Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11b Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11b.16829
CASE REPORT
An unusual case of pyogenic liver abscess during pregnancy
M P ShadwellI; T GviliaII
IMB ChB ; Department of General Surgery, Pietersburg Hospital, Limpopo Academic Health Complex, and School of Medicine, University of Limpopo, Polokwane, South Africa
IIFCS (SA), PhD; Department of General Surgery, Pietersburg Hospital, Limpopo Academic Health Complex, and School of Medicine, University of Limpopo, Polokwane, South Africa
ABSTRACT
Pyogenic liver abscess (PLA) is a condition involving bacterial abscess formation within the liver parenchyma. Despite significant changes in medicine involving improved diagnostic techniques and management strategies, the incidence of PLA has remained largely unchanged. We present an unusual case of PLA during pregnancy.
Since the first article on pyogenic liver abscesses (PLAs) was published in 1938 (cited by Townsend et al.[1]), the incidence of the condition has decreased, with a change in epidemiology and aetiology. We report a case of PLA in a young pregnant woman with no predisposing medical conditions.
Case report
A 22-year-old woman was referred to the Department of Internal Medicine at Pietersburg Hospital in Polokwane, Limpopo Province, South Africa. An ultrasound scan at her local district hospital had confirmed that she was 18 weeks pregnant. She had no known medical conditions, and gave a complicated history of her course of illness. She had initially presented to her local hospital a month earlier after an acute onset of general malaise, fever and abdominal pain. She was diagnosed with a liver abscess, aetiology unknown, and managed conservatively with antibiotics. She reported that she had improved significantly and had been discharged. However, her original symptoms returned 1 week later, this time accompanied by a productive cough, shortness of breath and orthopnoea.
On arrival at Pietersburg Hospital she was tachycardic and tachypnoeic, with a normal blood pressure, temperature and oxygen saturation on room air. She was unable to lie flat, and appeared acutely unwell. She had conjunctival pallor and bilateral pretibial pitting oedema extending to the knee, but showed no jaundice. Cardiovascular examination revealed only a tachycardia, while respiratory examination revealed decreased air entry in the right mid zone, with absent breath sounds in the right lower zone. On abdominal examination the abdomen was found to be soft, with no rebound tenderness or peritonism. The liver was palpable 2 cm below the costal margin, with dullness to percussion giving an approximate liver span of 20 cm. She had a gravid uterus 2 cm below the umbilicus. A chest radiograph showed a significantly raised right hemidiaphragm, with collapse consolidation of the right lower lobe and a pleural effusion. Blood tests showed a normocytic anaemia with normal iron levels, serum folate and vitamin B12, normal renal function, elevated canalicular enzymes, prothrombin time and septic and inflammatory markers, and a decreased serum albumin level. HIV serology was negative.
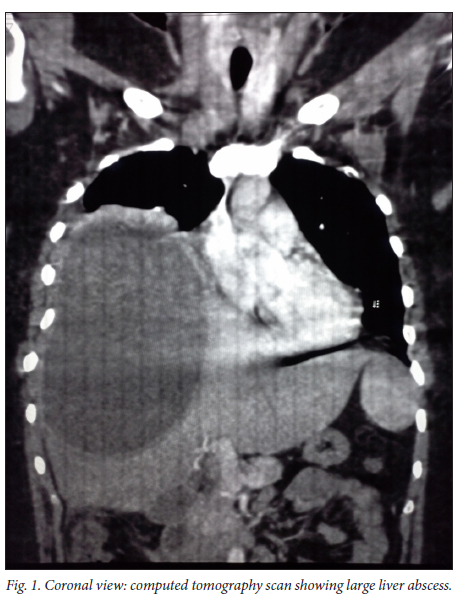
Because of the recent diagnosis of liver abscess and no definitive proof of resolution, the diagnosis of an unresolved liver abscess was made, complicated by a nosocomial pneumonia with concern regarding a hepatic pleural fistula and subsequent spread of the abscess. She was started on antibiotics, intravenous fluids and supportive management. An abdominal ultrasound scan demonstrated a large cystic structure within the right lobe of the liver measuring 10 χ 16 cm, with significant displacement of the right hemidiaphragm. A pleural effusion was also noted, increasing concern regarding rupture into the pleural space. Because of the size of the lesion and the high risk of complications, surgical drainage was planned. The magnetic resonance imaging scanner was unfortunately out of order, so a computed tomography (CT) scan of the upper abdomen and chest was performed. It showed a solitary encapsulated abscess in the right lobe of the liver, with no clear diaphragmatic rupture or hepatic pleural fistula, complicated by collapse consolidation of the right lower lobe of the lung (Fig. 1). Serological tests were negative for amoebic or hydatid disease, and the diagnosis of a PLA was therefore confirmed.
Based on the large size of the structure with no indication for open surgical drainage, the decision was made to prepare the patient for percutaneous drainage. Prior to the procedure, she received 2 units of cross-matched red blood cells and was counselled extensively on the risks it involved. Tests confirmed that her haemoglobin concentration, platelet count and clotting profile were adequate. Under ultrasound guidance, a drain was inserted into the abscess. Confirmation of drain placement was achieved by successful aspiration of pus and a repeat ultrasound scan after the procedure. Specimens were aspirated and sent for microbiological analysis. A total of 2 000 mL of purulent material was drained in the first 48 hours. After the procedure, the patient reported a significant improvement in her symptoms. Her condition remained stable and she opted for outpatient management. She was educated on drain and wound care, counselled on the dangers associated with a percutaneous drain, and discharged with the drain in situ, with regular follow-up scheduled. The laboratory was able to isolate a strain of Escherichia coli with a resistant pattern to second-generation cephalosporins and some penicillin-like antibiotics. At the time of submission of this case report, the patient was being followed up as an outpatient and remained stable. As the exact aetiology of the abscess is unclear, she will require further investigations to ensure her safety during the remainder of her pregnancy.
