Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.12 Pretoria Dez. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i12.16685
IN PRACTICE
HEALTHCARE DELIVERY
Successful multi-organ donation from a district-level hospital without an intensive care unit - a case series of referrals over an 18-month period
D ThomsonI, II; T du ToitI, II; F McCurdieIII; M ReynekeIV; E MullerV, VI; A BrinkVII; E du PlooyVIII, IX
IMMed (Surg), FCS (SA); Transplant Unit, Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
IIMMed (Surg), FCS (SA); Groote Schuur Hospital, Cape Town, South Africa
IIIBSc (Nursing), RN; Groote Schuur Hospital, Cape Town, South Africa
IVBCur, MCur; Groote Schuur Hospital, Cape Town, South Africa
IXMB ChB, MBA; Department of Economics and Management, Faculty of Economics and Law, University of Verona, Italy
VFCS (SA), MBA; Transplant Unit, Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
VIFCS (SA), MBA; Groote Schuur Hospital, Cape Town, South Africa
VIIMB ChB; Knysna Provincial District Hospital, Eden District, Western Cape, South Africa
VIIIMB ChB, MBA; Knysna Provincial District Hospital, Eden District, Western Cape, South Africa
ABSTRACT
Organ and tissue donation depends on non-transplant clinicians to identify and timeously refer potential donors and to counsel families compassionately about the prognosis at end of life. Organ donation referral is often felt to be beyond the capacity of district-level hospital services. In this case series, we report on four referrals from a geographically remote, public sector district-level hospital, and review the identification, referral and consent process of potential donors after brain death, and also donors after circulatory death. For the one successfully consented donor we report on the donor work-up and management, and the outcome of the organ recovery and organ allocation process.
Organ donation is typically felt to be beyond the remit of services offered outside of hospitals in major metropolitan areas. District-level hospitals have no intensive care units, and may not have blood gas machines or capacity and expertise to identify, refer and manage potential donors.[1] In addition, they may lack the ability to accurately diagnose the cause of death in complicated cases.[2]
South Africa (SA) has very low numbers of deceased organ donors.[3]
This is due to multiple factors; however, a combination of low referral rates of potential donors to the transplant teams and low consent rates is felt to be key.[4] These factors are majorly impacted by a lack of awareness of who can be a donor, and unfamiliarity with best practice related to the timing of referral and technique of obtaining consent by treating clinicians. Efforts are needed to expand the number of donors in SA by ensuring that all patients are adequately assessed for organ donation potential at the end of life. Spain has shown that while the spectrum of pathology alters the deceased donor potential of a hospital (e.g. based on the presence of a neurosurgery or stroke unit), up to 26% of donors can come from smaller hospitals.[5]
Methods
We report on a case series of donor referrals from a remote provincial district-level hospital in SA over an 18-month period following an educational outreach project. All organ donor referrals from the hospital were recorded by the transplant co-ordinator on call for the referral centre, and recorded as per standard practice. The clinical circumstances, timing of the referral, advice given on the potential for donation and outcome were critically reviewed. Ethics approval was given by the University of Cape Town, Human Research Ethics Committee (ref. no. HREC REF:185/2019)
Case 1
A 42-year-old hypertensive patient on treatment collapsed. The patient was transferred to George Provincial Hospital, where a computed tomography (CT) scan showed a massive spontaneous intracranial haemorrhage. The Glasgow Coma Score (GCS) remained at 2T on no sedation, and he was transferred ventilated back to Knysna for end-of-life care. A previous episode of pyelonephritis in 2011 showed normal renal function. Consent was granted for organ donation and the transplant centre contacted, but consent was subsequently withdrawn while the brain death testing was being performed.
Case 2
A 30-year-old morbidly obese person collapsed at home. The patient was transferred to George Provincial Hospital for a CT scan, which showed intracerebral haemorrhage with severe brain swelling. The patient's blood pressure was labile with a creatinine of 120 µmol/L. Urine dipstick showed 2+ protein. Organ donation was mentioned to that family at George Provincial Hospital prior to transfer back to Knysna for end-of-life care. The patient demonstrated persistence of some brain stem reflexes in the form of intermittent respiratory effort and a cough reflex. The patient was referred to the transplant team for potential donation after circulatory death. The transplant team assessed the patient as unsuitable for organ donation based on a combination of factors: that it would be a donor after circulatory death, that there was evidence of some renal impairment and that it would be a long-distance retrieval.
