Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.1 Pretoria Jan. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i1.16746
IN PRACTICE
ISSUES IN MEDICINE
Practising in a post-truth world: Pandemic ethics can inform patient autonomy and clinical communication
L BranniganI; H R EtheredgeII, III; C LundgrenIV, V; J FabianVI, VII
IFCP (SA), Cert Critical Care (SA); Wits Donald Gordon Medical Centre and School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMSc Med (Bioethics and Health Law), PhD; Wits Donald Gordon Medical Centre and School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMSc Med (Bioethics and Health Law), PhD; Department of Internal Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVPhD, MMed (Health Law and Bioethics); Wits Donald Gordon Medical Centre and School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VPhD, MMed (Health Law and Bioethics); Steve Biko Centre for Bioethics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIFCP (SA), PhD ; Wits Donald Gordon Medical Centre and School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIIFCP (SA), PhD ; Department of Internal Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
The COVID-19 pandemic posed an unprecedented challenge to modern bioethical frameworks in the clinical setting. Now, as the pandemic stabilises and we learn to 'live with COVID', the medical community has a duty to evaluate its response to the challenge, and reassess our ethical reasoning, considering how we practise in the future. This article considers a number of clinical and bioethical challenges encountered by the author team and colleagues during the most severe waves of the pandemic. We argue that the changed clinical context may require reframing our ethical thought in such a manner as to adequately accommodate all parties in the clinical interaction. We argue that clinicians have become relatively disempowered by the 'infodemic', and do not necessarily have adequate skills or training to assess the scientific literature being published at an unprecedented rate. Conversely, we acknowledge that patients and families are more empowered by the infodemic, and bring this empowerment to bear on the clinical consultation. Sometimes these interactions can be unpleasant and threatening, and involve inviting clinicians to practise against best evidence or even illegally. Generally, these requests are framed within 'patient autonomy' (which some patients or families perceive to be unlimited), and several factors may prevent clinicians from adequately navigating these requests. In this article, we conclude that embracing a framework of shared decision-making (SDM), which openly acknowledges clinical expertise and in which patient and family autonomy is carefully balanced against other bioethics principles, could serve us well going forward. One such principle is the recognition of clinician expertise as holding weight in the clinical encounter, when framed in terms of non-maleficence and beneficence. Such a framework incorporates much of our learning and experience from advising and treating patients during the pandemic.
An elderly man with COVID-19 pneumonia, from a geriatric frail-care facility, is admitted for supplemental oxygen. His family are extremely anxious, as they have not been allowed to visit him and are having difficulty accessing the attending clinician. The attending clinician has been on call for 36 hours with very few staff, as colleagues have either contracted COVID-19 or are isolating after being exposed. When the clinician calls, a family member mentions that they spoke to a nurse about their father's treatment and would like to know why he is not receiving ivermectin. They saw Facebook posts saying that it works, adding that their general practitioner was able to source ivermectin from a veterinary supplier. The clinician explains that until there is better evidence to support its use, hospital policy is to not use ivermectin. The family are displeased, to put it mildly.
This case highlights a common experience in clinical practice during COVID-19, where the tensions highlighted, although not necessarily new, are accentuated by the pandemic to an unprecedented extent. As the pandemic begins to ease, allowing some reflection, we propose that lessons learned can improve post-pandemic clinical practice. COVID-19 has changed the way in which patients, families and staff in the healthcare sector interact with each other, and it has demanded that we redefine what 'autonomy' means for everyone involved in the healthcare process. It has also challenged the neutrality of regulators and lawmakers as self-determining institutions, as evidenced by the case of the South African Health Products Regulatory Authority (SAHPRA) registering ivermectin in the wake of extensive public pressure.
This article considers the intersection of emerging ethical challenges facing clinicians in South Africa (SA), and is based on our experience of managing COVID-19 patients at the coalface.
