - 30% of those referred to tertiary centres with refractory epilepsy do not in fact have epilepsy,[3-6] hence the need for accurate descriptions of seizure events.[7]
The gold standard to confirm a diagnosis of epilepsy is to capture an ictal event via electroencephalogram (EEG) with video running (video EEG telemetry).[8,9] However, video EEG telemetry (vEEG) is a scarce resource, and seizures or paroxysmal events may not occur during the recording.[10]
The increasing use of telemedicine and mobile-phone technology (smartphones) illustrates use of newer technologies that play a valuable role in the management of epilepsy, and should be integrated into existing clinical pathways. The COVID-19 pandemic has highlighted that telehealth enables patients to gain access to healthcare, being exclusively used by 24.7% of child neurologists to manage their epilepsy patients during the early period of the pandemic.[11]
The present study undertakes a literature review, puts forward an adapted video screening tool and assesses the efficacy of the home videos through a convenience pilot study. The study aims to outline the accuracy of home videos in the diagnosis of paediatric epilepsy.
Methodology
Literature review
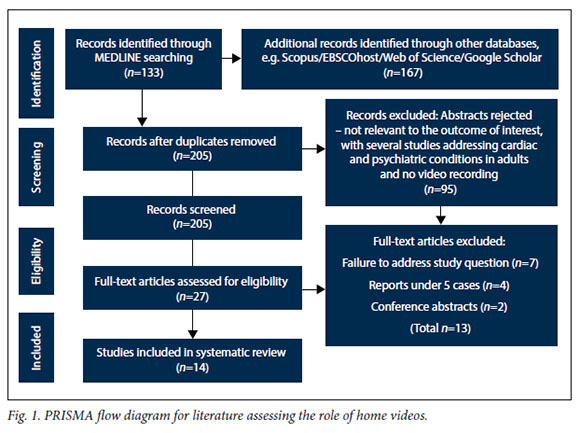
Search terms and methodology are summarised in the appendix (https://www.samedical.org/file/1950). Fig. 1 illustrates the PRISMA flow diagram for the identified articles. After removal of duplications, 205 article abstracts were screened, and 27 identified for full review.
Included studies were reviewed for knowledge and guidelines for the use and assessment of home video to delineate seizures and paroxysmal events. The studies were further explored for the advantages and disadvantages of home video. Aspects were noted that were deemed necessary for optimal recommended models for the intervention, encompassing safe ethical practice related to the use of confidential data.
Development of a quality of video scoring tool for children to grade assessment of video-submitted material
An existing quality of video (QOV) tool[12,13] designed for use in adult patients was adapted for paediatric use and incorporated into a pilot study.
Retrospective convenience study and assessment of viability of the adapted QOV tool
The Red Cross War Memorial Children's Hospital (RCWMCH), Cape Town, is a public paediatric teaching hospital in South Africa (SA). The paediatric neurology department receives frequent referrals of children with paroxysmal events into its dedicated epilepsy service. New patients are referred via inpatient and emergency services, primary and secondary healthcare facilities and private clinicians. Referrals are via telephonic request, fax or a video-recorded event of a child suspected to have an epileptic seizure, occasionally with some explanatory text message. A proportion of referrals from emergency or outpatient clinic present with a captured video event, while others follow instructions and subsequently record events ready for the follow-up consultation. To delineate and to better understand this group, video recordings from 25 children consecutively referred to the service were reviewed by two child neurologists who were blinded to the final diagnosis. The adapted QOV tool was assessed for use and viability in this setting.
The study population and inclusion criteria were children <18 years of age referred via videos to the neurology service who were suspected to have epileptic seizures or in whom there was diagnostic uncertainty, children who were reviewed for the first time with suspected seizures, and children with undefined seizures where the type of event could not be delineated based on clinical history. Referring clinicians were requested to attain parental consent and, where appropriate, children's assent, for the video recordings.
The study excluded children in whom a definite diagnosis of epilepsy was already made.
Data collected included the source of the video (parent, clinician), patient demographics, whether a presumptive diagnosis was made, if clinical history accompanied the recording, the QOV score and how the video changed the care for the child. The video diagnoses were reviewed by blinded paediatric neurologists in the service and records were kept of any discrepancies.
The study outcome was to establish evidence to support the use of home videos to delineate seizures and paroxysmal events, and to generate a recommendation for clinicians and caregivers to optimise mobile phone video-recording of events in children.