Case 3
A 47-year-old with an isolated stab to the head was admitted at 23h30 with a GCS of 13/15, but deteriorated rapidly during the night to a GCS of 2T requiring intubation, and became haemodynamically unstable, requiring initiation of an adrenaline infusion. A persistently high urine output of >500 mL/hr developed, and a clinical diagnosis of diabetes insipidus was made. The GCS remained 2T despite no sedation being given. The patient was assessed as a potential donor, with advice given to perform brain death testing 12 hours after the intubation dose of midazolam. The patient suffered a cardiac arrest during the cold caloric testing of the brain death test.
Case 4
A 19-year-old presented with an isolated transhemispheric gunshot wound to the head. The patient was intubated on scene without sedation and certified brain dead shortly after arrival in hospital. History revealed methamphetamine (tik) use for 3 years. The patient's height was 1.8 m and weight 70 kg. A consent approach was made by the treating clinician to the mother, with the transplant co-ordinator answering questions from the mother over the phone. Consent was obtained from the forensic pathologist and medical manager of Knysna Hospital. The donor was managed in the casualty unit on an Oxylog emergency/transport ventilator overnight, and was stable without requiring inotropes, but developed evidence of disseminated intravascular coagulation. An echocardiogram was requested by the cardiac transplant team. The Knysna team arranged for the private sector to perform this test, which showed a good-quality heart. An organ recovery operation was scheduled for 09h00 the following morning, with thoracic and abdominal retrieval teams coming from Cape Town. The creatinine deteriorated overnight from 76 to 176 µmol/L, and the liver function tests deteriorated slightly overnight, but the international normalised ratio improved from 2.6 to 1.3. The heart was allocated to a private sector recipient in Cape Town, as the blood group-suitable state recipient had a positive crossmatch. The liver was allocated to a recipient on the Johannesburg waiting list, as the Red Cross Children's Hospital recipient based in Eastern Cape Province was uncontactable. The kidneys were allocated to a George provincial recipient (the donor centre kidney) and Cape Town private sector recipient (the provincial 'pool' kidney).
Discussion
Organ donation is possible from small hospitals with limited resources and geographically remote from transplant centres. In this series, the single successful donor resulted in potentially >50 life years being gained by the recipients of the heart, liver and kidneys.[6] Additionally, a dialysis place was opened up in the state sector, where stringent dialysis rationing takes place, and a new patient was accomodated as a result of a state patient being transplanted.[7]
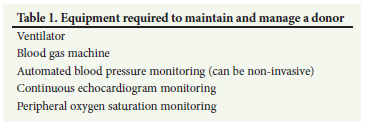
Knysna Provincial Hospital is a 90-bed district-level hospital situated 62 km from its regional hospital, George Hospital, and 650 km from the tertiary academic centre Groote Schuur Hospital. It serves a population of 120 000 people, with 17 doctors (7 of whom are community service doctors) covering primary healthcare, medical, surgical, maternity, paediatric and mental health services. Since 2011, the Eden district has been a National Health Insurance pilot site, with projects developed and relationships with the private sector explored. The hospital has 2 Oxylog ventilators in the emergency unit, a blood gas machine and laboratory services off-site. This level of resources was able to maintain and manage potential donors (Table 1) and to assess the donor organ suitability for transplantation. In one case, the local private sector was used to perform the echocardiogram to assess heart suitability (Table 2). Additional virological testing and the tissue-typing bloods necessary for allocation are sent through to specialised laboratories.
A series of academic outreach projects increased awareness around organ and tissue donation in the medical community in Knysna. These were a lecture on 'Organ donation in South Africa' from a surgical outreach team, free access to an online course 'Organ Donation: From Death to Life'[8] (Fig. 1; https://www.coursera.org/learn/organ-donation) and a local community pro-con debate on whether death determination is primarily a medical or a cultural determination.
These were followed by the series of referrals that we have presented here. There had never been any referrals from this hospital prior to the academic outreach projects. In our series, all referrals were appropriate. It is recognised that not all referrals will result in organ donation taking place, for varied reasons. Guidelines advise that good end-of-life care should as a standard of care explore the patient's wishes towards donation.[2]
In the first case, donation did not take place because of withdrawal of consent. Unfortunately, in this case the donation discussion had taken place prior to formal brain death certification being completed. The request for consent is best done as a planned approach once the prognosis has been communicated with the family. Ideally, a trained requestor should make the request, but where this is not possible it is important to have had a discussion with a specialist transplant co-ordinator to clarify the potential donation options and individualise the consent request.
