Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.1 Pretoria Jan. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i1.16700
RESEARCH
A doctor at a PHC clinic: A 'must-have' or 'nice-to-have'?
T P KerryI; P G T CudahyII, III; H L HolstIV; A RamsunderV; N G McGrathVI
IMFamMed; District Clinical Specialist Team, uMgungundlovu District, KwaZulu-Natal, South Africa
IIMD; Section of Infectious Disease, Department of Medicine, Yale School of Medicine, New Haven, USA
IIIMD; Department of Internal Medicine, Harry Gwala Regional Hospital, Pietermaritzburg, South Africa
IVMD, MBA; uMgungundlovu District, South Africa
VMB ChB; Northdale Hospital, Pietermaritzburg, South Africa
VIMBBS; Department of Anatomical Pathology, University of Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Many patients have their healthcare needs met at primary healthcare (PHC) clinics in KwaZulu-Natal (KZN), without having to travel to a hospital. Doctors form part of the teams at many PHC clinics throughout KZN, offering a decentralised medical service in a PHC clinic.
OBJECTIVES. To assess the benefit of having a medical doctor managing patients with more complex clinical conditions at PHC clinic level in uMgungundlovu District, KZN. Two key questions were researched: (i) were the patients whom the clinic doctors managed of sufficient clinical complexity that they warranted a doctor managing them, rather than a PHC nurse clinician? and (ii) what was the spectrum of medical conditions that the clinic doctors managed?
METHODS. Doctors collected data at all medical consultations in PHC clinics in uMgungundlovu during February 2020. A single-page standardised data tool was used to collect data at every consultation.
RESULTS. Thirty-five doctors were working in 45 PHC clinics in February 2020. Twenty-six of the clinic doctors were National Health Insurance (NHI)-employed. The 35 doctors conducted 7 424 patient consultations in February. Staff in the PHC clinics conducted 143 421 consultations that month, mostly by PHC nurse clinicians. The doctors concluded that 6 947 (93.6%) of the 7 424 doctor consultations were of sufficient complexity as to warrant management by a doctor. The spectrum of medical conditions was as follows: (i) consultations for maternal and child health; n=761 (10.2%); (ii) consultations involving non-communicable diseases (NCDs), n=4 372 (58.9%) - the six most common NCDs were, in order: hypertension, diabetes, arthritis, epilepsy, mental illness and renal disease; (iii) consultations involving communicable diseases constituted 1 745 (23.5%) of cases; and (iv) consultations involving laboratory result interpretation 1 180 (15.9%).
CONCLUSION. This research showed that at a PHC clinic the more complex patient consultations did indeed require the skills and knowledge of a medical doctor managing these patients. These data support the benefit of a doctor working at every PHC clinic: the doctor is a 'must-have' member of the PHC clinic team, offering a regular, reliable and predictable medical service.
Many patients have their healthcare needs met at primary healthcare (PHC) clinics in KwaZulu-Natal (KZN), without having to travel to a hospital. This is the situation in uMgungundlovu District, which is situated around the city of Pietermaritzburg, and has clinics in urban as well as rural areas. There are many more clinics than hospitals, with clinics located throughout the geographic area, providing healthcare nearer to communities. The main pillars of strength of the PHC clinics are the teams of full-time, dedicated, well-trained and hard-working operational managers and PHC professional nurse clinicians (PNs). Medical doctors form only a part of these PHC clinic teams, but offer a decentralised medical service for patients with more complex clinical conditions. Doctors going to clinics in KZN have for many years worked as an outreach service from district hospitals, community health centres (CHCs) and district offices. There are currently two sources of doctors for the clinics - outreach doctors and National Health Insurance (NHI) doctors. However, there are no directly funded medical posts on the establishment of the PHC clinics in KZN. NHI introduced the concept of the general practitioner (GP) or general doctor working in the PHC clinic in 2013 in three pilot districts in KZN, including uMgungundlovu.[1]-NHI GP posts are renewed on a yearly contract basis.
