Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.1 Pretoria Jan. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i1.16680
RESEARCH
Access to postpartum tubal ligation services in Cape Town, South Africa - an observational study
M VorsterI; G PetroII; M PatelIII
IMB ChB; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Cape Town, South Africa
IIMB ChB, FCOG (SA); Department of Obstetrics and Gynaecology, New Somerset Hospital, University of Cape Town, South Africa
IIIFCOG (SA), Cert Reproductive Medicine (SA)FCOG (SA), Cert Reproductive Medicine (SA); Reproductive Health and Fertility Regulation, Department of Obstetrics and Gynaecology, Groote Schuur Hospital and University of Cape Town, South Africa
ABSTRACT
BACKGROUND. Many women receiving antenatal care in public health services in Cape Town choose bilateral tubal ligation as their preferred method of postpartum contraception during their antenatal course. If the sterilisation does not occur immediately, these women are discharged on an alternative form of contraception and, ideally, an interval date for bilateral tubal ligation is arranged.
OBJECTIVES. To assess the access to tubal ligation services in the Metro West area of Cape Town, South Africa, in women who request permanent contraception following delivery, looking specifically at the number of women requesting bilateral tubal ligation who receive the procedure intrapartum, immediately postpartum or as an interval procedure. Other objectives included determining the reproductive outcomes if bilateral tubal ligation was not performed, investigating the alternative forms of contraception provided and to study the demographics of the population requesting bilateral tubal ligation as a form of contraception.
METHODS. The study was conducted as a cross-sectional observational study collecting data over a period of 3 months, from June 2019 to August 2019. Maternity case records for deliveries between June 2019 and August 2019 from four facilities were reviewed. The facilities, representing all levels of care, were Vanguard Midwife Obstetric Unit, Wesfleur Hospital (district hospital), New Somerset Hospital (regional hospital), Groote Schuur Hospital (tertiary hospital).
RESULTS. There were 260 women who requested tubal ligation as their choice of contraception. Only 50% of these received a tubal ligation. Of the 131 tubal ligations performed, 2 were interval sterilisations. Ninety-one percent (120/131) of the tubal ligations were done at the time of caesarean section. Of the 129 women who received alternative forms of contraception, 13 women had a recurrent pregnancy.
CONCLUSION. The study suggests that only 50% of women requesting tubal ligation as form of contraception actually end up receiving the procedure. Alternative forms of contraception are widely used and relied upon, but not without risks of recurrent pregnancy. Interval tubal ligation was not easily accessed by those women who were referred for the procedure.
Women's health is a topic that is receiving much interest worldwide. Reproductive health and contraception make up part of women's health. Availability of and access to contraception is a global matter of importance.
The unmet need for family planning is defined as the proportion of women who are fecund who want to terminate or postpone childbearing, but who are not using a contraceptive method.[1] Estimated data from low- and middle-income countries, which include South Africa (SA), showed that in 2019, out of 923 million women of reproductive age in these countries who wanted to avoid having a pregnancy, 218 million had an unmet need for modern contraception -that is, they wanted to avoid a pregnancy but were not using a modern method. The proportion of women with unmet need for contraception in 2012 was 53% in Africa, and 17% in southern Africa.[2]
The contraceptive prevalence rate (CPR) is defined as the percentage of women of childbearing age using any form of contraception at a given point in time.[3] The CPR in SA in 2010 was 63.7%. In comparison, the CPR for the whole of the African continent was much lower, at 30.9%. The SA CPR, in turn, was much lower compared with upper-middle-income countries such as Brazil (79.5%) or Russia (78.6%).[4,5]
The Millennium Development Goals (MDGs) set in 2000 included universal access to sexual and reproductive health, highlighting its importance, specifically with regard to improving women's health and well-being. Improving women's health contributes to a country's economic growth and development.[6,7] Progress made towards reaching the MDG was assessed in 2015. Results showed that contraception use among women in sub-Saharan Africa in the age group 15 - 49 years had more than doubled since 1990, yet an unmet need for contraception remained in 24% of these women.[8-]
In response to what was deemed a lack of sufficient progress towards the MDG, the Sustainable Development Goals were set in place in 2015 - which included universal access to sexual and reproductive health.[9]
The SA government made a pledge at the Family Planning London Summit in 2012 to prioritise the need to strengthen family planning services. The aim would be that the full range of family planning services would be made available to patients at public health facilities.[5]
The contraceptive use of SA women specifically was last studied and published in 2003, in the SA Demographic and Health Survey.'10- The most commonly used form of contraceptive was injectables - 53% of all women using contraception at the time were using injectables. At the time, only 7.3% of all SA women aged 15 - 49 years had tubal ligation or sterilisation as their contraceptive method.