In the second case, donation did not take place because the donor was assessed as an unsuitable candidate. The referral was appropriate as although certain factors, such as the morbid obesity in this case, may impact on the suitability of organs, it is important that decisions on suitability of a donor (when accepted referral triggers are met) are made by transplant teams who are aware of current urgent listings who may accept marginal donor organs, and are able to advise on the latest advances and capabilities related to organ retrieval.
In this case it was not one single factor that precluded organ donation, but rather a combination of factors. The referral timing was appropriate, as the clinical decision to withdraw mechanical ventilation had been made independent of the transplant team. The patient was expected to proceed to circulatory arrest upon withdrawal of non-beneficial life-sustaining treatment. Groote Schuur Hospital, which Knysna Provincial Hospital refers to, has a protocol in place to support donation after circulatory death, with good results published.[9]
In the third case, the potential donor was unable to be maintained during the brain death testing. In the UK, a potential donor audit in 2011/2012 showed that 8% of donors did not proceed to donation owing to inability to maintain the donor.[10] This is why donors are typically not transported from the referral hospital, with transplant teams being mobilised to perform the organ recovery, which is typically done close to the family of the deceased and within the jurisdiction of the local forensic pathologist. Active donor management is essential in ensuring that potential donors are not lost and patients and families are afforded the best chance to donate. This is particularly true in cases where diabetes insipidus can lead to massive fluid losses in the urine, and haemodynamic collapse if not replaced actively. Diabetes insipidus is present in 46% of brain dead patients. Vasopressor support is the norm and is needed in 97% of deceased donors.[11] Basic active management during the end-of-life counselling process ensures that clinicians do not deny a patient or their family the option to donate.
In our series, all four referrals were from different doctors. Brain death and donation after circulatory death are rare events. It is important for clinicians to identify all potential cases, to make an appropriately timed referral and facilitate an optimum approach for consent. Our series highlights the fact that aspects of best practice related to timing of referral and approach for consent need to form the basis of ongoing quality improvement that reach a broad group of doctors (Table 3). SA does not have a system where we audit our end-of-life care counselling processes, which should include the routine exploration with the family of the patient's wishes towards organ and tissue donation.[12] This is a feature of many high-performing systems where organ donation is recognised as a marker of good end-of-life care.[5] In Germany, 42% of missed potential donors are in non-university hospitals without a neurosurgical service.[13] In the UK, all hospitals are required to have a designated 'clinical lead in organ donation' as a way to ensure that there is a local institutional expert who can be consulted.[14] In SA, we always have a transplant co-ordinator a telephone call away, but formally acknowledged and trained local clinical links, as in the UK system, may be a model we can emulate.[15]
Organ donation is always an altruistic act from the donor and their family. No financial incentive is provided. It is important to note that the organ donation registry is not considered an advance directive in SA, and legally the next of kin must and will always be approached for consent. This consent can be withdrawn at any point prior to the organ recovery operation, as it was in our first case. Organ donation in the public sector is also an altruistic act by the referring hospital, with no system in place to ensure that the cost of donor work-up, maintenance and organ recovery is recovered by the hospital. This may function as a disincentive for smaller hospitals to contribute actively. In the private sector, costs of the donor maintenance and organ recovery are recovered from the hospital allocated the organs, and co-ordinated by the private transplant co-ordinator, but theatre time often has to be negotiated as elective cases may need to be rescheduled.
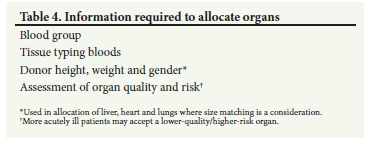
Allocation of organs in SA is on a national basis for patients meeting urgent listing criteria for heart, lungs and liver, as these patients face imminent death without a transplant (Table 4). If there is no urgent national listing, as in the case of the donor in this case series, the organs are allocated based on the allocation criteria within that province. For heart, lungs and liver this is based on severity of illness, but is offered to the waiting list within the healthcare system (public or private) of the donor first. Only when there is no suitable recipient on the waiting list is it offered to the other healthcare system. In the case of this donor, the lack of suitable state patients on the waiting list resulted in these organs being allocated to the private sector. Kidneys are always allocated within the province of the donor, and in the Western, Eastern and Northern Cape provinces are allocated through an online points-based allocation system. This system factors in age, time on the waiting list and crossmatch status to optimise long-term transplant outcomes. The first kidney is allocated to the patient with the highest score in the healthcare system of the donor, while the second kidney is allocated to the patient with the highest score on a combined list of public and private patients. Renal allocation practice is governed regionally and ensures that the donor hospital system always receives at least a kidney from the resources devoted to organ recovery.