This research has endeavoured to assess whether doctors are of benefit in a PHC clinic. Is a doctor at a PHC clinic a 'must-have' or just a 'nice-to-have' member of the team? To those doctors and PNs who work in PHC clinics, the answer is a resounding 'yes' that the doctors are a benefit and a 'must-have'. When the clinic operational managers in uMgungundlovu were interviewed using a provincial NHI monitoring form, they all without exception stated that the NHI doctors add benefit. Management of patients onsite at the PHC clinic has become more important over recent years, as busy hospitals can no longer manage all the patients with hypertension, diabetes and other chronic illnesses such as HIV. These patients are either cross-referred from hospital to a PHC clinic or initiated on treatment at the PHC clinic.
What work do doctors do in PHC clinics? Do they improve the package of care in a PHC clinic? Do they enable more patients to be cared for at a local level, without the need for referral to a sometimes faraway hospital? Doctors are trained to manage patients with undifferentiated presentations and complex medical conditions beyond the scope of the PN, such as chronic kidney disease or virological failure. Doctors can also initiate scheduled medicines beyond the scope of the PN; manage obstetric problems beyond basic antenatal care; manage child health problems not covered by integrated management of childhood illness (IMCI); perform more complex management of emergencies such as poison ingestion; perform minor surgical procedures; and interpret X-rays and laboratory results. Decentralised care by the doctors is convenient for the patients, who may not have money for public transport. The public health sector itself is facing challenges of dwindling financial resources.[2] Yet doctors should be deployed to where health needs occur, in communities situated close to PHC clinics. Hugo[3] likened community-orientated primary care (COPC) changing the 'game' of primary health to that of a soccer game. Disease and ill health exist in communities that are situated around the opponent's goal area. The soccer players (health workers) need to move onto the offensive and play the game closer to where the diseases occur.
In a key article published in 2009, support to PHC clinics by doctors in three districts in northern KZN was studied by Nkosi et al.[4] They found that the medical work mainly comprised review of chronic medication, attending to referred patients and staff training. The doctor visits were seen as a positive experience by nurses and doctors. Staff agreed that it was better for the same doctor to visit the same clinic regularly. The authors concluded that the doctor's role in a PHC clinic is underutilised; better teamwork is required; and hospital managers need to support the visiting doctors and give the clinic visits priority. In a recent article, Gaede[5] challenged the clinic doctor to go beyond just providing clinical services: Complex outreach at a PHC clinic should include activities such as clinical governance, mentoring and training. Mash et al.[6] found that primary care services at clinics and CHCs were struggling to cope with high patient numbers, the complexity of undifferentiated problems, multiple comorbidities and serious illnesses. Pillay et al.[7] reviewed the burden of diabetes in KZN, largely based on data from the District Health Information System (DHIS). In this same article, data specific to uMgungundlovu from 2010 to 2014 showed that >90% of 10 417 diabetic patients had their treatment started at PHC clinic level. The authors concluded that 'these clinics should receive increased staffing in the form of doctor support and nursing, which is the way forward envisaged by NHI'. In North West (NW) Province, the role of the visiting clinic doctor was studied in discussion with PHC nurses at clinics.[8] The authors concluded that 'the positive role of visiting doctors to clinics cannot be overemphasised.' The following recommendations were made: hospital or district management needs to be supportive, especially with regards to transport of the doctor to the clinic; the visiting doctor needs to be oriented to clinic work, and needs extra skills, such as working with mental healthcare users, knowledge of the Essential Medicine List (EML),[9] rational prescribing and knowledge of IMCI; a specific doctor should be allocated to a specific clinic long term; the doctor should display good relationships, mutual respect and teamwork. Tumbo et al.[10] examined the utilisation of three private GPs who had worked in PHC clinics in NW Province over several years. Many benefits were shown about this public-private partnership, such as satisfied patients, enhanced continuity of care, support of the staff by the GPs, committed long-term relationships, teaching by the GP and a strong sense of social obligation by the GPs to their local community.
Objective
Few studies, however, have quantified the benefit of a doctor working at a clinic, and what (s)he does in the clinic. Does a medical doctor working at a PHC clinic extend the package of care, so reducing the number of referrals to hospital? This research aimed to assess the benefit of having a medical doctor managing patients with more complex clinical conditions at the PHC clinic level in uMgungundlovu District, KZN. The results may provide motivation for securing and expanding the role of doctors in PHC clinics. The two objectives of the research were therefore as follows:
(i) firstly, to establish whether the patients whom the clinic doctors managed were of sufficient clinical complexity that they warranted a doctor managing them, as opposed to a PHC nurse clinician;
( ii) secondly, to obtain a snapshot of the spectrum of medical conditions that the clinic doctors managed.