Discussion
Ochsner et al.[2] analysed 47 cases of PLA and performed the first-ever serious literature review of PLAs in 1938.[1] They noted that the incidence of the condition was higher in men than in women, with a large proportion of cases attributed to intra-abdominal infections, most commonly appendicitis.[2] They noted significantly raised mortality rates in patients with multiple abscesses, and 100% mortality in patients who were managed conservatively. As a result of advances over the past 80 years, the incidence of the disease has decreased and management principles and mortality and morbidity have improved significantly. With improvements in diagnostic imaging and antibiotic therapy and an ageing population, the epidemiology of the condition has shifted. Patients can present with numerous symptoms, some of which may be nonspecific. In all settings, patients who present with symptoms such as right upper quadrant pain, jaundice and tenderness on palpation of the right upper quadrant should receive urgent imaging, as a number of diagnoses with high morbidity and mortality rates share these presenting features. However, this specific constellation of symptoms is limited to ~10% of all cases,[1] and patients may present with any combination of the nonspecific symptoms of fever, rigors, generalised abdominal pain, nausea and vomiting, and malaise. There may also be nonspecific results on laboratory testing, which may indicate systemic inflammation or liver pathology. Ultimately, diagnostic imaging is required to evaluate these patients. Plain radiographs are of limited use, as they will only display air-fluid levels within the abscess (if present), or potential displacement of nearby structures should the abscess be large enough to cause a mass effect. Ultrasound and CT are useful in the diagnosis of liver abscess, as they make it possible to evaluate the parenchyma of the liver, and assess for space-occupying abscesses/cysts. CT scans are more sensitive than ultrasound in the detection of liver abscesses (97 - 85%).[3] However, both can be useful, with ultrasound playing a role in the low-resource setting. The aetiology of PLA has evolved significantly, with biliary tract sepsis becoming the leading cause. Other processes include translocation of bacteria from the intestines into the splanchnic venous system with haematological spread, penetrating trauma, and potentially cryptogenic causes.[4] While the micro-organism isolated from the abscess may indicate the aetiology, it is only a presumption and further work-up will be required to confirm.[3]
The approach to management of PLAs has improved dramatically since the implementation of percutaneous drainage, with surgical drainage reserved for patients with complicated disease or evidence of rupture. Indications for surgical drainage include evidence of rupture of the abscess such as peritonitis and failed percutaneous drainage.[5] In the past, multi-loculated abscesses were seen as an indication for open surgical drainage. However, even in these cases there is benefit in attempting percutaneous drainage before moving to a more invasive technique, as success with percutaneous techniques has been demonstrated.[6]
It is important to note that types of liver abscess other than pyogenic are prevalent, because management principles differ according to the causative organism. The other main type of liver abscess encountered is amoebic liver abscesses (ALAs). ALAs differ from PLAs in that, if they are detected early and remain uncomplicated, they can be managed with antibiotics alone.[7] Unfortunately, presenting features, imaging and biochemical and haematological testing are unlikely to distinguish between PLA and ALA, and serological and microbiological testing will be required.[8]
Conclusion
Patients with liver abscesses may present with nonspecific signs and symptoms. It is important to have a high index of suspicion when pathology is suspected in the right upper quadrant, while ensuring that one keeps an open mind and allows for a broad differential diagnosis. While early diagnosis and intervention in these patients are crucial to reduce associated complications, morbidity and mortality, it is important to not rush to invasive management techniques, as these may not be in the best interests of the patient.
Declaration. None.
Acknowledgements. None.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Townsend C, Beauchamp R, Evers B, Mattox K. Sabiston Textbook of Surgery. 21st ed. St Louis, Mo.: Elsevier, 2020. [ Links ]
2. Ochsner A, DeBakey M, Murray S. Pyogenic abscess of the liver: II. An analysis of forty-seven cases with review of the literature. Am J Surg 1938;40(1):292-319. https://doi.org/10.1016/S0002-9610(38)90618-X [ Links ]
3. Khim G, Em S, Mo S, Townell N. Liver abscess: Diagnostic and management issues found in the low resource setting. Br Med Bull 2019;132(1):45-52. https://doi.org/10.1093/bmb/ldz032 [ Links ]
4. Akhondi H, Sabih D. Liver Abscess. 18th ed. Treasure Island, Fla.: StatPearls Publishing, 2019. https://www.ncbi.nlm.nih.gov/books/NBK538230/ (accessed 13 September 2022). [ Links ]
5. Longworth S, Han J. Pyogenic liver abscess. Clin Liver Dis (Hoboken) 2015;6(2):51-54. https://doi.org/10.1002/cld.487 [ Links ]
6. Liu Y, Li Z, Liu A, et al. Early percutaneous catheter drainage in protecting against prolonged fever among patients with pyogenic liver abscess: A retrospective cohort study. Ann Med 2022;54(1):2269-2277. https://doi.org/10.1080/07853890.2022.2110612 [ Links ]
7. Lodhi S, Sarwari A, Muzammil M, Salam A, Smego R. Features distinguishing amoebic from pyogenic liver abscess: A review of 577 adult cases. Trop Med Int Health 2004;9(6):718-723. https://doi.org/10.1111/j.1365-3156.2004.01246.x [ Links ]
8. Neill L, Edwards F, Collin S, et al. Clinical characteristics and treatment outcomes in a cohort of patients with pyogenic and amoebic liver abscess. BMC Infect Dis 2019;19(1):490. https://doi.org/10.1186/s12879-019-4127-8 [ Links ]
 Correspondence:
Correspondence:
M P Shadwell
mikeshadwell6@gmail.com
Accepted 12 September 2022