Data derived from the 2012 SA National HIV Prevalence, Incidence and Behaviour Survey[11] showed that 8.1% of SA women of childbearing age were sterilised.
An unmet need for contraception leads to unintended pregnancies. The SA National HIV Prevalence, Incidence and Behaviour Survey showed that ~50% of pregnancies at the time were unplanned. The rate of unintended pregnancies in women aged >35 years was 44.9%.[12] Unintended pregnancies have a negative effect on the health, social and economic systems of countries.[13]
Adequate family planning methods, such as sterilisation, can directly reduce the maternal mortality rate. Preventing unplanned pregnancies reduces the risk of early pregnancy complications and unsafe abortions.[14] Thirteen percent of the annual global maternal mortality results from complications of unsafe abortions.[15] Studies from Bangladesh show that maternal deaths can be reduced by 26% if grandmultiparous women of advanced maternal age were sterilised.[16]
In order to decrease maternal mortality and reduce unintended pregnancies, barriers to the uptake of sterilisation should be addressed. Ongoing counselling and education prevent misinformation, misconceptions and fear of side-effects as a cause for poor uptake of family planning.[17] Sterilisation includes bilateral tubal ligation (BTL) and vasectomy. It is an option for couples who have completed their family and want permanent contraception.
The Cairo Declaration[18] on population development issued in 1994 states that all barriers preventing access to family planning services should be addressed and removed while recognising international human rights. The 1995 Beijing Declaration and Platform for Action[19-aim to promote gender equality and women's rights. The human rights of women include their freedom to decide responsibly on matters relating to their sexuality and reproductive health, free from discrimination, violence and coercion. Patients should not be coerced into signing consent for a sterilisation. India and other countries such as SA, Namibia and Chile have abused forced sterilisation as a form of population control and prevention of HIV transmission.[20,21] Informed consent should be obtained - the patient must be given accurate, adequate and understandable information. The person taking consent should be open to questions and further explanation of the procedure. The patient should feel free to make a voluntary choice, which includes refusal of treatment.[22]
Current barriers to these forms of contraception may include accessing services. Patients should have adequate access to tubal ligation services. This includes adequate information on where to access these services and referral to relevant facilities.[23] Training more healthcare providers and having more healthcare facilities provide sterilisation services will increase the uptake thereof.[10,24]
Some women receiving antenatal care in Metro West choose BTL as form of contraception during their pregnancy. Not all of these women receive their tubal ligation. Different levels of healthcare facilities offer different methods of immediate postpartum contraception. Primary healthcare facilities such as Midwife Obstetric Units (MOUs) do not have the staff or infrastructure to offer immediate postpartum tubal ligation services. Patients requesting BTL who deliver at primary healthcare facilities should be referred to secondary-level centres for their interval sterilisation. Immediate postpartum tubal ligation can be performed at secondary-level facilities either at the time of caesarean delivery or as a postpartum procedure prior to discharge. If the sterilisation does not occur immediately, these women are discharged on an alternative form of contraceptive, and ideally, an interval BTL date is given.
In the Metro West area of Cape Town, there are currently no data available on:
• how many women receive the requested BTL
• the number of women who have recurrent pregnancies if the BTL was not done
• the alternative forms of contraception women received if BTL was not performed.
The aim of this study is to assess the access to tubal ligation services in the Western subdistrict of Metro West in women who request permanent contraception following delivery. The objectives were:
• to assess the demographics of the population requesting BTL as form of contraception
• to determine the number of women requesting BTL who received the procedure at the time of caesarean section, immediately postpartum or as an interval procedure
• to determine the reproductive outcomes if BTL was not performed, including early pregnancy complication or termination of pregnancy
• to investigate alternative forms of contraception provided.
Methods
Ethics approval for the study was granted by University of Cape Town, Faculty of Health Sciences, Human Research Ethics Committee (ref. no. HREC REF 485/2021).