Methods
Study design
We conducted a prospective, descriptive, cross-sectional study. The objectives of the study were met by designing and administering the 'doctor in PHC clinic data tool' (appendix https://www.samedical.org/file/1953). We documented what work the PHC doctors did in the PHC clinics of uMgungundlovu District during the whole of February 2020 (which was just days before the first patient with COVID-19 was diagnosed in uMgungundlovu, and in South Africa). One copy of the data tool was filled in after every consultation by the PHC doctors during February 2020. All doctor consultations for the month were included in the study, so as to give an accurate spectrum of the conditions managed.
Situations and conditions were chosen to maximise objectivity by the doctor in filling in the data tool, as follows:
( i) Certain medical conditions were by nature complex and beyond the scope of a PHC PN, e.g. management of thyroid disease, nephrology/urology or interpreting an X-ray.
(ii) Potentially complex conditions were named, such as hypertensive disorder of pregnancy or previous caesarean section.
( iii) Complex medical conditions were identified by the schedule of the medicine used to treat the patients, such as epilepsy, mental health problems, cardiac disease, second-line antiretroviral treatment (ART), etc. Such medicines are classified as 'doctor-initiated' in the PHC EML[9] or KZN Medicine Catalogue.[11]
(iv) The primary researcher had written an unpublished guide that has been in use for several years in the PHC clinics of the district, called 'Guide for PNs and doctors in PHC: Which patients to refer to the PHC clinic doctor'. This guide is based on the PHC EML[9] and Adult Primary Care booklet (APC) [12] The guide specifies which medical conditions should be managed by a doctor rather than a PHC PN. The guide was again given to the PHC doctors.
( v) Spectrum of medical conditions: the data tool identified 24 broad categories of consultation known to be common in PHC medical practice, such as emergencies, antenatal and child consultations, and adult consultations including communicable and non-communicable disease, administrative and chronic medicine-related consultations. If the condition did not fit into the more common categories, then there was a tick box for 'other medical or social conditions'.
Setting
In February 2020, 35 doctors were specifically employed to work in 45 PHC clinics in uMgungundlovu District. The three CHCs in the district, although classified as PHC facilities, were not included in this study, as CHCs have full-time posts for doctors in their establishments.
Participants
For the first objective, the research assessed the PHC doctors as participants, as they consulted with the primary care patients. All doctors were given the option not to participate in the research, without prejudice. For the second objective, the patients in each doctor consultation in the PHC clinic were the participants.
In KZN, PHC clinics follow the principle that the patient should first seek healthcare with the PHC PN. If the problem is beyond the skill or scope of the PN, then (s)he can refer the patient to the doctor. Booking diaries are used for elective bookings in PHC clinics. Elective bookings usually comprise between 70% and 80% of the work by the clinic doctors. The research identified the five ways by which patients could be booked for the doctor:
(i) The PN electively booked patients for the doctor's next available consultation day
(if) The doctors themselves booked certain patients for follow-up by themselves.
(iii) The PN referred the patient to the doctor on the same day, if the doctor was present that day.
(iv)The PN had a 'quick question' to ask the doctor, e.g. interpret a creatinine result or Xpert tuberculosis (TB) test.
(v) Phone calls or messages for advice from the doctor who usually works at that PHC clinic.
When using the data tool, the doctors also decided whether the booked referrals were appropriate or not. For example, a patient booked for review for a problem of hypertension, yet with a normal blood pressure and taking hydrochlorthiazide 12.5 mg daily and amlodipine 5 mg daily would not be considered an appropriate referral.
The data tool was pre-printed for each doctor and placed in a lever-arch file, with one copy of the data tool to be filled in after each consultation. Most of the data required could be ticked, and took <1 minute to complete. The data tool was pre-tested in the clinical situation, and modifications were then made. The data tool reflected the process of the consultation, including:
• demographic data (but omitting patient names or clinic record numbers)
• by what means the patient was referred to the PHC doctor
• the category of medical condition
• conclusion to the consultation: could the patient have been managed by a PN? Or was the patient's medical condition sufficiently complex so as to warrant management by a clinic doctor?
