Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 n.12 Pretoria Dec. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i12.16689
IN PRACTICE
MEDICINE AND THE ENVIRONMENT
Fatal infective necrotising fasciitis: Complication following Naja nigricincta nigricincta bite (western barred spitting cobra/zebra snake)
E L SaaimanI; P J (Christo) BuysII
IMB ChB; MMed (Anaesth); Anaesthetist, private practice, Windhoek, Namibia; Member of the Namibian Snakebite Interest Group
IIMB ChB, MMed (ORL); Ear, nose and throat surgeon, private practice, Windhoek, Namibia; Namibian snakebite management expert; Founding member and head of the Namibian Snakebite Interest Group
ABSTRACT
Wound infections following cytotoxic snakebites are common. Bites from Naja nigricincta nigricincta (an African spitting cobra) usually present as severe dermonecrosis spreading within the subdermal fascia layer. Primary infections can follow inoculation of the snake's oral flora during the bite, worsening the dermonecrosis into infective necrotising fasciitis. We report the case of a 21/2-year-old boy who presented with infective (Proteus vulgaris) necrotising fasciitis after an N. n. nigricincta bite, resulting in multiple-organ failure and death. A P. vulgaris with the same antibiotic profile was cultured from the mouth of the snake.
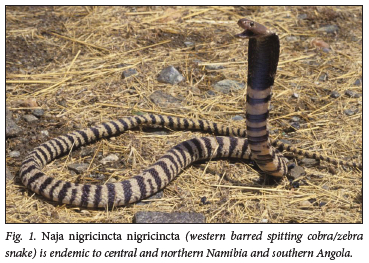
Naja nigricincta nigricincta (western barred spitting cobra/zebra snake) (Fig. 1) is endemic to central and northern Namibia as well as southern Angola. It is responsible for most of the venomous snakebites seen in these areas of Namibia. The majority of bites occur at night while the victims are asleep. These are often babies and small children, who suffer high mortality. The snake frequents human habitation, both urban and rural, and is often found inside dwellings.[1,2]
Like other African spitting cobras, namely Naja mossambica and Naja nigricollis, N. n. nigricincta injects its highly cytotoxic venom into the subdermal fascia layer. Necrosis spreads rapidly in a plane between skin and deeper-lying muscles. The subcutaneous necrotic spread usually extends considerably further than the overlying skin discoloration.[1-4]
Apart from severe local swelling and blue discoloration of the skin overlying the bite site,[1,2] victims of N. n. nigricincta bites can also present with drowsiness, convulsions, raised serum creatine kinase (CK), haematological features of haemolysis, and a raised international normalised ratio (INR).[5] The last-mentioned three abnormalities have only been reported in association with N. n. nigricincta bites and were thought to be venom-induced systemic manifestations.[1,5] Kidney failure has been reported (authors' clinical experience). Children have high morbidity and mortality, but the specific pathogenesis is still unclear. They often present with excessive swelling, and are prone to develop systemic inflammatory response syndrome (SIRS), progressing to multiple-organ dysfunction syndrome and death (authors' clinical experience).
Specific antivenom is not available. The accepted southern African protocol for the treatment of spitting cobra bites, i.e. intravenous South African Institute for Medical Research (SAIMR) polyvalent antivenom followed by late debridement, was historically part of the routine treatment of N. n. nigricincta bites.[6,7] However, even very large doses of up to 200 mL, administered early (within hours) following the bite, were unable to prevent severe disfiguration and function loss. This protocol was eventually abandoned in favour of emergency surgical debridement and antibiotics without antivenom administration (proposed by author PJCB in 1976), which resulted in much more favourable functional and cosmetic clinical outcomes.[1,5]
An exception to the above management are bites in the face. Most of the bites that have been encountered in the face and head regions occurred in children, many of whom presented very late without receiving any treatment. Contrary to expectation, the resulting destructive dermonecrosis was much milder than that encountered after bites on limbs. Whether this is due to different anatomy of the head and face compared with the extremities, or factors such as blood supply or fascial compartments, is open to speculation. In the majority of these cases, later surgery with minimal debridement and small skin grafts were sufficient (clinical experience gained over the past 46 years - PJCB). With this in mind, the decision regarding surgery should be based on individual circumstances in consultation witha snakebite expert and a plastic surgeon.