The study was conducted following approval of the research committee at RCWMCH and ethics approval from the Faculty of Health Sciences Research and Ethics Committee, University of Cape Town (ref. no. HREC 402/2020).
Results
Available literature on home video recordings for seizures and paroxysmal events in children
Fig. 1 summarises the literature search flow. The appendix summarises the 14 studies using PICO (population, intervention, comparator and outcome) criteria.
Population: Huang et al[14] recruited 452 paediatricians. Other studies recruited small numbers of clinicians. Ojeda et all12-recruited three epileptologists, and Amin et al[15] two epilepsy specialists. Tatum et al[16,17] recruited epileptogists and residents for both OSmartViE study reports; Ramanujam'18-studied competency of 'the epilepsy fellow', Karakas,[19] Chen,[20] Erba[21] and Beniczky[22]recruited small numbers of epileptologists, Goodwin et all3 referred to clinicians only and Samuel and Duncan[24] to 'medical staff'. Wasserman and Herskovitz[25] recruited 26 neurologists and 20 non-neurology practitioners, inclusive of nursing staff. Dash et al.'[13] used a different model, recruiting 312 caregivers and patients to record videos.
Intervention: All studies were prospective. Tatum et al.[17] showed a large number of videos (n=530) from 44 patients to a selected number of epileptologists (n=10) and trainees (n=9). Tatum et al.[16]-in their further analysis recruited 7 epilepsy experts and 6 residents to assess the quality of the videos and how this impacted on the diagnoses. Huang et al[14] used 12 selected videos of infants with paroxysmal events to show to 452 paediatricians who were
initially only supplied with a description of the events. Likewise, Wasserman and Herskovitz[25] used 10 videos of five epileptic seizures and five psychogenic non-epileptic seizures (PNES) to show to neurologists and non-neurologists. Karakas et al.[19] assessed the accuracy of four epileptologists to diagnose smartphone-recorded events from 50 veterans with established diagnoses. Amin et al.[15] also explored the accuracy of two specialists to diagnose smartphone video events consecutively brought to an epilepsy service based on the subgroup for whom vEEG confirmed the definitive diagnosis.[18] Beniczky et al.[22] assessed the accuracy of clinical description compared to video-captured events, and Erba et al.[21]the ability of adult and child neurologists to categorise types of epileptic and non-epileptic events. Chen et al.[20] similarly reviewed the sensitivity and specificity of selected events recorded during vEEG of adults with epileptic seizures and PNES. These researchers were exploring the competency of clinicians to differentiate events based on selected videos with or without the addition of clinical information. Ramanujam et al.[18]also selected better-quality videos (n=269) to show to a blinded epilepsy fellow to assess ability to differentiate PNES. In a similar study, Ojeda et al.[12] recruited 135 home videos, which were scored for quality and shown to three epileptologists to assess accuracy in differentiating of events. Dash et al.'13- recruited 624 video events that were screened by epilepsy trainees and neurology specialists using a 29-point questionnaire. Goodwin et al.[23]-and Samuel and Duncan[24] encouraged patients to undertake home videos, which were reviewed for diagnostic use in small cohorts (n=45 and 22, respectively).
Comparator: Tatum et al.[16,17] explored the validity of smartphone video to differentiate events based on the experience of the reviewer (epileptologist v. trainee). Similarly, Wasserman and Herskovitz[25] assessed the ability of different practitioners, from neurologists to emergency medicine nurses. Karakas et al.[19] assessed whether the tool was more accurate with the addition of basic patient demographic information. Huang et al.[14] explored how the addition of video after the description added to the subsequent ability to accurately differentiate events. Ramanujam[18] assessed the accuracy of the home video events compared with vEEG. Ojeda et all12-also explored features captured in the videos that experts found useful in differentiation of events as scored via the QOV tool. They then explored whether the original diagnosis was revised by the process. Dash et al.[13] used their 29-point questionnaire, which was completed by caregivers and clinicians against history and video, with final diagnosis verified by vEEG. Chen et al.[20] assessed the confidence of specialists to differentiate the videos captured as part of vEEG procedure compared with the EEG in isolation. Similarly, Beniczky[22] assessed the consensus of specialists when provided with clinical event descriptions compared with videos of events, and Erba[21] the confidence of specialists categorising different clinical events. Samuel and Duncan[24] and Goodwin et al.[23] did not have a comparator group.
