Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11b Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11b.16825
CASE REPORT
Aneurysm caused by intimomedial mucoid degeneration: A case report
R NshutiI; N S SitholeII
IMMed (Surg), Cert Vase (SA) ; Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
IIMB ChB; Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
ABSTRACT
Intimomedial mucoid degeneration (IMMD) is characterised by aneurysm formation following mucin deposition in the intima and media, with elastic tissue degeneration of the arterial wall. IMMD aneurysms have been sporadically reported, with a series of 22 cases by Abdool-Carrim et al. emanating from the University of Natal, Durban, South Africa. We report on a patient who presented with a ruptured abdominal aortic aneurysm. IMMD was confirmed on histological examination of a biopsy specimen taken during open repair of the aneurysm.
Aneurysms due to intimomedial mucoid degeneration (IMMD) are rare. They were first described in South Africa (SA) by Decker et al. in 1977.[1] Subsequently, a case series from the University of Natal was reported by Abdool-Carrim et al.[2] Katz et al.[3] stated that to their knowledge, only 24 cases had been reported in the medical literature at the time of writing. IMMD is characterised by aneurysm formation following mucin deposition in the intima and media, with subsequent degeneration of elastic tissue in the arterial wall. We report on a patient with IMMD operated on at Pietersburg Hospital in Polokwane, Limpopo Province, SA.
Case report
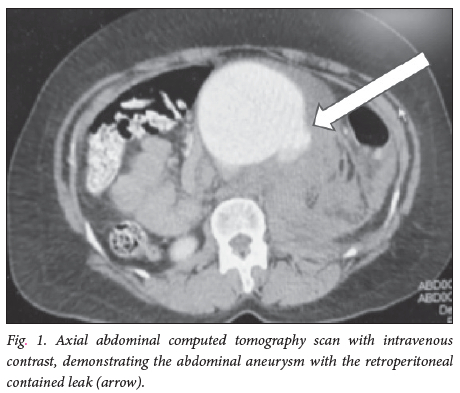
A 49-year-old woman was referred from Tshilidzini Hospital, Shayandima, Limpopo, with a ruptured abdominal aortic aneurysm. On arrival at Pietersburg Hospital, she was hypotensive and had a low haemoglobin concentration and renal impairment. The hospital's massive blood transfusion protocol was initiated and activated. A computed tomography scan performed prior to referral to the Department of General Surgery demonstrated a ruptured infrarenal aortic aneurysm. The patient was prepared for open surgical repair. Intraoperatively, the diagnosis of IMMD was suspected because no intraluminal thrombus was identified, while the aortic wall was found to be thin and frail. The surgical repair was difficult owing to copious oozing from the suture line despite all the necessary precautions. Fresh-frozen plasma and platelets were given intraoperatively, and postoperatively the patient was admitted to the intensive care unit on high doses of inotropes for ongoing resuscitation. During the postoperative period, she developed acute renal failure requiring dialysis. She recovered gradually, was transferred to the normal surgical ward, and was discharged after 3 weeks in a stable condition. She is being followed up and monitored, in particular because of her renal function, which was recovering at the time of writing.
Discussion
IMMD was first described in SA in 1977,[1] and since then 87% of cases have been reported in black hypertensive females who were relatively younger than patients with atherosclerotic aneurysms. The patients identified by Abdool-Carrim et al.[2] were mostly black women (average age 52 years for patients with IMMD, with a range of 20 - 71 years, v. 65 years for those with atherosclerotic aneurysms), with an unknown aetiology. Our patient, a black woman aged 49 years, fits the previously reported profile. In the medical literature, there have been some reports of IMMD in the non-black population, but very few compared with cases in blacks.
The exact cause of IMMD remains unknown. It has mostly been reported in the large and medium vessels, but Georgios et al.[4 reported a case in the peripheral vessels, indicating that IMMD can affect other vessels, and questioning its earlier description as a disease of large and medium vessels only. IMMD does not have distinctive clinical features, and the diagnosis can only be confirmed on postoperative histological examination of the resected specimen. However, cases of IMMD are rare, and can be missed if the pathologist is not specifically looking for this condition.[5] If there are clinical grounds for suspecting IMMD, we suggest that this should be mentioned to the pathologist.
Conclusion
IMMD remains a rare disease, with unknown aetiology. It should be suspected in younger patients, particular females, who present with large aneurysms with no other underlying causes. Care should be taken to avoid complications related to this rare disease.
Declaration. None.
Acknowledgements. None.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Decker GAG, Samson ID, Schmaman A. Abdominal aneurysm in South African Negroes due to intimomedial mucoid degeneration: A clinicopathological study. Br J Surg 1977;64(7):513-516. https://doi.org/10.1002/bjs.1800640718 [ Links ]
2. Abdool-Carrim ATO, Robbs JV, Kagwa AM, Kenoyer G, Cooper K. Aneurysms due to intimomedial mucoid degeneration. Eur J Vasc Endovasc Surg 1996;11(3):324-329. https://doi.org/10.1016/s1078-5884(96)80079-7 [ Links ]
3. Katz JR, West DL, Bui JT, et al. Endovascular treatment of intimomedial mucoid degeneration. J Vasc Interv Radiol 2008;19(12):1765-1768. https://doi.org/10.1016/j.jvir.2008.08.019 [ Links ]
4. Georgios T, Skripochnik E, Landau D, Wain RA, Tassiopoulos AK. Intimomedial mucoid degeneration of the peripheral arteries. J Vasc Surg Cases Innov Tech 2019;5(4):452-455. https://doi.org/10.1016/j.jvscit.2019.04.005 [ Links ]
5. Wiskott K, Genet P, Lobrinus JA, Fracasso T, Lardi C. Intimomedial mucoid arterial degeneration, a rare arterial disorder of forensic significance. Forensic Sci Med Pathol 2019;15(4):591-594. https://doi.org/10.1007/s12024-019-00154-x [ Links ]
 Correspondence:
Correspondence:
R Nshuti
rnshuti1@gmail.com
Accepted 7 September 2022