Case presentation and management
A 21/2-year-old boy was admitted to the emergency department at 21h10, 20 minutes after being bitten by a snake while asleep in his bed. The snake was found under his pillow, identified as N. n. nigricincta, and removed for relocation by the local snake expert and handler.
On admission, the patient was uncomfortable and restless. There were puncture marks on both his upper and lower right eyelids, with blue discoloration and marked swelling. The right side of his face was slightly swollen. Blood pressure, pulse and respiratory rates, oxygen saturation and temperature were within normal limits. A full blood count, urea and electrolytes, liver function tests, and measurement of C-reactive protein and CK were requested. Marked neutrophilia with elevated lactate dehydrogenase and CK levels was present (Tables 1 - 3).
The findings on ophthalmological examination were normal. The patient was admitted to the intensive care unit under the care of a paediatrician. Treatment was initiated with intravenous fluids, ampicillin-cloxacillin, dexamethasone, paracetamol and morphine. During the night, the patient's pulse rate gradually increased to a sinus tachycardia of 160 bpm. Urinary output decreased, glucose levels rose to >20 mmol/L, and the inflammatory markers C-reactive protein, white blood cell count and platelets, as well as potassium, urea, aspartate transaminase, lactate dehydrogenase and CK (25 690 IU/L) levels, were increased (Tables 1 - 3). Treatment was altered accordingly, with increased fluids, forced diuresis and insulin infusion.
A plastic surgery consultation was sought the next morning. There was severe blue/black discoloration of the skin around the right eye. Areas of blue discoloration were present in the right temporal and submandibular regions. The whole face was swollen, noticeably more so on the right. The areas of discoloration were marked and documented. The patient was closely observed for any deterioration.
During the course of the day the patient became progressively more pyrexial (temperature 38.3°C), and the pulse rate increased to 200 bpm. The trunk and extremities appeared mottled, and he was very restless. By 17h00 the blue discoloration involved the entire right side of his face. Excessive swelling of his neck was present, and the imminent airway compromise necessitated tracheal intubation (22 hours after the bite). At 20h00 the temperature was 39.3°C, the pulse rate 220 bpm; the serum potassium level (measured at 10h00) was 5.8 mmol/L. The discoloration and swelling were still spreading. It was decided to take the patient to theatre for surgical debridement.
Foul-smelling liquified fascia and subdermal tissues were found upon incision. All visible necrotic tissue from the right temporal and subdermal areas was removed and a swab was taken for microscopy, culture and antibiotic sensitivity (MC&S). The latter yielded a Proteus vulgaris, sensitive to amikacin, ciprofloxacin, cefepime, gentamicin, meropenem, piperacillin-tazobactam and sulfamethoxazole-trimethoprim and resistant to ampicillin, amoxycillin-clavulanate, cefuroxime, cefoxitin, ceftriaxone and imipenem (Table 4). Blood cultures did not grow any organisms.
Post debridement the patient remained tachycardic (pulse rate 220 bpm) hypotensive and pyrexial. Piperacillin-tazobactam was added and an adrenaline infusion was started. At 05h00 the next morning (32 hours after the bite), the patient went into asystole. A sinus rhythm was regained after cardiopulmonary resuscitation (CPR). During the next 3 hours the patient experienced another five episodes of pulseless electrical activity necessitating CPR and was successfully resuscitated.
Despite full inotropic support, ventilation and aggressive supportive treatment, the Glasgow Coma Score remained 3/10T with fixed dilated pupils and a persistent acidosis. The patient was too unstable to leave the unit for a computed tomography brain scan or another debridement in theatre. Very poor urine output was achieved. An echocardiogram done 40 hours after the bite showed global myocardial hypokinesia, a dilated left ventricle and a left ventricular ejection fraction of 38%.
The patient remained critical and unstable. On the 4th day after the bite, the necrotic demarcation had progressed to the nipple line. Four days and 12 hours after the bite, the patient went into asystole and could not be resuscitated. A final diagnosis of N. n. nigricincta snakebite complicated by Gram-negative P. vulgaris necrotising fasciitis terminating in septicaemic shock was made.
At the time of the patient's death, the snake was still in captivity, awaiting relocation. In view of the P. vulgaris cultured from the patient's wounds and the resulting clinical features, it was decided to take swabs for MC&S from the snake's mouth, pharynx, venom, skin and cloaca.