Outcome: Tatum et al.[16,17] found that experts were more accurate in predicting diagnosis, while residents were less accurate but tended to have greater confidence. Motor signs and additional history increased diagnostic yield. They supported use of the tool to aid diagnosis of PNES and to triage urgency of patients awaiting vEEG, and further strengthened this statement in their follow-up analysis of the quality of the videos. These findings were supported by Chen et al.[20] who, based on the high sensitivity and specificity of their results, concluded that home video could have a role in early differentiation of PNES from epileptic seizures. The group further highlighted useful clinical signs to aid differentiation. Beniczky et al.[22] demonstrated the significantly higher consensus and accuracy of specialists when reviewing videos compared with being provided with clinical descriptions in isolation, and Erba[21] found that videos could be used to categorise events in a third of cases. Karakas et al.,[19] however, found that adding basic demographic information did not significantly increase diagnostic yield. Huang et al.[14] found that use of home video was a cost-effective tool, and useful to diagnose paroxysmal events in infants - the more senior the clinician, the more accurate the diagnostic yield. Ramanujam et al.[18] concluded that good-quality home videos can be used to differentiate PNES from epileptic seizures, and can complement vEEG in diagnosing PNES in a cost-effective manner. The group critiqued and assessed useful and important clinical markers to note during the video. Amin[15] also promoted the use of the tool as a diagnostic adjunct for seizure-like events. Wasserman and Herskovitz[25] found that more experienced neurologists were statistically more effective in correctly diagnosing events compared with general physicians. Knowledge gained through accompanying the neurologist was hypothesised to explain why the emergency medicine nurses performed better than the general physicians. Ojeda et al.[12] found that the non-epileptic events resulted in better QOV scores than epileptic seizures (although this failed to reach statistical significance). Furthermore, of the recruited group, the researchers were only able record videos in about half of the patients. The group suggested that training and guidance is needed for caregivers to attain optimal videos. Dash et al.[13] found that focal seizures were more likely to be correctly diagnosed in patients with a home video, compared with when only history was available. Assessment of the home videos detected significantly more semiological signs than the history alone. The group devised the scoring system referred to as the QOV scale with 11 items. The study concluded that home video aided epilepsy diagnosis and PNES differentiation. Goodwin et al.[23] noted that selection and recruitment of the correct patient is important for the best results. Samuel and Duncan[24] concluded that home videos were useful differentiating aids, and the researchers noted that interaction with patients during events was useful.
Limitations in the studies included bias where only the fair and good-quality videos were included.[18,19,23] Some patients and caregivers declined to join studies or failed to capture adequate quality videos, inclusive of when events were too short to record.[12,16,18] The studies varied as to whether caregivers were trained or guided for optimal videos.[12,13] Only three studies included focus on child or adolescent home videos for review.[14,18,25] There were variances in the directness and consistency of the studies, such that some recruited large numbers of clinicians who reviewed a small number of carefully selected videos to verify their ability to differentiate epileptic from non-epileptic seizures.[14] Other studies selected large numbers of home videos and showed them to small select groups of clinicians.[17-Some of these videos were selected following screening for the best-quality videos after direction was given to caregivers for best quality, while others were random selections as presented by caregivers.[2,18] Some studies provided additional information such as history or verified outcomes when compared with vEEG telemetry.[17,18] Three of the studies (two from the same group)[12,13,18] used the QOV tool.
Studies established that home videos are useful to aid differentiation between epileptic and non-epileptic seizures, especially when viewed by a more experienced clinician and if accompanying history was provided.[13,14,17,25] All the studies supported use of smartphone videos to aid assessment of patients with undiagnosed paroxysmal events. There was consensus that videos can be challenging to capture, and optimally useful with fair-to-good QOV scores.[12,13,18] While the QOV scoring system has some important criteria, it focused on analysis of events in adults.