The study was conducted as a cross-sectional observational study, collecting data from June 2019 to August 2019. Maternity case records (MCRs) for deliveries between June 2019 and August 2019 from four facilities were reviewed: Vanguard MOU (VGMOU), Wesfleur Hospital (WFH; district hospital), New Somerset Hospital (NSH; regional hospital) and Groote Schuur Hospital (GSH; tertiary hospital). These facilities serve a large area of the Metro West district and include high- and low-risk pregnancies. Metro West is a large urban area around Cape Town with a population of 4 801 000. The annual delivery data from Metro West reports 3 500 deliveries at GSH, 6 400 at NSH, 1 800 at WFH and 1 300 at VGMOU. These facilities were chosen in order to represent different levels of care.
VGMOU manages low-risk deliveries - they do not have theatre facilities onsite. WFH manages low-risk pregnancies at a district level -the hospital has a theatre onsite to do emergency caesarean sections, but refers high-risk patients to NSH. NSH manages higher-risk pregnancies and deliveries at a secondary-level hospital and accepts referrals from VGMOU and other MOUs in the area. Referral criteria to NSH include: teenage pregnancies; advanced maternal age; impaired glucose tolerance; high body mass index (BMI >35 but <50); previous caesarean section; chronic hypertension; gestational proteinuric hypertension (>34 weeks' gestation); uncomplicated twin pregnancy; placenta praevia minor; preterm labour (>32 weeks); prolonged rupture of membranes (>32 weeks); abruptio placenta with a live baby; failure to progress; cephalopelvic disproportion; cord prolapse; breech presentation; and other common obstetric complications. GSH is a tertiary hospital and manages high-risk pregnancies and deliveries. They accept referrals from VGMOU and NSH and other facilities in Metro West. Patients typically managed at GSH include: high BMI (>50); multiple gestations (monochorionic, growth restriction); placenta praevia major; autoimmune conditions; cardiac conditions; thyroid disease; gestational proteinuric hypertension (<34 weeks); eclampsia; abruption with intrauterine fetal demise; preterm labour (<32 weeks); preterm rupture of membranes (<32 weeks); previous early-onset pre-eclampsia; poorly controlled asthma; gestational diabetes; chronic diabetes; and epilepsy.
VGMOU does not offer tubal ligation services. These patients need to be referred specifically to NSH for interval tubal ligations. This involves a referral letter to the facility, and depends on the patient's attendance of a clinic date. Postpartum tubal ligation services are offered at WFH, NSH and GSH, although this is often not done due to bed constraints, shortage of personnel and limited theatre time. Other contraindications to surgery and anaesthesia are also taken into account, e.g. obesity, severe gestational proteinuric hypertension, chorioamnionitis and anaemia.
MCRs of women who delivered at the four designated sites between June 2019 and August 2019 were reviewed. Data collection was done between October 2021 and January 2022. Only women who selected tubal ligation as a form of contraception were included in the study. We used a convenience sample size over a period of 3 months. The data collected gave us an adequate sample size.
From clinical experience, about 5% of women request tubal ligation during their antenatal care. We anticipated that this would give us a sample size of 160.
Page 10 of the MCR is completed by the healthcare worker attending to the patient at her booking visit. The majority of booking visits are done at local clinics with basic antenatal care facilities, or at MOUs. The preferred method of contraception is discussed at this time. Midwives are trained to do contraceptive counselling in line with the Royal College of Obstetricians and Gynaecologists Best Practice Papers,[25] although the exact method of counselling is not documented in the MCR. On follow-up visits, contraception is often re-discussed (especially when referred to a higher level of care). Changes regarding the choice of contraception should preferably be documented on page 10, although it is common to only find this information in the clinical notes on closer inspection of the MCR. The researcher and one research assistant reviewed only page 10 of the MCR and the discharge summary page.
The discharge page of the MCR indicated whether the patient received her primary form of contraception at the time of discharge. The hospital numbers of women who did not receive a tubal ligation immediately post delivery were collected. These numbers were then inserted into Clinicom (the Western Cape Department of Health provincial patient data management system) to detect whether the patient visited any healthcare centre in the Western Cape to receive an interval tubal ligation, evacuation of the uterus or termination of pregnancy. Clinicom can be accessed at any governmental healthcare facility in the Western Cape. Specific codes are allocated to specific procedures. Hospital numbers of the study population were entered into the Clinicom system and correlated with these specific codes. This process was done in January 2022, just before write-up of the results, in order to maximise the time window during which patients could present for management of subsequent pregnancies or interval tubal ligation. The hospital numbers were also inserted into LabTrack (National Health Laboratory Service, SA) to see whether a laboratory cascade of booking bloods (haemoglobin, Rhesus, rapid plasma reagent) were collected after the date of discharge - which likely indicates a recurrent pregnancy.