We have termed the first ethical issue 'clinical evidence assessment', and it involves a clinician's ability to critically evaluate an ever-expanding corpus of knowledge and to ensure that evidence-based science informs their clinical practice. Clinicians need to contextualise the abundance of published information available to their patients, who, given access to this information, are more likely to challenge how their condition is managed. This needs to be done in a way that advances the autonomy of patients through presenting all available alternatives. However, this is a mammoth task, given wide non-consensus regarding these alternatives among stakeholders. Although accentuated in the COVID-19 pandemic, where the science evolved quickly and best practice was a 'moving target', the challenge remains post pandemic, albeit that there is now more time to develop consensus documents and treatment guidelines.
The second ethical issue involves navigating a tangible realisation of patient autonomy within an emerging conviction among patients and their families that autonomy should be unlimited. We have termed this issue 'information and empowerment'.
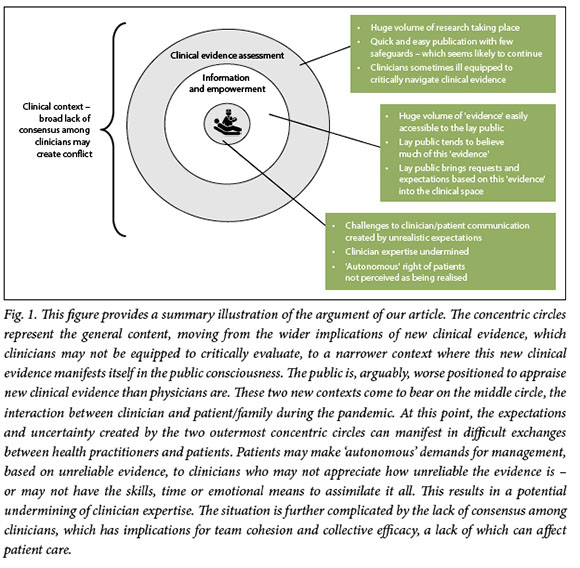
We argue that these ethical issues, combined, create a multi-layered clinical context where each level has implications for the interaction at the centre of healthcare: that between clinical team and patient. It is through this interaction that the ethical principle of patient autonomy is realised, or otherwise. We propose that a strongly entrenched framework of shared decision-making (SDM) may foster a more productive environment for clinical encounters.
Discussion
Our proposed framework accounts for the emerging ethical and legal uncertainties of the pandemic and lays a foundation for realistic discussions about patient management in a post-pandemic world. Our argument is summarised in Fig. 1.
Clinical evidence assessment
Our familiar principles of ethical practice continue to evolve. Generally, formulations of autonomy, beneficence, non-maleficence and justice anchor ethical reasoning in clinical settings, with a peppering of care ethics and utilitarianism. However, this contemporary ethical guidance did not anticipate the huge challenges a pandemic would bring, and an ethical vacuum has emerged. Simultaneously, the 'ripping up' of our trusty pre-pandemic rulebook has opened the door to widespread improvisation and experimentation, which does not fit neatly into our ethics frameworks, and new mechanisms to understand ethical dilemmas are required. Most countries - including SA -are currently authoring ethical guidelines for pandemic research, presupposing a lack of such guidance to begin with, and acknowledging that pandemics may occur more frequently in the future.
Improvisation and experimentation is not problematic in and of itself, as innovation is key to overcoming a novel virus.[1] However, a combination of the unprecedented volume of so-called research with the ability to publish content with relative ease, poses some challenges. Academic medical journals and the lay press have been inundated with COVID-19-related articles addressing treatment options, vaccination and public perceptions. Often, these articles purport to have sound research methodology and scientific rigour.[2] Platforms like medRxIV have stolen the limelight, publishing research studies that have not been peer reviewed - and the legitimacy of which in contributing to the scientific evidence base is questionable. However, the benefit of such a platform over traditional academic publishing processes is the speed with which information can be made public, as the peer review process often takes several weeks (or months), resulting in delayed publication.[3] Although such platforms host a disclaimer that articles have not been peer reviewed and therefore should not be used to guide clinical practice and should be reported in the news media with caution, it appears that they are used for both these things.
At present, clinicians must navigate the huge body of published research, and decide what is relevant. This presupposes that clinicians are well positioned to evaluate scientific articles. However, critical appraisal of medical literature is a difficult area that requires much training and practice. It is often presumed in clinicians as a fait accompli having been to medical school. While it is true that medical students in SA are required to undertake a research project as part of their undergraduate studies, and a research component is built into the MMed degree required as part of specialist training and qualifications in SA, this does not equate to a deep understanding of the generation and interpretation of empirical evidence.