The use of secure online platforms was noted by some of the more recent studies, but none commented on the ethics of families bringing videos of sensitive and personal recordings and the manner in which these are routinely circulated in clinical practice.[16,17,22]
Recommended QOV tool for children to assess video-submitted material
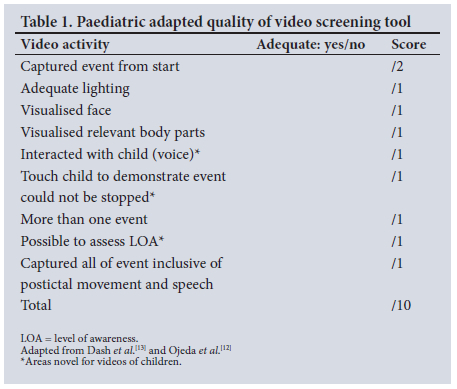
Based on the elements analysed in the literature, a grading system was adapted from the tool developed for adult QOV to critique the quality of a submitted video of a child (Table 1).[12,13] Key elements included in the adapted scale for children were whether the caregiver interacted with the child, if the event could be interrupted by touch, and whether level of awareness could be gauged from the video. In line with Dash et al.[13] recommendations, the maximum score for the QOV scale was 10. A score of 1 - 4 was considered poor quality, 5 - 7 moderate quality, and 8 - 10 good quality.[13-
Results of convenience sample
The 25 recordings were sent consecutively to the neurology team WhatsApp group (June 2019 - January 2020). Parents recorded the videos and provided verbal permission for the files to be sent for assessment via their referring clinicians, or clinicians made the recordings themselves with verbal consent from the carer. Similar to other studies, the main question was to determine whether the recorded event was an epileptic seizure or not, and to further define focal seizures in a number of cases. Table 2 summarises the key findings.
Of the 25 recordings sampled, 14 (56%) were male and 11 (44%) were female patients, ranging in age from 2 months old to 11 years of age, with a median age of 18 months. The quality of video recordings for clarity and capturing of the onset/early manifestations was adequate, and correlated with QOV scoring in 19 of the 25 videos (76%). Clinicians could make a correct diagnosis in 18 out of the 19 cases (95%) with high certainty, often without requiring the accompanying history. Patient 10 had a video supplied directly by a caregiver, which demonstrated myoclonus and facilitated urgent referral for a more detailed assessment, as the accompanying history was inadequate. Of the 18 confirmed cases, 11 were epileptic events and 7 were non-epileptic.
The remaining 6 video recordings (24%) were of poor quality owing to the onset not being captured in 5 videos (83%), the face not being visible in 3 (50%) and the carer not stimulating the patient in 2 videos (33%). The quality issues often overlapped. The adapted QOV scale was <3 for all.
In the videos where a diagnosis was possible, management and appropriate referrals were made, with the majority commenced on antiseizure medication, or existing antiseizure medications switched to more appropriate agents. Urgent medical intervention was enabled where relevant, e.g. admission and steroids commenced for epileptic spasms (patients 7, 18 and 22).
A brief history supplied for 15/25 (60%) of the videos was associated with improved diagnostic accuracy. A definitive diagnosis was possible in 11 out of the 15 videos (73%) with a history. In comparison, a definitive diagnosis was possible for only three of the remaining nine videos (33%) which lacked an accompanying history.
Consent was obtained verbally by the referring clinician from the parent in order to share the recording with a specialist. It emerged, however, that details of sharing video recordings across online platforms were not always discussed with the carers from the outset.
Discussion
Epilepsy is the most common neurological condition, with an estimated 50 million people affected in the world, of whom up to 75% live with little to no access to medical services or treatment, especially vEEG.[10,26-28] Moreover, the global COVID-19 pandemic has further disrupted access to medical care, with limitations on movement and health resource reallocations, making telemedicine an increasingly attractive and useful resource to improve access to clinical services, especially in the management of epilepsy.
The literature search revealed gaps in data which assessed the use of smartphone video recordings in the diagnosis of paroxysmal events, especially for paediatric populations. No studies were conducted in the African setting. Studies are needed to address the role of mobile video recordings in epilepsy diagnosis, especially across ethical, diagnostic, management, educational and research areas. The ethics of sharing mobile video recordings and the importance of consent/ assent were not adequately addressed, highlighting the issue of safety, ownership and regulation of sensitive patient information shared across internet platforms among vulnerable populations. However, the tool has the potential to support existing infrastructure and facilitate established referral and communication networks in the clinical assessment of remote patients. Further, there are potential educational and research benefits emanating from the collection of large amounts of data used for characterising paediatric seizures.