• qualitative information about the consultation, which could be written on the back of the data tool.
A group training session of how to fill in the data tool was conducted. Doctors were asked to use the data tool for 2 days, and these tools were checked to ensure correct understanding and practice. Then all the PHC doctors used the data tool for every patient for the month of February 2020, which was a normal working month, unaffected by holidays. Doctors were asked to review the accuracy of completion of their data tools at the end of their session. The primary researcher was available for advice by telephone, and drove to see doctors working at clinics so as to improve the quality of completion of the data tool. At the end of the month, all forms were collected at the district office. It had been intended that the team of researchers would gather together to review and analyse the data tools in a uniform manner. However, owing to COVID-19 and the lockdown, this was not possible. Instead, the primary researcher reviewed all the paper copies of the data tools. The data were captured from each doctor's lever-arch file into Excel (Microsoft, USA) by three researchers, and statistical analysis performed.
No clinical interventions were made in this descriptive research study.
Main outcome measures
Firstly, the most important measurement to prove with significance was that the patient's medical condition was sufficiently complex as to warrant management by the clinic doctor. This was to be compared with the number of doctor consultations that could have been managed by a PN. Secondly, we wanted to obtain a snapshot of the spectrum of medical work that the doctors were doing at the clinics.
Ethical considerations
This research was approved by the uMgungundlovu Health Ethics Review Board (UHERB) (ref. no. 004/2019). The ethical risks were minimal - no identifying details of the patients were collected.
Results
Description of population and sample
Thirty-five doctors participated in the research, working in 45 PHC clinics in uMgungundlovu District, which has a population of ~1.2 million people. Of these 35 doctors, 19 were part-time and 16 full-time. Twenty-six of the doctors were employed by NHI, of whom 7 also had private medical practices. The remaining 9 non-NHI doctors were employed directly by the KZN Department of Health. The PHC doctors worked a total of 925 hours per week in the PHC clinics in February 2020. This averaged 26 hours per week per doctor in the PHC clinics. The 35 doctors had a total of 228 years of experience of working in the PHC setting by 1 February 2020. The mean or average experience was 6.5 years per doctor; the median experience was 4.9 years and the range of experience was between 0 and 34 years. The doctors conducted a total of 7 424 consultations during February 2020. The total number of PHC consultations by PNs and doctors in February 2020 was 143 421. The results for the first objective are shown in Table 1.
Patient demographics
Female patients comprised 64% of the consultations, and male patients 36%.
In the <10-year-old age group, there were 64 infants aged <1 year, and 240 children between 1 year and their 10th birthday.
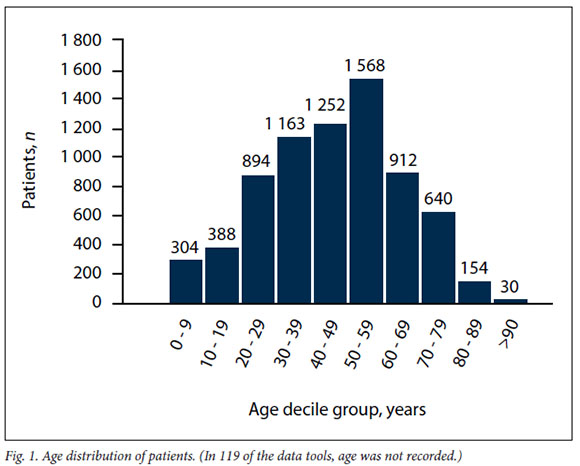
Of the doctor consultations, 4.1% were for children <10 years, and 9.3% were for children and youth <20 years (Fig. 1).
A breakdown of the ways in which the patients were booked for the doctor is shown in Table 2. Of the 7 424 doctor consultations, 3 618 (48.7%) were referred electively by the PN, while 1 341 (18.1%) were referred by the PN on the same day. Doctors considered 94% of the elective referrals and 87% of the same-day referralsto be appropriate, which was a significant difference by Pearson's χ2 test (p<0.0001). Doctors booked 2 185 patients for themselves to follow up.