Further complicating clinical appraisal of research is a perception that high-quality medical evidence is not essential to regulatory decision-making, undermining the imperative of a strong evidence base in clinical practice. Patient-generated movements, sometimes supported by clinicians, have gained much momentum during the pandemic and are partially responsible for creating this situation. For instance, these groups have applied substantial pressure on regulatory authorities to make medications supposedly associated with better COVID-19 outcomes available for prescription to humans, with limited evidence. In SA, the most notable example of this is SAHPRA's registration of the anthelmintic drug ivermectin for COVID-19 treatment and prophylaxis. In cases like these, the actions of civil society and patient advocacy movements have arguably undermined the regulator.[4] It goes without saying that if the regulator is pressured by patients, we can empathise with how clinicians at the coalface may be feeling.
Information and empowerment
The plethora of often unvalidated information discussed in the previous section, now known as the infodemic, is muddying the waters not only of public perception, but also of patient care. The infodemic has made it more difficult to meet the needs of patients and healthcare systems. It has 'empowered' people with information that may not be reliable. In our anecdotal experience, patients may try to utilise questionable publications with unreliable results as leverage to request or demand (or refuse) certain treatment modalities, preventive strategies or vaccination.[3,5] The lack of direction and consensus consequent to the infodemic has given a platform to 'magic bullet' therapies and treatments, which have captured the public imagination. Ironically, these platforms have also fuelled vaccine hesitancy and provided a conduit for vaccine-related myths to circulate.
Clinicians are expected to navigate these complexities through communication. There is an obligation to communicate relevant information, treatment plans, team decisions and prognostic factors to patients and their families. These groups are not only empowered with information but also in a state of panic given the high stakes associated with COVID-19 hospitalisation. Clinicians, for reasons to be discussed, are disempowered.
Clinical communication
Academic enquiry in the field of health communication is well established, and in pre-pandemic times, numerous barriers to communication between clinicians and patients/families had been identified. Regardless of specialty or treatment modality, common barriers to clinician-patient communication are:
• Lack of time on the part of clinicians to communicate with patients/families. Sometimes this is linked to an absence of highlevel hospital policies endorsing clinical communication or setting a minimum standard for it.
• Discomfort with communicating bad news/prognoses - and an accompanying feeling of failure on the clinician's part.
• The complexity of translating medical concepts into lay language that can easily be understood by patients/families.
• In countries like SA, language mismatches, where the clinician is unable to speak the first language of the patient/family and interpreters may not be available.
This is not an exhaustive list. And COVID-19 has rendered these barriers to communication more acute because it brings substantial uncertainties and a corresponding sense of panic. Further barriers to communication have emerged thanks to COVID. These are mainly physical, such as conversing with the families of inpatients over the phone or a video call, as well as the barriers presented by personal protective equipment, where patients may be unable to pick out any distinguishing features of the individual treating them. The patient burden for many clinicians has increased with rotation of fewer staff through wards. The time pressures that often limit clinical communication are therefore also more acute during the pandemic. If the state of inpatient communication was wanting in pre-pandemic times, the pandemic has arguably made it more so. Interestingly, as many now work remotely, so too has much clinical practice remained remote and distanced in the specialties where physical interaction with patients is not required to provide care.
Clinical practice
It is probably unsurprising that clinicians find themselves inundated with demands from patients and their families to provide unregistered or unproven treatments.[6] Sometimes these demands are accompanied by thinly veiled threats if said treatment or procedure is not provided, especially the threat of legal action. These occur within a policy vacuum, similar to the ethical vacuum discussed previously, where our guiding frameworks have not been designed to respond to the challenges posed by COVID-19. The policy vacuum is characterised by:
• Substantial confusion created by varying levels of medical evidence, and their clinical interpretation or implications.
• Absence of robust communication and decision-making frameworks in many hospitals.