The accuracy of seizure descriptions by witnesses, including medical professionals, is highly variable.[29] Neurologists are better at the diagnosis of epilepsy than non-specialists (mistake rate 5.6% v. 18.9%).[30] The misdiagnosis rate of epilepsy is high, reported at 23% - 71% depending on the population group sampled and the methodology of screened patients.[4-6,30,31]
The accuracy of seizure documentation and description by patients varies over time.[32] Witnesses tend to inaccurately describe movements, misleading medical professionals away from focal events.[33] Subtle features such as automatisms, lip movements or staring episodes are more difficult to identify, not just for lay persons but also healthcare professionals.[34] Different semiologies can be associated with different levels of reporting accuracy, with non-convulsive semiologies being less accurately described than convulsive events.[35-Facial appearance and vocalisations were most accurately described, while limb movements and post-ictal behaviour are least accurately recalled and described.[36]
Mobile phone technology plays an integral part in our daily lives, with evolving roles beyond a communication device.[37-45] However, seizure detection methods are considered to be in the early stages of development.[46]
Mobile technology is easy to use and does not require special training. Furthermore, it is becoming increasingly accessible in low-and middle-income countries (LMICs).[47] Smartphone ownership/ social media utilisation averages 42% in LMICs and 72% in high-income countries.[48]
The use of mobile technology in the description of seizures serves as an adjunct to diagnosis, and should not substitute a good clinical history and examination. The incorporation of mobile technology to facilitate epilepsy diagnosis requires access to mobile phones and electricity, as well as reliable internet connectivity to relay video recordings, which may be challenging in rural areas in some LMICs. Sociocultural barriers may also exist for sharing of information relating to epilepsy, and this may influence carers negatively. Witnesses may not be available to record events, or they may be preoccupied and worried about the safety of the patient. In other instances, seizures may be very brief and/or subtle, and therefore not easily captured by video recording. Nocturnal events and events occurring in poorly lit areas may also not be picked up and recorded. Additionally, the beginning of the event may be difficult to record, especially if seizure evolution is very fast, occurs with little warning or if there are behaviours or somatosensory auras not recognised as ictal.
Based on the literature review and the convenience sample findings, the following aspects are important to document in the setting of a home video referral: presence of accompanying history from referring source; level of experience of the referring clinician (in instances where the source is a clinician); and whether the caregiver was given instructions on how to take an optimal home video. The outcome of the videos should be graded according to the QOV (Table 1) and the confidence of the specialist to make a diagnosis, which should fall into the following categories: certain, possible, or not possible. Children in whom the diagnosis remains unclear will be the group directed for more extensive interventions by means of further history, additional videos and potentially vEEG.
The use of online media platforms for sharing or conveying video material also carries the risk of security breach of the patient's private information. Concern about information privacy on mobile platforms carries a high litigation risk for all parties involved, and can also be a deterrent for patients to use the services. There are also emerging concerns on the proprietary ownership of information that is shared on online platforms, considering that a permanent data record is held in custodial trust by internet domains, and as such is not entirely owned by the person who made the recording. Data records are also vulnerable to other cyber threats, such as infiltration/ corruption of stored electronic records by computer viruses, etc. Clinicians must abide by the Protection of Personal Information Act No. 4 of 2013, passed in SA and equivalent to the European Union General Data Protection Regulation. This Act reinforces the lawful and responsible processing of the personal information of data subjects. One secure resource that is increasingly used in SA is the Vula app (Vula Mobile, SA; https://www.vulamobile. com). This tool allows healthcare workers to connect via a secure platform for patient referrals. It can be customised, and as such could be a feasible resource for upload and transfer of sensitive video material. Another tool, routinely used in the UK, is the vCreate platform (vCreate, UK; https://www.vcreate.tv/neuro). This has been formatted specifically for neurological referrals, and has entry points for different providers to access, inclusive of caregivers, general doctors and specialists. The platform has been audited and found to permit more targeted patient care approaches, such as those in need of urgent assessment or neuroimaging, or who do not need neurology referral at all. Audit of implementation of the tool in the UK supports both cost saving and improved patient care. The vCreate group are exploring expanding their platform to resource-limited regions, including SA.
Study limitations
The existing studies lacked consistency in study methodology and directness in terms of study question, which limited comparison of findings. To the best of our knowledge, we identified all studies relevant to our study question, but the search terms may have been too narrow and missed some reports. Furthermore, use of videos is common, and the structured studies may not have represented real clinical practice. The convenience sample was small and limited to clinicians/carers with access to a paediatric neurology service, and may not adequately represent the breadth of paroxysmal events in the wider population. This assessment was undertaken to assess the viability of the QOV tool rather than to understand the complete range of video cases referred to the service. As such, larger multicentre trials would be needed to assess the viability of the adapted paediatric QOV tool.
Conclusion
The available literature supported the idea that home-video recordings of good quality, reviewed by experienced clinicians, with accompanying history, can be beneficial to differentiate between epileptic and non-epileptic seizures, thus improving reliability and diagnostic accuracy. This could lead to earlier, more targeted care, and avoid unnecessary invasive and costly interventions and risk of inappropriate antiseizure medications. The reviewed studies varied in consistency and directness in their methodologies. Few formally critiqued the quality of the submitted videos using the QOV scale. Only three studies included children. The ethical issues of transfer of private information on internet domains were not categorically addressed in these studies.