The inclusion criteria were women who requested tubal ligation as choice of contraception in their MCR (page 10) for deliveries between June 2019 and August 2019 at the four facilities - VGMOU, WFH, NSH, GSH. Exclusion criteria were women not requesting tubal ligation as contraception in their MCR for deliveries between June 2019 and August 2019.
Results
The birth registers from the facilities showed the following number of deliveries between June 2019 and August 2019: VGMOU 149; WFH 234; NSH 1 722; GSH 504.
The number of files that were available for review at each of these facilities was: VGMOU 109; WFH 120; NSH 1635; GSH 480.
Table 1 shows the number of deliveries, files reviewed and women requesting BTL at each facility.

The study population included women aged between 25 and 46 years, with a mean age of 34 years (Table 2). Almost half the population (49.6%, 129/260) were women of advanced maternal age (>35 years). The women included in the study had between 0 and 9 children, with a median parity of 3. Twenty-seven women (10.3%) were grandmultiparous (≥ 5 children).

Only half the women who requested tubal ligation as their choice of contraception received the procedure, as seen in Figs 1 and 2: of the 260 women included in the study, 129 women received a tubal ligation at the time of discharge. Two women received interval sterilisations. Alternative methods of contraception were used in 115 (87%) of the remaining 131 women. Injectables were the most common form of alternative contraception (83/115), followed by Implanon (18/115) and intrauterine contraceptive device (10/115). Sixteen women were discharged without contraception.
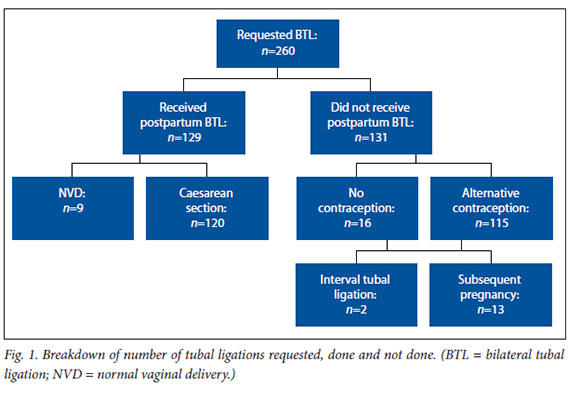

Of the group of women who received alternative forms of contraception or no contraception, 13 (9.9%) women had recurrent pregnancies, with the following outcomes: 6 deliveries, 2 miscarriages requiring an evacuation of the uterus, 2 ectopic pregnancies and 3 terminations of pregnancy.
The mode of delivery plays a role in whether a tubal ligation isdone - <10% of women who had normal vaginal deliveries received a tubal ligation, while 82% of women who delivered via caesarean section received a tubal ligation as requested. This is shown in Fig. 3.

Fifty-seven percent (74/129) of women who received a tubal ligation were of advanced maternal age, and 10% (14/129) were grandmultiparous (14/129). The only tubal ligation done at GSH after a normal vaginal delivery was for a 39-year-old grandmultiparous woman.
Fifty-nine percent (16/27) of grandmultiparous women delivered vaginally. Of these 16 women, only 3 (18.7%) received a tubal ligation. The remaining 11 grandmultiparous women who delivered via caesarean section (7 emergency and 4 elective) all received a tubal ligation (Fig. 4).

Nine of 115 (7.83%) women who delivered vaginally received their tubal ligation at the time of discharge. Forty-eight of 59 (81.3%) women who had emergency caesarean sections received a tubal ligation, while 72 of 86 (83.7%) women who had elective caesarean sections received a tubal ligation.
No data are available on the overall number of women who were referred for an interval tubal ligation.