A P. vulgaris with the same antibiotic sensitivity and resistance was cultured from the snake's mouth, nasopharynx and cloaca. Other organisms cultured from the snake were Morganella morganii, Salmonella spp., Enterococcus faecalis and Pseudomonas aeruginosa (Table 4).
Discussion
Necrotising fasciitis is a fulminant and progressive bacterial infection. It spreads rapidly through fascial planes, causing extensive tissue destruction, and has an aggressive clinical course with a high risk of multiple-organ failure and a significant mortality rate.[8] Children suffering from necrotising fasciitis have an overall mortality of 15.4%.[9]
Musculoskeletal tissue damage evokes an immunothrombotic survival acute-phase response. Continued tissue destruction as seen in necrotising fasciitis elicits dysregulation of this response, leading to sepsis-induced coagulopathy (SIC) and SIRS. Both SIC and SIRS may be complicated by critical illness corticosteroid insufficiency, deep-vein thrombosis, microangiopathy and subsequent multiple-organ failure.[10-12]
The diagnosis of necrotising fasciitis is mainly clinical.[8,11,13] Clinical indicators are fever, crescendo pain, rapidly progressive erythema, swelling and skin ischaemia with blisters, bullae and necrosis.'11- Surgical exploration with tissue biopsy remains the gold standard. The presence of foul-smelling 'dishwater' liquefaction fluid and loosely adherent fascia are diagnostic.[8,11,13]
Owing to the thrombogenic nature of necrotising fasciitis, antibiotics are unable to penetrate the necrotic infected tissue. Early diagnosis is essential, as mortality is directly proportional to time to intervention. Treatment consists of aggressive haemodynamic resuscitation and prompt and adequate surgical debridement, followed by appropriate antibiotics. Removing necrotic, toxic, infected and infarcted tissue with surgical debridement improves subsequent antibiotic penetration. Serial surgical debridements are almost always needed.[10,11,13]
One of the most important complications of snakebite with local envenoming is soft-tissue infection.[14,15] Venom causing cytotoxic injuries with extensive tissue destruction and devitalisation predisposes the wound to bacterial infection from the snake's indigenous oral flora introduced through the fangs. Dermonecrosis resulting from venom injury can therefore easily expand, and degrades into a necrotising soft-tissue infection, i.e. necrotising fasciitis.[16-20]
Necrotising fasciitis following snakebite has been reported from India,[21,22] Nigeria,[23] French Guiana,[14] Taiwan,[24] Zambia[25] and Vietnam,'26- and seems to be more common following bites by Naja atra as reported from Taiwan and China. Serratia marcescens, Aeromonas hydrophile, Aeromonas sobria, M. morganii, Enterococcus spp. and Bacteroides fragilis have all been implicated as causative organisms. [14,21,22,24,26]
A recent study from China suggests that, as for necrotising fasciitis, early radical surgical debridement (venom decontamination and removing of devitalised tissue) and empirical broad-spectrum antibiotics (combating invading bacteria) should be considered as treatment of severe cytotoxic cobra envenomation in order to restrict local tissue damage.[19]
Prior to managing this case, we did not recognise or fully appreciate the degree to which an underlying necrotising fasciitis or a severe inflammatory response complicates and plays a role in the clinical presentation of victims of N. n. nigricincta snakebites, and probably misinterpreted it as direct effects of envenomation. Such obvious clinical features of a full-blown, fulminant necrotising fasciitis as seen in this specific case are not the norm. The raised CK levels, high INRs and haemolysis previously identified by us may all be features of a severe inflammatory response and not an indication of systemic venom manifestations, as we thought. Both venom-induced tissue destruction (damage-associated molecular pattern) and a bacterial infection (pathogen-associated molecular pattern) may result in a systemic inflammatory response.[27]
Emergency debridement, appropriate parenteral antibiotics and specific antivenom are joint priorities in the treatment of necrotising fasciitis following snake envenomation.