The results for the second objective are shown in Table 3 - the spectrum of medical conditions that the doctors managed in the PHC clinics.
Further results on the conditions in Table 3 were as follows:
• Identified antenatal consultations: normal antenatal attendance 152; intrauterine growth restriction 22; previous caesarean section 52; hypertensive disorders of pregnancy 22; high HIV viral load 75.
• The most common problems in infants were, in order of frequency: dermatological problems, congenital problems, respiratory infections, neonatal jaundice and HIVrelated management issues.
• Patients with both hypertension and diabetes comprised 664 patients (8.9%).
• In patients with epilepsy, 83 women of child-bearing age (16 - 42 years) were taking valproic acid, which is not recommended.
• According to DHIS, a total of 140 patients were initiated on TB treatment in PHC clinics in February 2020 - doctors were involved in 43% of these initiations.
• Of the 169 TB review consultations, 57 were for disability grants (34%).
• There were 800 consultations for chronic medicine ordering: 418 patients were for Central Chronic Medicine Dispensing and Distribution (CCMDD). These medicines are available at a PHC clinic. A total of 382 patients were for repeat prescription cards - these medicines are not routinely available at PHC clinics, e.g. hydralazine.
Discussion
Principal findings
The first objective of the research was to determine whether a significant proportion of the patients whom the clinic doctors managed had sufficiently complex clinical problems that warranted being managed by a doctor. The doctors concluded that the vast majority of the consultations (93.6%) should indeed have been conducted by a doctor. Only 477 (6.4%) doctor consultations were thought to have been inappropriately referred to the doctor, and the patient should rather have been managed by the PN. Upon reviewing all the paper copies of the data tool, it was surprising that the figure of 477 patients for the PN was not even lower: several patients had problems that should probably have been managed by a doctor, such as chronic lower back pain and chronic skin rashes in children - both notoriously difficult conditions to manage successfully.
Bookings for the doctor: Patients booked electively by the PN for the doctor comprised almost half (48.7%) of the consults. The doctors assessed that 94% of these doctor bookings were appropriate, which reflects well on the judgement and experience of the PNs in the PHC clinics. Followup appointments by the doctor (29.4%) comprised a significant proportion of the patients who warranted being managed by a doctor. However, the doctor had already decided in the previous consultation that the patient needed to be followed up by a doctor rather than a PN. This high follow-up figure may be in keeping with the complexity ofthe patients consulted by doctors. Elective bookings by both PNs and doctors comprised 78.1% of the consultations. Patients referred by the clinic PN to the doctor on the same day (18%) are an important service, as otherwise many of these patients would have to be referred to the hospital. Doctors assessed that 86% of these patients were appropriately referred. The accuracy of the same-day referral by the PN was significantly different than for elective referrals, but the absolute magnitude was only 8%. Regardless of the difference, both were still good figures. It is very useful for PNs to have a doctor in the clinic of whom to ask a quick question. The number of quick-question consultations recorded was lower than expected (2.5%). This may be the result of the doctors not filling in the data tool for quick consultations. Doctors report that when consulting at a PHC clinic, the PNs ask them about five quick questions per working day about patient issues such as an X-ray or laboratory result. However, the PHC doctor needs to be approachable and knowledgeable for this to happen. Phone calls or phone messages comprised just a small number of the reasons for consultation (0.4%). This way of communicating should become more important. A part-time clinic doctor is not always on site, but knows the PNs and the clinical context.
Age distribution: Over 90% of doctor consultations were for adult patients from the age of 20 years. It is concerning that children and youth were not better represented in the patients seen by doctors. The most populous decile in age distribution was between 50 and 59 years.
The second objective of the research was to determine the spectrum of medical conditions that the doctors managed in the PHC clinics.
Emergencies: These constituted only 2.5% of doctor consultations, even though one of the important functions of a PHC doctor is to better manage emergency situations in the PHC clinic. Our perception that workload from emergencies was greater than the number measured could be due to the longer time that is spent with each emergency patient, such as for resuscitation or suturing.