Discussion
VGMOU was included in the study to demonstrate that not all facilities have the infrastructure to provide postpartum tubal ligations. This facility only manages vaginal deliveries and has no theatre facilities onsite. None of the thirteen women (5% of the study population) who delivered at this facility received a tubal ligation. These women would have required referral to NSH, which offers interval sterilisation services. While the other facilities included in the study do offer tubal ligation
services, only 9 women of 102 who had normal vaginal deliveries at these facilities (WFH, NSH, GSH) received a tubal ligation. This may be due to limited theatre time, as 58% of deliveries at these facilities are via caesarean section. Postpartum tubal ligations are often delayed by hours or even days because of theatres constantly being used for elective and emergency caesarean sections. NSH has a single obstetric operating theatre for elective and emergency caesarean sections. This is the same theatre where postpartum tubal ligations take place. Patients who deliver vaginally are typically discharged from the hospital or MOU within 6 - 24 hours after delivery. The delay in access to theatre often leads to the patients changing their minds regarding tubal ligation.
Of the 9 women who received a tubal ligation following a normal vaginal delivery, 4 (44%) were of advanced maternal age and 3 (33%) were grandmultiparous. Fifty-nine percent (16/27) of grandmultiparous women delivered vaginally, and subsequently the majority of these women (13/16) did not receive a tubal ligation, while we feel that these are the women who should be prioritised for tubal ligations.
Of the 145 women in the study who delivered via caesarean section, only 120 received a tubal ligation at the time of delivery. Many factors could be responsible for this discrepancy. Factors leading to alternative choice of contraception include: patient age; pregnancy outcome; change in fertility desires, etc.; and understanding permanence of procedure when taking informed consent for caesarean section and tubal ligation.
Suggestions to improve access to postpartum tubal ligations include organising sterilisation drives where doctors working in obstetrics and gynaecology run a dedicated tubal ligation theatre list on a monthly basis. Access to interval tubal ligations can possibly be improved using appropriate referral systems such as the VULA platform. We plan on presenting the findings to local stakeholders to highlight the lack of access and subsequent unplanned pregnancies in a bid to find solutions.
Limitations of the study include the fact that this is not a representation of all the facilities in Metro West. Page 10 of the MCR does not indicate the counselling process regarding choice of contraceptive - this may reflect the healthcare worker's suggestion of the most appropriate form of contraception instead of the patient's preferred method. However, the aim of the study was not to assess contraceptive counselling. Reasons for not receiving a tubal ligation in women who delivered at facilities that offer these services were not identified. Women who did not receive a tubal ligation at the time of delivery might have migrated to other provinces in the country, therefore interval sterilisations might have been received in other provinces or even in private healthcare facilities - the details of these patients would not be seen on Clinicom. COVID lockdowns may have affected access to interval sterilisations, as these procedures are seen as elective surgical services and may have been postponed indefinitely.
Conclusion
The study shows that there are barriers to access to tubal ligation services in Metro West. The majority of women who deliver via normal vaginal deliveries do not receive a tubal ligation at the time of delivery. Alternative methods of contraception are offered, and the uptake of alternative methods is acceptable. Interval sterilisations are seldom accessed. Unplanned pregnancies are a consequence of lack of access to tubal ligations.
Declaration. This study formed MV's MMed research.
Acknowledgements. We acknowledge the clerks at the various facilities who helped with obtaining MCRs. We also acknowledge Alwyn Burger for giving professional writing advice.