Literature studies on secondary wound infections, our own clinical experience and data from a recent unpublished Namibian study culturing bacteria from the oral cavity of N. n. nigricincta are the current basis for antibiotic selection.[18,20]
The obvious need for specific antivenom needs to be readdressed. We live in Africa. We have limited resources. Both the South African Vaccine Producers/SAIMR (using N. mossambica venom) and Echi-Tab-ICP-plus (using N. nigricollis venom) polyvalent antivenoms are available in southern Africa and are purported to possess cross-neutralisation effectivity against N. n. nigricincta envenomation. Studies evaluating the neutralisation and potency of both these antivenoms are currently being conducted. If potent enough, we can reintroduce one of these antivenoms into our protocol. If not, developing a monospecific antivenom might be the only suitable alternative.
Conclusion
The non-recognition or delayed treatment of necrotising fasciitis may in part be the cause of the high morbidity and mortality observed in children bitten by N. n. nigricincta.
When dealing with African spitting cobra bites, and specifically N. n. nigricincta bites, the clinician needs to be aware of and have a high index of suspicion for the development of infective necrotising fasciitis. The fatal course of the case reported underlines the aggressive clinical course of necrotising fasciitis. Early recognition combined with prompt and aggressive intervention are essential for survival.
Declaration. None.
Acknowledgements. Dr Carel Haumann, clinical pathologist, and Dr Steffan Bau, paediatrician in charge.
Author contributions. ELS wrote the manuscript. PJCB advised, oversaw and supervised the research and compilation of the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Buys PJC. Medical Management of Snakebite in Namibia. Windhoek, Namibia: Gamsberg Macmillan, 2003. [ Links ]
2. Griffen M. The Zebra snake antivenom project. Travel News Namibia, 2001. https://www.travelnewsnamibia.com/news/stories/featured-stories/the-zebra-snake-antivenom-project/ (accessed 22 October 2019). [ Links ]
3. Warrell DA, Greenwood BM, Davidson NM, Ormerod LD, Prentice CR. Necrosis, haemorrhage and complement depletion following bites by the spitting cobra (Naja nigricollis). Q J Med 1976;45(177):1-22. https://doi.org/10.1093/oxfordjournals.qjmed.a067448 [ Links ]
4. Tilbury CR. Observations on the bite of the Mozambique spitting cobra (Naja mossambica mossambica). S Afr Med J 1982;61:308-313. [ Links ]
5. Saaiman E, Buys P. Spitting cobra (Naja nigricincta nigricincta) bites complicated by rhabdomyolysis, possible intravascular haemolysis, and coagulopathy. S Afr Med J 2019;109(10):736-740. https://doi.org/10.7196/SAMJ.2019.v109i10.14103 [ Links ]
6. Blaylock RS. The identification and syndromic management of snakebite in South Africa. S Afr Fam Pract 2005;47(9):46-53. https://doi.org/10.1080/20786204.2005.10873288 [ Links ]
7. World Health Organization. Guidelines for the prevention and clinical management of snakebite in Africa. Brazzaville: World Health Organization Regional Office for Africa, 4 February 2010:44-52. [ Links ]
8. https://www.who.int/publications/i/item/9789290231684 (accessed 13 April 2016). [ Links ]
9. Davoudian P, Flint NJ. Necrotizing fasciitis. Contin Educ Anaesth Crit Care Pain 2012;12(5):245-250. https://doi.org/https://doi.org/10.1093/bjaceaccp/mks033 [ Links ]
10. Zundel S, Lemaréchal A, Kaiser P, Szavay P. Diagnosis and treatment of pediatric necrotizing fasciitis: A systematic review of the literature. Eur J Pediatr Surg 2017;27(2):127-137. https://doi.org/10.1055/s-0036-1584531 [ Links ]