Within this vacuum, a seemingly accepted belief that patient autonomy should supersede all else has become evident, with patients and families repeatedly stating that it is their 'autonomous right' to access this or that treatment.[7,8] Clinicians are more or less disabled in the interaction, and fear legal or reputational repercussions. It is notable, however, that while patients and families may be more rights-aware than ever before, clinicians are not necessarily obliged to provide treatment unless the situation is an emergency.[9] The South African Medical Association stipulates that clinicians have the right to choose their patients, especially in a context where a patient or family's behaviour starts to infringe on the constitutional rights of the clinician, such as the right to bodily and psychological integrity.[9] This right must be balanced against the duty of care clinicians owe their patients, and as such it is a complex legal area that has not been empirically tested in a court. Consequently, clinician autonomy also has an important role to play, and it may often be overlooked.
Clinical interactions, patient autonomy and post-pandemic practice
Over the past half-century, the patient-centred care movement has gained significant traction worldwide. Patient-centred care is rooted in the bioethical principle of autonomy and involves placing the patient in a position such that they can adequately articulate their autonomous preference for healthcare, provided they are given correct information.[10] This is realised through extensive communication between patient and members of the healthcare team, and relies heavily on co-ordination and agreement among the healthcare team. Options are presented to the patient with their attendant risks, benefits and consequences, and the patient chooses which would be preferable.
Patient-centred care places a significant emphasis on the knowledge and lived experience of the patient. The latter is always subjective, and should never be overlooked. The former proves more elusive, especially in an environment where the volume of information available to a patient is unsurpassed, as discussed in the 'Information and empowerment' section of this article. Patient-centred care models do not appear to be adequate facilitators of communication in the setting of a pandemic.[11,12] If clinicians struggle to appraise huge volumes of published information and make treatment decisions on its basis, as discussed in the 'Clinical evidence assessment' section, it is reasonable to conclude that patients must be feeling even more overwhelmed by information overload.
Simultaneously, the empowered patient population today is aware of their rights, will evoke the notion of autonomy and will express their expectation of such. They may threaten medical staff with legal action even in cases where their autonomous preferences cannot be fulfilled - for instance, in asking doctors to prescribe a treatment that is not registered, perform a procedure based on limited scientific evidence, or bend the rules put in place to protect the hospital workforce.[13] These situations are occurring in a world where medical literacy remains poor.
Two major issues need to be addressed to facilitate good medical practice as we begin to comprehend a post-pandemic world. Firstly, we need to consider whether SA clinicians are adequately empowered in synthesising medical evidence, and in the event of a lack of robust evidence, clinicians need a forum where they can discuss tricky treatment propositions with their peers, possibly in a mediated manner. Secondly, a system supporting clinician expertise and bringing this to bear more forcefully in the doctor-patient interaction is important, especially when patients have limited or incorrect information. Clinicians also need to be assured of the protection of their hospital or institution, a particularly complex issue in the private sector, where the contractual nature of the relationship between clinicians and institution varies. All the while, these recommendations need to be tempered by a recognition that clinical practice is still about people, who have certain preferences, and that these need to be given equal attention.
Shared decision-making with imperfect information
Through fostering a system of SDM, it may be possible to realign clinician expertise and patient expectations in SA.[14] Although the SDM framework has been around for some decades, its uptake has been relatively poor.[15]
SDM requires a conversation, in which best-available evidence and patient preferences are incorporated and a two-way flow of information gives rise to the realisation of patient autonomy, while also presenting a reasonable framework for patient expectations of treatments that they feel would be preferable.[15] One of the main advantages of SDM is that it allows for the intersection of the clinician's experience and training as a locus of authority, with the expertise of the patient as a locus of experience.[16] This presupposition that both parties have a pivotal role in decision-making helps to promote an environment in which a clinician could be better empowered to turn down unreasonable requests in the knowledge that this is supported at an institutional level. One of the lessons we have learned from COVID-19 is that where there is a collective will and commitment towards implementing certain hospital policies, it is possible to put these in place and gain the buy-in of the majority of the hospital workforce. Moreover, it is vitally important that a culture of SDM is communicated to patients and their families as something that the hospital actively encourages.
Declaration. None.
Acknowledgements. None.