Author contributions. MP and GP were responsible for the conception and design of the study. MV was responsible for data collection, interpretation and drafting of the work. GP was involved in the interpretation of the data. MP and GP revised and approved the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. USAID Data for Impact. Unmet need for family planning. North Carolina: Data for Impact Project, 2013 (updated 2022). https://www.data4impactproject.org/prh/family-planning/fp/unmetneed-for-family-planning/ (accessed 15 July 2021). [ Links ]
2. Darroch JE, Singh S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys. Lancet 2013;381(9879):1756-1762. https://doi.org/10.1016/S0140-6736(13)60597-8 [ Links ]
3. USAID Data for Impact. Contraceptive Prevalence Rate. North Carolina: Data for Impact Project, 2013 (updated 2022). http://www.cpc.unc.edu/measure/prh/rh_indicators/specific/fp/cpr (accessed 6 January 2016). [ Links ]
4. Alkema L, Kantorova V, Menozzi C, Biddlecom A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: A systematic and comprehensive analysis. Lancet 2013;381:1642-1652. [ Links ]
5. National Department of Health, South Africa. National contraception and fertility planning policy and service delivery guidelines. Pretoria: NDoH, 2012. [ Links ]
6. United Nations. The Millennium Development Goals Report 2015. New York: UN, 2015. [ Links ]
7. Olakunde BO, Sam-Agudu NA, Patel TY, et al. Uptake of permanent contraception among women in sub-Saharan Africa: A literature review of barriers and facilitators. Contraception 2019;99(4):205-211. [ Links ]
8. Guttmacher Institute. Adding it up: Investing in contraception and maternal and newborn health. New York: Guttmacher Institute, 2019. https://www.guttmacher.org/fact-sheet/addingit-up-contraceptionmnh-2017 (accessed 15 December 2018). [ Links ]
9. United Nations Department of Economic and Social Affairs. Sustainable Development Goals. Sustainable Development Knowledge Platform. New York: DESA, 2015. https://sustainabledevelopment.un.org/topics (accessed 26 November 2015). [ Links ]
10. National Department of Health, South African Medical Research Council, ORCMacro. South Africa Demographic and Health Survey 2003. Pretoria: NDoH, 2007. [ Links ]
11. Shisana O, Rehle T, Simbayi L, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press, 2014. [ Links ]
12. Chersich MF, Wabiri N, Risher K, et al. Contraception coverage and methods used among women in South Africa: A national household survey. S Afr Med J 2017;107(4):307-314. https://doi.org/10.7196/SAMJ.2017.v107i4.12141 [ Links ]
13. Makhathini BS, Makinga PN, Green-Thompson RR. Knowledge, attitudes, and perceptions of antenatal women to postpartum bilateral tubal ligation at Greys Hospital, KwaZulu-Natal, South Africa. Afr Health Sci 2019;19(3):2615-2622. https://doi.org/10.4314/ahs.v19i3.37 [ Links ]
14. World Health Organization. Unsafe abortion: Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. Geneva: WHO, 2011. [ Links ]
15. Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: An analysis of 172 countries. Lancet 2012;380(9837):111-125. [ Links ]
16. Fortney JA. The importance of family planning in reducing maternal mortality. Stud Fam Plann 1987;18(2):109-114. [ Links ]
17. Campbell M, Sahin-Hodoglugil NN, Potts M. Barriers to fertility regulation: A review of the literature. Stud Fam Plann 2006;37(2):87-98. [ Links ]
18. United Nations Population Information Network. Cairo Declaration on Population and Development, ICPPD. Cairo: UNFPA, 1994. https://www.unfpa.org/sites/default/files/resource-pdf/94-09-04_Cairo_Declaration_on_Population_Development_ICPPD.pdf (accessed 15 July 2021). [ Links ]
19. UN Women. Beijing Declaration and Platform for Action. Beijing: UN Women, 1995. http://www.pdic.gov.ph/files/gad/International%20GAD%20Treaties/DigitalLibrary. International%20GAD%20Treaties.Beijing%20Decla ration%20and%20Platform%20for%20Action.pdf (accessed 12 July 2021). [ Links ]
20. Bi S, Klusty T. Forced sterilisations of HIV-positive women: A global ethics and policy failure. AMA J Ethics 2015;17(10):952-957. https://doi.org/10.1001/journalofethics.2015.17.10.pfor2-1510 [ Links ]
21. Gupte PR. India: 'The Emergency' and the politics of mass sterilisation. Educ About Asia 2017;22(3):40-44. [ Links ]
22. ACOG Committee. Informed consent and shared decision making in obstetrics and gynecology. Obstetr Gynecol 2021;137(2)392-393. https://doi.org/10.1097/AOG.0000000000004248 [ Links ]
23. Hoke T, Harries J, Crede S, et al. Expanding contraceptive options for PMTCT clients: A mixed methods implementation study in Cape Town, South Africa. Reprod Health 2014;11:3. [ Links ]
24. Babalola S, John N. Factors Underlying the Use of Long-Acting and Permanent Family Planning Methods in Nigeria: A Qualitative Study. New York: EngenderHealth/The RESPOND Project, 2012. [ Links ]
25. Royal College of Obstetricians and Gynaecologists. Best practice in postpartum family planning. Best Practice Paper No 1. London: RCOG, June 2015. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/bpp (accessed 1 March 2019). [ Links ]
 Correspondence:
Correspondence:
M Vorster
mvorster0610@gmail.com
Accepted 22 August 2022