Maternal and child health (MCH): This is perhaps the most important function of a PHC clinic. However, only 10.2% of doctor consultations were for antenatal women and children aged <10 years. The low rates of antenatal consultations could due be to three factors: the clinic midwives do not refer antenatal patients to the doctor; the doctors discourage referrals because they feel unsure of their knowledge of primary care obstetrics; and some NHI doctors reported that they had reservations about antenatal work due to lack of medicolegal indemnity. PHC clinic doctors in uMgungundlovu have for several years been requested to get more involved in MCH -e.g. every pregnant woman should be reviewed routinely at least once by a clinic doctor between 28 and 34 weeks' gestation. Several continuing professional development (CPD) sessions for doctors had been spent on antenatal care as well as ART in pregnancy.
The even lower rate of paediatric consults could be due to two factors: firstly, most of the PNs have been trained in IMCI, which covers primary care pediatric conditions, and so do not need to refer many children to the doctor. Secondly, all the PHC doctors have attended CPD sessions on basic IMCI, but not all have attended a full 10-day IMCI course, and may have felt unsure of their IMCI skills. IMCI training now forms part of a doctor's undergraduate pre-service training. Clinic doctors should be especially involved in ART care for children.
Non-communicable diseases (NCDs): It was expected that the majority of the doctor consultations would be for NCDs, and this proved to be correct, with 58.9% of consultations for NCDs. Epilepsy and mental health problems are both common conditions in uMgungundlovu District, and important for the doctor to be involved in and knowledgeable about. Data were collected on anti-epileptic drugs used for epilepsy - 83 women of childbearing age (set at 16 - 42 years) were found to be taking valproic acid. The PHC EML[9] now discourages the use of valproic acid for women of childbearing age because of potential teratogenicity. Renal and urological conditions were surprisingly common, especially chronic kidney disease. Thyroid conditions accounted for <1% of consultations, but are important for the PHC doctor to be involved in.
Communicable diseases: The need for good quality ART and TB management is an important reason for having a doctor working in a PHC clinic, and these conditions accounted for 23.5% of consultations. Interpreting laboratory results can be technical, and doctors need to be well acquainted with the latest TB and ART guidelines. ART initiation surprisingly accounted for only 1% of doctor consultations, and represents task-shifting of ART initiation from hospital to clinic doctor to PN. The nurse-initiated management of ART (NIMART)-trained PNs are becoming increasingly competent in ART management, and initiate the vast majority of patients onto ART. Same-day initiation of ART may be a factor in the low initiation rate by doctors: a patient may have been found to be HIV-positive and was started on ART on the same day, but the patient's management then became more complex a week later when the laboratory results show a low CD4, high serum creatinine or positive TB Xpert. ART first-line management accounted for 16.5% of consultations. Some of these patients were attending for another clinical problem, but the patient happened to be on first-line ART, and did not primarily have an ART management problem. ART second-line management accounted for 4.2% of consultations, and is an important field where a doctor should be involved.
Of the patients (n=60) initiated onto TB treatment, almost half (n=29) required an X-ray to make the diagnosis. In the district, a system has been set up whereby a patient can be referred for an X-ray at a hospital or CHC, and the patient brings back the radiograph to the clinic doctor for interpretation and treatment. Interpreting an X-ray for TB is beyond the scope of a PN. In February 2020, a total of 140 patients were initiated onto TB treatment in the PHC clinics, and doctors were involved in 43% of these TB initiations - this is an encouraging figure, but could be higher. The review of patients already on TB treatment accounted for 169 consultations. One-third of these consultations happened because the patient needed forms for a disability grant to be completed, which is not a medical reason for a doctor being involved in TB care.
Miscellaneous doctor consultations: The interpretation of laboratory results was a common reason (15.9%) for a patient being referred to a doctor. Interpreting laboratory results forms a large part of a doctor's undergraduate training, but less so for a PN. The teaching of laboratory result interpretation forms a more significant part of NIMART and postgraduate PHC nurse training. So it is very helpful having a doctor present in the PHC clinic to interpret laboratory results. The category of 'other medical conditions' accounted for a high proportion of consultations (24.0%) because it accounted for medical conditions not fitting into the predetermined categories of consultation in the data tool. 'Other medical and social conditions' could have ranged from cancer to ingrown toe nail.
