Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11b Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11b.16836
CASE REPORT
Advanced oesophageal cancer treated with endoscopic stent insertion: A case report
M TunI; T GviliaII
IMMed (Surg), FACS Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
IIMD, PhD Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
ABSTRACT
The majority of oesophageal cancers are squamous cell carcinomas. They have a poor prognosis. Dysphagia is regarded as the most distressing symptom of oesophageal cancer, with a profound impact on quality of life. Insertion of a self-expanding metal stent (SEMS) is one of the most effective ways to relieve dysphagia. We present a case of advanced oesophageal cancer in which a SEMS was inserted using a modified endoscopic technique.
In some parts of South Africa, the incidence of oesophageal squamous cell carcinoma is 160 per 100 000. Squamous cell carcinoma accounts for the majority of oesophageal carcinomas and has a poor prognosis. The most distressing symptom for patients with advanced oesophageal cancer is dysphagia - difficulty in swallowing, which can be uncomfortable or painful. One of the most effective ways to relieve dysphagia is inserting a self-expanding metal stent (SEMS) into the area of cancer blockage.[1,2]
Case report
A 64-year-old man was referred with a diagnosis of advanced oesophageal cancer. He was suffering from severe dysphagia. According to the referring doctors, he had already had an oesophagoscopy performed. A malignant-looking lesion had been identified at the level of 25 cm from the incisor teeth. Subsequent fluoroscopy demonstrated that it was associated with a tracheobronchial fistula. Biopsy of the lesion showed it to be an invasive, moderately differentiated, keratinising squamous cell carcinoma.
In view of the patient's severe dysphagia and the advanced stage of the oesophageal cancer, we decided to place an oesophageal stent as the initial palliative treatment. A partially covered SEMS (PC-SEMS) was inserted using the following technique:
• The procedure was performed using a forward-viewing endoscope and fluoroscopy control.
• The lesion was at 25 cm from the incisor teeth endoscopically, as reported by the previous endoscopist, and the oesophageal lumen was almost completely obliterated by tumour.
• A sphincterotome with a thin, floppy-tip guidewire was introduced into the endoscope. • The guidewire was used to identify the obliterated oesophageal lumen by applying gentle pressure while the sphincterotome was being steered into the lumen.
• Contrast was injected through the sphincterotome only after the guidewire was located in the correct position in the oesophageal lumen.
• The path into the stomach was confirmed with the radiological finding of the coiled guide located in the stomach and visualisation of the gastric mucosa after contrast injection on fluoroscopy.
• Under fluoroscopic control, a new surgical blade was strapped on the patient's chest wall where the upper margin of the lesion was identified endoscopically.
• Because of the fluoroscopic finding of an advanced lesion, we decided to insert the stent without prior dilatation of the stricture, so as not to cause more damage to the diseased oesophagus.
• The endoscope was removed while the guidewire was kept in place for stenting.
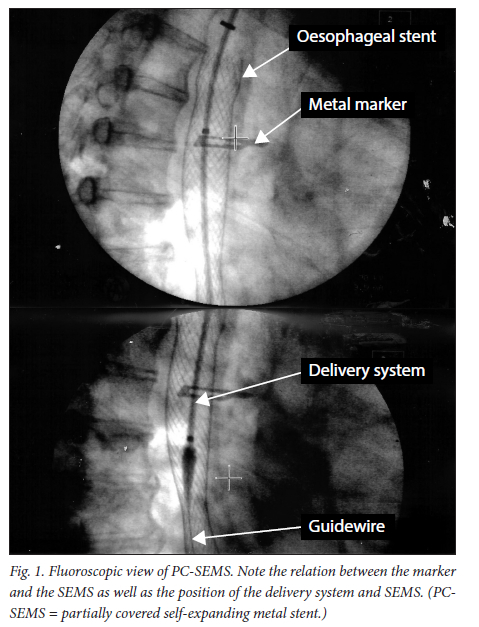
• The delivery system with a 23 × 150 mm PC-SEMS was inserted under fluoroscopic control. It was not difficult to pass the delivery system through the stricture (Fig. 1).
• The endoscope was introduced again to check the position of the SEMS and to secure the SEMS to the oesophagus with three metal clips (Fig. 2).
The patient's dysphagia improved markedly after stent insertion. He was advised not to consume solid food, as it could block the stent, and was prescribed medication to minimise the acid reflux that could result from the stent insertion.
Discussion
Oesophageal cancer is known to be a disease with a poor prognosis, with 5-year survival rates of only 10 - 15%. Most patients with advanced disease have a mean survival of only 3 - 5 months. The main symptom of oesophageal cancer is dysphagia, which has profound effects on social and physical function as well as other aspects of quality of life (QoL), especially in patients with advanced disease. It is essential to provide treatment that provides prompt and lasting palliation of dysphagia, but is associated with minimal procedure-related complications and minimal compromise of other aspects of QoL. SEMS has been recommended as a treatment that can provide rapid initial relief of dysphagia, with fewer adverse effects and lower re-intervention rates than other endoscopic therapies.[1-5] In our case, a PC-SEMS was inserted to relieve the patient's disabling dysphagia.