Conclusion
It is possible for small public hospitals to successfully support organ transplantation in SA. This is dependent on motivated and informed clinicians referring all potential donors. There is a need for continued quality improvement in terms of our systems and educational efforts to further increase the donor pool and improve access to transplantation.
Declaration. None.
Acknowledgements. We thank the treating clinical teams for the referrals and the families who thoughtfully considered donation in their time of grief.
Author contributions. All the authors contributed to the conceptualisation of the study, data interpretation, and approval of the final version in line with the International Committee of Medical Journal Editors. DT and EDP wrote the first draft.
Funding. None.
Conflicts of interest. None.
References
1. National Department of Health, South Africa. A District Hospital Service Package for South Africa 2002. Pretoria: NdoH, 2002. http://www.kznhealth.gov.za/norms.pdf (accessed 6 June 2022). [ Links ]
2. Thomson D, Joubert I, de Vasconcellos K, et al. South African guidelines on the determination of death. South Afr J Crit Care 2021;37(1b):41-54. https://doi.org/10.7196/sajcc.2021.v37i1b.466 [ Links ]
3. Du Toit T, Manning K, Thomson D, et al.. A 10-year analysis of organ donor referrals to a South African tertiary public sector hospital. S Afr Med J 2020;110(2):132-134. https://doi.org/10.7196/samj.2020.v110i2.14125 [ Links ]
4. Bookholane H, Michaelides A, Prins L, et al. Factors influencing consent rates of deceased organ donation in Western Cape Province, South Africa. S Afr Med J 2020;110(3):204-209. https://doi.org/10.7196/samj.2020.v110i3.14227 [ Links ]
5. Rodríguez-Arias D, Wright L, Paredes D. Success factors and ethical challenges of the Spanish Model of organ donation. Lancet 2010;376(9746):1109-1112. https://doi.org/10.1016/s0140-6736(10)61342-6 [ Links ]
6. Schnitzler MA, Whiting JF, Brennan DC, et al. The life-years saved by a deceased organ donor. Am J Transplant 2005;5(9):2289-2296. https://doi.org/10.1111/j.1600-6143.2005.01021.x [ Links ]
7. Moosa M. The state of kidney transplantation in South Africa. S Afr Med J 2019;109(4):235-240. https://doi.org/10.7196/samj.2019.v109i4.13548 [ Links ]
8. Thomson D. Organ Donation: From Death to Life. https://www.coursera.org/learn/organ-donation (accessed on 6 June 2022). [ Links ]
9. Du Toit T, Manning K, Thomson D, et al. Kidney transplantation utilising donors after circulatory death - the first report from the African continent. Transplantation 2018;102:S493-S494. https://doi.org/10.1097/01.tp.0000543311.81537.58 [ Links ]
10. National Health Service, UK. Potential Donor Audit 2011 - 2012. NHS, 2012. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/3180/pda_report_1112.p (accessed on 6 June 2022). [ Links ]
11. Salim A, Martin M, Brown C, et al. Complications of brain death: Frequency and impact on organ retrieval. Am Surg 2006;72(5):377-381. https://doi.org/10.1177/000313480607200502 [ Links ]
12. Barber KM, Hussey JC, Bond ZC, et al. The UK National Potential Donor Audit. Transplant Proc 2005;37(2):568-570. https://doi.org/10.1016Zj.transproceed.2004.12.088 [ Links ]
13. Esser G, Kolbrink B, Borzikowsky C, et al. Evaluation of underidentification of potential organ donors in German hospitals. Plos ONE 2020;15(11):e0242724. https://doi.org/10.1371/journal.pone.0242724 [ Links ]
14. Murphy PG, Smith M. Towards a framework for organ donation in the UK. Br J Anaesth 2012;108(Suppl 1):i56-i67. https://doi.org/10.1093/bja/aer402 [ Links ]
15. Muller E, Thomson D, McCurdie F. Transplantation in South Africa. Transplantation 2015;99(4):643-645. https://doi.org/10.1097/tp.0000000000000712 [ Links ]
 Correspondence:
Correspondence:
D Thomson
david.thomson@uct.ac.za
Accepted 26 July 2022