Chronic medicine: A significant proportion of doctor consultations (10.8%) involved chronic medicine orders. A doctor working at a PHC clinic can optimise the management of chronic medicines in three areas. Firstly, doctors can initiate and continue medicines (e.g. lamotrigine) beyond the scope of the PN. Secondly, doctors can generate prescriptions for more complex patients onto CCMDD. The CCMDD system enables a stable patient to collect their medicines from outside the PHC clinic for 6 months, which is a safer practice in times of COVID-19. Only a doctor can prescribe schedule 5 medicines (e.g. risperidone or tramadol) onto CCMDD. Thirdly in KZN, repeat prescription cards (colloquially called 'pink cards') are used to continue to order medicines that were initiated at a hospital or specialist level, but are not on code for a PHC clinic: e.g. hydralazine as a fourth medicine for hypertension, or brimonidine for glaucoma. Only a doctor can prescribe the repeat prescription card, thus enabling a patient to conveniently collect their essential medicines at local level.
A doctor at a PHC clinic should do minor surgical procedures such as suturing lacerations, doing skin biopsies and taking blood where venous access is difficult. The research showed that a small but significant number of consultations (n=268) were for these reasons.
Referrals: Referrals by the doctor occurred in a significant proportion of the consultations (10%), and a third were of an urgent nature. Most referrals were to the referral hospital. However, some referrals were to other health professionals within the clinic, such as an outreach physiotherapist. The high referral rate of 10% appears to be a contradiction in terms, because a doctor is supposed to be working at a clinic in order to reduce the number of referrals to hospital. However in reality, the PNs refer a lot of the patients to the clinic doctor, who should have better skills in organising patients with medical conditions for management - either at the clinic or at the hospital. In fact, this shows a good system at work. In February 2020, the PHC clinics conducted a grand total of 143 421 consultations, with doctors referring 742 patients, which is only 0.5% of the total patients consulted. Inevitably, some patients will have medical conditions requiring referral to hospital. Of course, PNs do themselves refer patients directly to hospital if there is no doctor present that day, or the reason is clear, e.g. a red IMCI classification.
Administrative work: This is part of any doctor's working day, and comprised 17.4% of consultations, including J88 forms, unemployment insurance forms, etc. However, completion of various disability grant applications comprised 88% of the administrative consultations and 15.2% of total consultations. This proportion is significant, but in keeping with the district recommendation that a PHC doctor should consult no more than five patients for disability grants in an 8-hour working day (15% - 20% of consultations). Filling in disability grant forms is a necessary function in our health and social setting, and is an opportunity to review the health of the patient. A total of 128 (11%) of the disability grant consultations were for grant-in-aid (GIA). The GIA used to be awarded only for patients with severe disabilities such as paraplegia or severe stroke.[13] However, it now appears to be awarded for anyone >70 years of age, irrespective of health status.
In summary, PHC doctors have particular clinical skills to address more complex conditions and scenarios in primary care. Some examples of these complexities are greater ability to: diagnose patients with undifferentiated clinical problems; manage patients with more complex clinical problems; manage patients with a number of comorbidities; interpret X-rays and laboratory results onsite; perform more difficult clinical procedures onsite; and prescribe higher levels of medication at PHC clinic level.
Strengths and weaknesses of the study
A strength of the study was that all 7 424 doctor consultations for a whole month were recorded and analysed, not just a sample. This provided a good snapshot of the spectrum of work being done by PHC doctors in the district. A potential weakness may have been using PHC doctors themselves for completion of the data tools. However, it is good for doctors to be able to reflect upon their own clinical practice.
Contribution to the body of knowledge and strengths and weaknesses in relation to other studies: This study quantified the benefit of a doctor working in a PHC clinic.
The meaning of the study to clinicians and policy makers: This research showed that a doctor is an essential, 'must-have' role player in the PHC clinic. Managers, planners and funders should consider formalising the role into permanent funded medical posts for PHC clinics, for the benefit of the patients.
Unanswered questions and recommendations for future research: More study could be done on: referrals from PHC to hospital; models of how best to place and fund doctors in PHC clinics; and clinical competencies required for a doctor to work in a PHC clinic.