Author contributions. LB and CL: conceptualised the study, reviewed and edited the manuscript; HRE: contributed the bioethics framework and wrote the first draft of the manuscript; JF: reviewed and edited the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Troya J, Seijo LM, Pérez M, Sentchordi-Montane L, Martínez-Alcalá Á. Improvisation in times of pandemic, a reason for reflection. Int J Infect Dis 2020;96:361-362. https://doi.org/10.1016/j.ijid.2020.05.038 [ Links ]
2. Palayew A, Norgaard O, Safreed-Harmon K, Andersen TH, Rasmussen LN, Lazarus JV. Pandemic publishing poses a new COVID-19 challenge. Nature Hum Behav 2020;4(7):666-669. https://doi.org/10.1038/s41562-020-0911-0 [ Links ]
3. Oermann MH, Nicoll LH. A primer on preprints. Nurse Author Editor 2020;30(2):1-10. https://doi.org/10.1111/j.1750-4910.2020.tb00564.x [ Links ]
4. Goodman JL, Borio L. Finding effective treatments for COVID-19: Scientific integrity and public confidence in a time of crisis. JAMA 2020;323(19):1899-1900. https://doi.org/10.1001/jama.2020.6434 [ Links ]
5. Uscinski JE, Enders AM, Klofstad C, et al. Why do people believe COVID-19 conspiracy theories; Harvard Kennedy School Misinformation Rev 2020;1(3). https://doi.org/10.37016/mr-2020-015 [ Links ]
6. Wadvalla B-A. COVID-19: Ivermectin's politicisation is a warning sign for doctors turning to orphan treatments. BMJ 2021;373:n747. https://doi.org/10.1136/bmj.n747 [ Links ]
7. Parmet WE, Paul J. COVID-19: The first posttruth pandemic. Am J Public Health 2020;110(7):945-946. https://doi.org/10.2105/ajph.2020.305721 [ Links ]
8. Stock PG, Wall A, Gardner J, et al. Ethical issues in the COVID-19 era: Doing the right thing depends on location, resources, and disease burden. Transplantation 2020;104(7):1316-1320. https://doi.org/10.1097/tp.0000000000003291 [ Links ]
9. South African Medical Association. Rights and responsbilities of doctors and patients. 2012. https://www.samedical.org/images/attachments/rights-and-responsibilities-of-doctors-and-patients-jul012.pdf (accessed 16 May 2021). [ Links ]
10. Reynolds A. Patient-centered care. Radiol Technol 2009;81(2):133-147. [ Links ]
11. Hamza M, Khan H, Sattar Z, Hanif M. Doctor-patient communication in surgical practice during the coronavirus (COVID-19) pandemic. Br J Surg 2020;107(7):e193. https://doi.org/10.1002/bjs.11661 [ Links ]
12. Wittenberg E, Goldsmith JV, Chen C, Prince-Paul M, Johnson RR. Opportunities to improve COVID-19 provider communication resources: A systematic review. Patient Educ Couns 2021;104(3):438-451. https://doi.org/10.1016/j.pec.2020.12.031 [ Links ]
13. Menon V, Padhy SK, Pattnaik JI. Stigma and aggression against health care workers in India amidst COVID-19 times: Possible drivers and mitigation strategies. Indian J Psychol Med 2020;42(4):400-401. https://doi.org/10.1177/0253717620929241 [ Links ]
14. Abrams EM, Shaker M, Oppenheimer J, Davis RS, Bukstein DA, Greenhawt M. The challenges and opportunities for shared decision making highlighted by COVID-19. J Allergy Clin Immunol Pract 2020;8(8):2474-2480.e1. https://doi.org/10.1016/j.jaip.2020.07.003 [ Links ]
15. Légaré F, Adekpedjou R, Stacey D, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2018;7(7):CD006732. https://doi.org/10.1002/14651858.cd006732.pub4 [ Links ]
16. Barnoy S, Ofra L, Bar-Tal Y. What makes patients perceive their health care worker as an epistemic authority? Nurs Inquiry 2012;19(2):128-133. https://doi.org/10.1111/j.1440-1800.2011.00562.x [ Links ]
 Correspondence:
Correspondence:
J Fabian
june.fabian@wits.ac.za
Accepted 29 August 2022