Based on the findings of the retrospective convenience sample, coupled with the paucity of similar studies in children, there is a need for a prospective study to delineate whether the growing practice of using mobile video recordings, particularly in the current post-pandemic context, is an appropriate tool to add to the management of people with epilepsy, and to understand how this should be implemented for optimal ethical and management outcomes. A multicentre prospective study would further enable protocol development for seizure diagnostic aids utilising mobile video technology.
The ethical concerns of conveying sensitive information across internet platforms also need to be highlighted. Liaison between referring and receiving clinicians on video-captured events will further define the knowledge gaps among healthcare practitioners on identification of paroxysmal events and target education needs. It will also help to inform parental education needs regarding seizure identification.
Declaration. None.
Acknowledgements. Thanks to parents for permission to include home videos and clinicians in the neurology service for identifying cases.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia 2014;55(4):475-482. https://doi.org/10.1111/epi.12550 [ Links ]
2. Scheffer IE, Berkovic S, Capovilla G, et al ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017;58(4):512-521. https://doi.org/10.1111/epi.13709 [ Links ]
3. Hauser WA. The prevalence and incidence of convulsive disorders in children. Epilepsia 1994;35(Suppl 2):S1-S6. [ Links ]
4. Smith D, Defalla BA, Chadwick DW. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. QJM 1999;92(1):15-23. https://doi.org/10.1093/qjmed/92.115 [ Links ]
5. Hindley D, Ali A, Robson C. Diagnoses made in a secondary care 'fits, faints, and funny turns' clinic. Arch Dis Child 2006;91(3):214-218. https://doi.org/10.1136/adc.2004.062455 [ Links ]
6. Scheepers B, Clough P, Pickles C. The misdiagnosis of epilepsy: Findings of a population study. Seizure 1998;7(5):403-406. https://doi/10.1016/s1059-1311(05)80010-x [ Links ]
7. Oto MM. The misdiagnosis of epilepsy: Appraising risks and managing uncertainty. Seizure 2017;44:143-146. https://dolorg/10.1016/j.seizure.2016.11.029 [ Links ]
8. Gastaut HJ, Bert J. EEG changes during cinematographic presentation; moving picture activation of the EEG. Electroencephalogr Clin Neurophysiol 1954;6(3):433-444. https://doi.org/10.1016/0013-4694(54)90058-9 [ Links ]
9. Velis D, Plouin P, Gotman J, et al. Recommendations regarding the requirements and applications for long-term recordings in epilepsy. Epilepsia 2007;48(2):379-384. https://doi.org/10.1111/j.1528-1167.2007.00920.x [ Links ]
10. Hingray C, El-Hage W, Duncan R, et al Access to diagnostic and therapeutic facilities for psychogenic nonepileptic seizures: An international survey by the ILAE PNES Task Force. Epilepsia 2018;59(1):203-214. 2017/11/20. https://doi.org/10.1111/epi.13952 [ Links ]
11. Wirrell EC, Grinspan ZM, Knupp KG, et al Care delivery for children with epilepsy during the COVID-19 pandemic: An international survey of clinicians. J Child Neurol 2020;35(13):924-933. https://doi.org/10.1177/0883073820940189 [ Links ]
12. Ojeda J, Gutierrez G, Del Rio Villegas R, et al. Utility of home-made videos in an adult epilepsy clinic. J Neurol Dis 2016;4(7):311. https://doi.org/10.4172/2329-6895.1000311 [ Links ]
13. Dash D, Sharma A, Yuvraj K, et al. Can home video facilitate diagnosis of epilepsy type in a developing country? Epilepsy Res 2016;125:19-23. https://doi.org/10.1016/j.eplepsyres.2016.04.004 [ Links ]
14. Huang LL, Wang YY, Liu LY, et al Home videos as a cost-effective tool for the diagnosis of paroxysmal events in infants: Prospective study. JMIR Mhealth Uhealth 2019;7(9):e11229. https://doi.org/10.2196/11229 [ Links ]