Conclusion
This research showed that at a PHC clinic, the more complex patient consultations did indeed require the skills and knowledge of a medical doctor managing these patients. These data support the benefit of a doctor working at every PHC clinic: The doctor is a 'must-have' member of the PHC clinic team, offering a regular, reliable and predictable medical service.
Declaration. None.
Acknowledgements. The authors thank uMgungungdlovu Health District and the KZN Department of Health for their support of the research. Thanks also to the dedicated PHC doctors for participating in the research.
Author contributions. TPK: primary researcher, author, study design, cleaning and review of data tools, capture of data onto Excel, initial data analysis, manuscript finalisation. PGTC: detailed statistical analysis and interpretation. HLH and AR: capture of data onto Excel. NGM: assistance with study design, pre-testing and review of manuscript.
Funding. None.
Conflicts of interest. None.
References
1. South African Government News Agency. Ten districts announced for NHI pilot. SANews, 22 March 2012. https://www.sanews.gov.za/south-africa/10-districts-announced-nhi-pilot (accessed 27 May 2022). [ Links ]
2. KwaZulu-Natal Department of Health. KZN Budget Policy Statement 2022/23 by Simelane N Hon. MEC for Health, 10 May 2022. [ Links ]
3. Marcus T, Hugo J. Community orientated primary care: Where there is a doctor. In: Mash B, ed. Handbook of Family Medicine. 4th ed. Cape Town: Oxford University Press, 2017:334-359. [ Links ]
4. Nkosi PH, Horwood CM, Vermaak K, Cosser C. The role of doctors in provision of support for primary healthcare clinics in KwaZulu-Natal, South Africa. S Afr Fam Pract 2009;51(5):408-412. https://doi.org/10.1080/20786204.2009.10873893 [ Links ]
5. Gaede B. Revisiting the doctor's role at the primary healthcare clinic. S Afr Fam Pract 2020;62(1):a5242. https://doi.org/10.4102/safp.v62i1.5242 [ Links ]
6. Mash R, Ogunbanjo G, Naidoo SS, Hellenberg D. The contribution of family physicians to district health services: A national position paper for South Africa. S Afr Fam Pract 2015;57(3):54-61. http://hdl.handle.net/10019.1/99785 (accessed 5 January 2022). [ Links ]
7. Pillay S, Lutge E, Aldous C. The burden of diabetes in KZNs public sector: A 5-year perspective. S Afr Med J 2016;106(4):384-388. https://doi.org/10.7196%2FSAMJ.2016.v106i4.9920 [ Links ]
8. Couper I, Malete N, Tumbo J, Hugo J. The role of the visiting doctor in primary care clinics. S Afr Fam Pract 2003;45(6):11-16. [ Links ]
9. National Department of Health, South Africa. Standard Treatment Guidelines and Essential Medicine List for South Africa: Primary Health Care Level. Pretoria: NDoH, 2018. http://www.health.gov.za/edp.php (accessed 20 September 2020). [ Links ]
10. Tumbo J, Hugo J, Couper I. The involvement of private general practitioners in visiting primary health care clinics. S Afr Fam Pract 2006;48(7):16-16d. https://doi.org/10.1080/20786204.2006.10873420 [ Links ]
11. Department of Health, KwaZulu-Natal. KZN Department of Health Item Catalogue for Provincial Pharmaceutical Supply Depot. KZN DoH, 2022. [ Links ]
12. National Department of Health, South Africa. Adult primary care: Symptom-based integrated approach to the adult in primary care. Pretoria: NDoH, 2019/2020. https://www.knowledgehub.org.za/system/files/elibdownloads/2020-08/APC%202019-20%20eBook.pdf (accessed 27 May 2022). [ Links ]
13. South African Social Security Agency. You and your grants 2020/21. https://www.sassa.gov.za/publications/Documents/You%20and%20Your%20Grants%202020%20-%20English.pdf (accessed 27 May 2022). [ Links ]
 Correspondence:
Correspondence:
T P Kerry
tkerry@futurenet.co.za
Accepted 8 August 2022