SEMS are available in three types: uncovered (UC-SEMS), fully covered (FC-SEMS) and PC-SEMS. A variety of covering materials (most commonly polytetrafluoroethylene) are used to prevent tumour and granulation tissue ingrowth, which occurs when a UC-SEMS is used. FC-SEMS do not have any exposed bare metal, but they are known to be more prone to migration. PC-SEMS have a small portion of bare metal at the proximal and distal ends to allow embedding into the oesophageal wall with granulation tissue, which provides the benefit of preventing stent migration, but they have the additional benefit of covering materials that protect against the ingrowth of tumour through the SEMS.[6]
In our department, we generally use PC-SEMS for malignant lesions and FC-SEMS for benign ones. When we do use PC-SEMS for benign strictures, they are removed within 2 weeks after insertion so that they do not become permanently embedded into the oesophageal wall by granulation tissue. We only use UC-SEMS in a few exceptional cases. For malignant strictures, the stent must be long enough to bridge the stricture and extend 2 - 4 cm beyond the proximal and distal ends.[6]
Radio-opaque markers are used to identify the extent of the strictures. In our case, we used a new surgical blade to mark the proximal end of the stricture. In addition, the position of the stent was confirmed by fluoroscopy as well as by endoscopy during and after the procedure.
Although insertion of SEMS is classified as a minimally invasive procedure, they are known to have immediate as well as late complications. Immediate complications include chest pain, fever, bleeding, gastrointestinal reflux, globus sensation, perforation and stent migration. Late complications include tumour ingrowth, stent migration, stent occlusion, development of an oesophageal fistula and recurrence of the stricture.[6-8] In our practice, dietary advice, lifelong oral proton pump inhibitors and regular followup are part of routine management after stent insertion. Thanks to technical advances, SEMS deployment is no longer a complex endoscopic procedure. However, in patients with high-grade strictures and those with a tortuous lumen, stent placement can pose major challenges. There are many ways to bypass these difficult strictures, such as prior oesophageal dilatations using paediatric scopes.[6] However, these can be technically challenging and can cause procedure-related complications.
Endoscopic retrograde cholangiopancreatography (ERCP) is one of the endoscopic procedures that requires technical accuracy to prevent procedure-related complications.[9] Guidewire-first cannulation has been recognised as one way to achieve technical accuracy in interventional ERCP procedures.[10] We perform this guidewire-first cannulation ERCP technique for SEMS insertion, especially when we encounter high-grade oesophageal strictures and/or a tortuous oesophageal lumen.
Conclusion
We concur with the existing medical literature on the importance of providing efficient and safe palliative treatment for patients with advanced oesophageal cancer.[2-5] We present a case of advanced oesophageal cancer in which a PC-SEMS was placed by applying the principle and technique of guidewirefirst cannulation in ERCP.
Declaration. None.
Acknowledgements. We thank all staff of the Department of General Surgery, Limpopo Academic Complex, for their contributions to endoscopy services. Without them, this article could not have been written. We also thank Mr C M Aung for his help formatting the figures.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Jobe BA, Hunter JG, Watson DI. Esophagus and diaphragmatic hernia. In: Brunicardi FC, Andersen DK, Billiar TR, et al., eds. Shwartz's Principles of Surgery. 11th ed. New York: McGraw-Hill, 2019: chapt 2. [ Links ]
2. Adamson D, Blazeby J, Nelson A, et al. Palliative radiotherapy in addition to self-expanding metal stent for improving dysphagia and survival in advanced oesophageal cancer (ROCS: Radiotherapy after Oesophageal Cancer Stenting): Study protocol for a randomized controlled trial. Trials 2014;15:402. https://doi.org/10.1186/1745-6215-15-402 [ Links ]
3. O'Hanlon DM, Callanan K, Karat D, Crisp W, Griffin SM. Outcome, survival, and costs in patients undergoing intubation for carcinoma of the esophagus. Am J Surg 1997;174(3):316- 319. https://doi.org/10.1016/s0002-9610(97)00104-9 [ Links ]
4. Watkinson AF, Ellul J, Entwistle K, Mason RC, Adam A. Esophageal carcinoma: Initial results of palliative treatment with covered self-expanding endoprostheses. Radiology 1995;195(3):821-827. https://doi.org/10.1148/radiology.195.3.7538682 [ Links ]
5. Sreedharan A, Harris K, Crellin A, Forman D, Everett SM. Interventions for dysphagia in esophageal cancer. Cochrane Database Syst Rev 2009, Issue 4. Art. No.: CD005048. https://doi.org/10.1002/14651858.CD005048.pub2 [ Links ]
6. Hindy P, Hong J, Lam-Tsai Y, Gress F. A comprehensive review of esophageal stents. Gastroenterol Hepatol (N Y) 2012;8(8):526-534. [ Links ]
7. Martinez JC, Puc MM, Quiros RM. Esophageal stenting in the setting of malignancy. ISRN Gastroenterol 2011;2011:719575. https://doi.org/10.5402/2011/719575 [ Links ]
8. Baron TH. Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 2001;344(22):1681-1687. https://doi.org/10.1056/NEJM200105313442206 [ Links ]
9. Talukdar R. Complications of ERCP. Best Pract Res Clin Gastroenterol 2016;30(5):793-805. https://doi.org/10.1016/j.bpg.2016.10.007 [ Links ]
10. Tse F, Yuan Y, Moayyedi P, Leontiadis GI. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev 2022, Issue 3. Art. No.: CD009662. https://doi.org/10.1002/14651858 [ Links ]
 Correspondence:
Correspondence:
M Tun
drmyinttun@outlook.com
Accepted 21 September 2022