15. Amin U, Primiani CT, MacIver S, et al. Value of smartphone videos for diagnosis of seizures: Everyone owns half an epilepsy monitoring unit. Epilepsia 2021;62(9):e135-e139. https://doi.org/10.1111/epi.17001 [ Links ]
16. Tatum WO, Hirsch LJ, Gelfand MA, et al. Video quality using outpatient smartphone videos in epilepsy: Results from the OSmartViE study. Eur J Neurol 2021;28(5):1453-1462. https://doi.org/10.1111/ene.14744. [ Links ]
17. Tatum WO, Hirsch LJ, Gelfand MA, et al. Assessment of the predictive value of outpatient smartphone videos for diagnosis of epileptic seizures. JAMA Neurol 2020;77(5):593-600.https://doi.org/10.1001/jamaneurol.2019.4785 [ Links ]
18. Ramanujam B, Dash D, Tripathi M. Can home videos made on smartphones complement video-EEG in diagnosing psychogenic nonepileptic seizures? Seizure 2018;62:95-98. https://doi.org/10.1016/j.seizure.2018.10.003. [ Links ]
19. Karakas C, Modiano Y, Van Ness PC, et al. Home video prediction of epileptic vs. nonepileptic seizures in US veterans. Epilepsy Behav 2021;117:107811. https://doi.org/10.1016/j.yebeh.2021.107811 [ Links ]
20. Chen DK, Graber KD, Anderson CT, et al. Sensitivity and specificity of video alone versus electroencephalography alone for the diagnosis of partial seizures. Epilepsy Behav 2008;13(1):115-118. https://doi.org/10.1016/j.yebeh.2008.02.018 [ Links ]
21. Erba G, Giussani G, Juersivich A, et al. The semiology of psychogenic nonepileptic seizures revisited: Can video alone predict the diagnosis? Preliminary data from a prospective feasibility study. Epilepsia 2016;57(5):777-785. https://doi.org/10.1111/epi.13351 [ Links ]
22. Beniczky SA, Fogarasi A, Neufeld M, et al. Seizure semiology inferred from clinical descriptions and from video recordings. How accurate are they? Epilepsy Behav 2012;24(2):213-215. https://doi.org/10.1016/j.yebeh.2012.03.036 [ Links ]
23. Goodwin E, Kandler RH, Alix JJ. The value of home video with ambulatory EEG: A prospective service review. Seizure 2014;23(6):480-482. https://doi.org/10.1016/j.seizure.2014.02.008. [ Links ]
24. Samuel M, Duncan JS. Use of the hand held video camcorder in the evaluation of seizures. J Neurol Neurosurg Psychiatr 1994;57(11):1417-1418. https://doi.org/10.1136/jnnp.57.11.1417 [ Links ]
25. Wasserman D, Herskovitz M. Epileptic vs psychogenic nonepileptic seizures: A video-based survey. Epilepsy Behav 2017;73:42-45. https://doi.org/10.1016/j.yebeh.2017.04.020 [ Links ]
26. Meinardi H, Scott RA, Reis R, et al. The treatment gap in epilepsy: The current situation and ways forward. Epilepsia 2001;42(1):136-149. [ Links ]
27. Ngugi AK, Bottomley C, Kleinschmidt I, et al. Estimation of the burden of active and life-time epilepsy: A meta-analytic approach. Epilepsia 2010;51(5):883-890. https://doi.org/10.1111/j.1528-1167.2009.02481.x [ Links ]
28. Brodie MJ, Barry SJ, Bamagous GA, et al. Patterns of treatment response in newly diagnosed epilepsy. Neurology 2012;78(20):1548-1554. https://doi.org/10.1212/WNL.0b013e3182563b19 [ Links ]
29. Mannan JB, Wieshmann UC. How accurate are witness descriptions of epileptic seizures? Seizure 2003;12(7):444-447. https://doi.org/10.1016/s1059-1311(03)00052-9 [ Links ]
30. Leach JP, Lauder R, Nicolson A, et al. Epilepsy in the UK: Misdiagnosis, mistreatment, and undertreatment? The Wrexham area epilepsy project. Seizure 2005;14(7):514-520. https://doi.org/10.1016/j.seizure.2005.08.008 [ Links ]
31. Uldall P, Alving J, Hansen LK, et al. The misdiagnosis of epilepsy in children admitted to a tertiary epilepsy centre with paroxysmal events. Arch Dis Childhood 2006;91(3):219-221. https://doi.org/10.1136/adc.2004.064477 [ Links ]
32. Elger CE, Hoppe C. Diagnostic challenges in epilepsy: Seizure under-reporting and seizure detection. Lancet Neurol 2018;17(3):279-288. https://doi.org/10.1016/S1474-4422(18)30038-3 [ Links ]