11. Moore-Lotridge SN, Gibson BHY, Duvernay MT, Martus JE, Thomsen IP, Schoenecker JG. Pediatric musculoskeletal infection: An update through the four pillars of clinical care and immunothrombotic similarities with COVID-19. J Pediatr Orthop Soc North Am 2020;2(2). https://doi.org/10.55275/JPOSNA-2020-124 [ Links ]
12. Hysong AA, Posey SL, Blum DM, et al. Necrotizing fasciitis: Pillaging the acute phase response. J Bone Joint Surg Am 2020;102(6):526-537. https://doi.org/10.2106/JBJS.19.00591 [ Links ]
13. An TJ, Benvenuti MA, Mignemi ME, Thomsen IP, Schoenecker JG. Pediatric musculoskeletal infection: Hijacking the acute-phase response. JBJS Rev 2016;4(9):e4. https://doi.org/10.2106/JBJS.RVW.15.00099 [ Links ]
14. Stevens DL, Bryant AE. Necrotizing soft-tissue infections. N Engl J Med 2017;377(23):2253-2265. https://doi.org/10.1056/NEJMra1600673 [ Links ]
15. Houcke S, Resiere D, Lontsingoula GR, et al. Characteristics of snakebite-related infection in French Guiana. Toxins (Basel) 2022;14(2):89. https://doi.org/10.3390/toxins14020089 [ Links ]
16. Saravia-Otten P, Gutierrez J, Arvidson S, Thelestam M, Flock J-I. Increased infectivity of Staphylococcus aureus in an experimental model of snake venom-induced tissue damage. J Infect Dis 2007;196(5):748-754. https://doi.org/10.1086/520537 [ Links ]
17. Resiere D, Gutierrez JM, Neviere R, Cabie A, Hossein M, Kallel H. Antibiotic therapy for snakebite envenoming. J Venom Anim Toxins Includ Trop Dis 2020;26:e20190098. https://doi.org/10.1590/1678-9199-jvatitd-2019-0098 [ Links ]
18. Sadeghi M, Barazandeh M, Zakariaei Z, et al. Massive cutaneous complications due to snakebite: A case report and literature review. Clin Case Rep 2021;9(5):e04129. https://doi.org/10.1002/ccr3.4129 [ Links ]
19. Garg A, Sujatha S, Garg J, Acharya NS, Parija SC. Wound infections secondary to snakebite. J Infect Dev Ctries 2009;3(3):221-223. https://doi.org/10.3855/jidc.39 [ Links ]
20. Lin JH, Sung WC, Mu HW, Hung DZ. Local cytotoxic effects in cobra envenoming: A pilot study. Toxins (Basel) 2022;14(2):122. https://doi.org/10.3390/toxins14020122 [ Links ]
21. Wagener M, Naidoo M, Aldous C. Wound infection secondary to snakebite. S Afr Med J 2017;107(4):315-319. https://doi.org/10.7196/SAMJ.2017.v107i4.12084 [ Links ]
22. Kaur H, Mahajan G. An interesting case of snake bite with necrotizing fasciitis: A case report. J Pediatr Crit Care 2018;5(3):91-93. https://doi.org/10.21304/2018.0503.00396 [ Links ]
23. Chidambaram M, Charan MSP, Saraga K, Paramasivam JD, Sujatha B. Necrotizing fasciitis due to Serratia marcescens infection following snake bite. Indian J Pediatr 2022;89(4):414. https://doi.org/10.1007/s12098-021-04031-w [ Links ]
24. Abhulimhen-Iyoha B, Oguejiofor C, Ogonor E. Venomous snake bite in children: A case report from Nigeria. Int J Med Pharm Case Rep 2018;11(1):1-7. https://doi.org/10.9734/ijmpcr/2018/40082 [ Links ]
25. Tsai Y-H, Hsu W-H, Huang K-C, Yu P-A, Chen C-L, Kuo LT. Necrotizing fasciitis following venomous snakebites in a tertiary hospital of southwest Taiwan. Int J Infect Dis 2017;63:30-36. https://doi.org/10.1016/j.ijid.2017.08.005 [ Links ]
26. Banda CH, N'gambi C. Necrotizing fasciitis with mediastinitis following snakebite envenomation. SAGE Open Med Case Rep 2019;7:2050313X18823090. https://doi.org/10.1177/2050313X18823090 [ Links ]
27. Le HQ, Nguyen NTT, Vo TNA, et al. Envenoming by king cobras (Ophiophagus hannah) in Vietnam with cardiac complications and necrotizing fasciitis. Toxicon 2021;200:127-133. https://doi.org/10.1016/j.toxicon.2021.07.007 [ Links ]
28. Chakrabotry RK, Burns B. Systemic inflammatory response syndrome. Treasure Island, Fla.: StatPearls, 2022. https://www.ncbi.nlm.nih.gov/books/NBK547669/ (accessed 12 June 2022). [ Links ]
 Correspondence:
Correspondence:
E Saaiman
estasaaiman@gmail.com
Accepted 15 August 2022