33. Muayqil TA, Alanazy MH, Almalak HM, et al Accuracy of seizure semiology obtained from first-time seizure witnesses. BMC Neurol 2018;18(1):135. https://doi.org/10.1186/s12883-018-1137-x [ Links ]
34. Heo JH, Kim DW, Lee SY, et al. Reliability of semiology description. Neurologist 2008;14(1):7-11. https://doi.org/10.1097/NRL.0b013e3181343cb4 [ Links ]
35. Benbir G, Demiray DY, Delil S, et al. Interobserver variability of seizure semiology between two neurologist and caregivers. Seizure 2013;22(7):548-552. https://doi.org/10.1016/j.seizure.2013.04.001 [ Links ]
36. Rugg-Gunn FJ, Harrison NA, Duncan JS. Evaluation of the accuracy of seizure descriptions by the relatives of patients with epilepsy. Epilepsy Res 2001;43(3):193-199. https://doi.org/10.1016/s0920-1211(00)00209-6 [ Links ]
37. Van de Vel A, Cuppens K, Bonroy B, et al. Long-term home monitoring of hypermotor seizures by patient-worn accelerometers. Epilepsy Behav 2013;26(1):118-125. https://doi.org/10.1016/j.yebeh.2012.10.006 [ Links ]
38. Fisher RS, Blum DE, DiVentura B, et al. Seizure diaries for clinical research and practice: Limitations and future prospects. Epilepsy Behav 2012;24(3):304-310. https://doi.org/10.1016/j.yebeh.2012.04.128 [ Links ]
39. Williams JA, Cisse FA, Schaekermann M, et al. Smartphone EEG and remote online interpretation for children with epilepsy in the Republic of Guinea: Quality, characteristics, and practice implications. Seizure 2019;71:93-99. https://doi.org/10.1016/j.seizure.2019.05.025 [ Links ]
40. Chapman Smith SN, Govindarajan P, Padrick MM, et al A low-cost, tablet-based option for prehospital neurologic assessment: The iTREAT Study. Neurology 2016;87(1):19-26. https://doi.org/10.1212/wnl.0000000000002799 [ Links ]
41. Drummond L, Brunnhuber F. 'There's no place like home' - a prospective control study of home video telemetry versus inpatient video telemetry at Kings College Hospital. Abstract. Epilepsia 2009;50(Suppl 4):S125. [ Links ]
42. Kandler R, Ponnusamy A, Wragg C. Video ambulatory EEG: A good alternative to inpatient video telemetry? Seizure 2017;47:66-70. https://doi.org/10.1016/j.seizure.2017.02.010 [ Links ]
43. Lawley A, Evans S, Manfredonia F, et al The role of outpatient ambulatory electroencephalography in the diagnosis and management of adults with epilepsy or nonepileptic attack disorder: A systematic literature review. Epilepsy Behav 2015;53:26-30. https://doi.org/10.1016/j.yebeh.2015.09.032 [ Links ]
44. Patel AC, Thornton RC, Mitchell TN, et al. Advances in EEG: Home video telemetry, high frequency oscillations and electrical source imaging. J Neurology 2016;263(10):2139-2144. Article. https://doi.org/10.1007/s00415-016-8159-3 [ Links ]
45. Zeiler SR, Kaplan PW. Our digital world: Camera phones and the diagnosis of a seizure. Lancet 2009;373(9681):2136. https://doi.org/10.1016/S0140-6736(09)60304-4 [ Links ]
46. Jory C, Shankar R, Coker D, et al. Safe and sound? A systematic literature review of seizure detection methods for personal use. Seizure 2016;36: 4-15. https://doi.org/10.1016/j.seizure.2016.01.013 [ Links ]
47. Vital Wave Consulting. mHealth for Development: The opportunity of mobile technology for healthcare in the developing world. Washington, DC: United Nations Foundation, Vodafone Foundation, 2009. http://www.globalproblems-globalsolutions-files.org/unf_website/assets/publications/technology/ mhealth/mHealth_for_Development_full.pdf (accessed 30 November 2022). [ Links ]
48. Poushter J, Bishop C, Chwe H. Social media use continues to rise in developing countries, but plateaus across developed ones. Washington, DC: Pew Research Center, 2018. https://www.pewresearch.org/global/2018/06/19/social-media-use-continues-to-rise-in-developing-countries-but-plateaus-across-developed-ones/ (accessed 5 December 2022). [ Links ]
 Correspondence:
Correspondence:
J M Wilmshurst
Jo.wilmshurst@uct.ac.za
Accepted 9 September 2022.














