Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11b Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11b.16821
RESEARCH
An audit on the preliminary results of endoscopic retrograde cholangiopancreatography performed in the Limpopo Academic Complex, Polokwane, South Africa
M TunI; T GviliaII; A B (Sebastian) van AsIII
IMMed (Surg), FACS; Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
IIMD, PhD; Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
IIIMMed (Surg), PhD; Department of General Surgery, Limpopo Academic Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
ABSTRACT
BACKGROUND. Endoscopic retrograde cholangiopancreatography (ERCP) is an endoscopic procedure that is an important treatment modality for the management of hepatic, pancreatic and biliary diseases. The ERCP unit in the Limpopo Academic Complex in Polokwane, South Africa, was established at the end of 2021.
OBJECTIVES. To identify areas for improvement in the new ERCP unit.
METHODS. All ERCP procedures were audited in five components: (i) room set-up; (ii) endoscope, guidewires and consumable accessories; (iii) fluoroscopy; (iv) sedation and analgesia; and (v) ERCP endoscopist and staff. These were considered the essential pillars of an ERCP unit. The quality of each component was graded in every ERCP procedure as grade 1 (very poor), grade 2 (below average), grade 3 (average), grade 4 (above average), and grade 5 (highly satisfactory).
RESULTS. Nine therapeutic ERCP procedures were performed during the period 10 January - 31 May 2022. Eighteen theatre slots were allocated for ERCP procedures during the study period, but only seven of them were utilised. The quality of ERCP unit components was highest for the sedation and analgesia component (mean grade of 4) and lowest for fluoroscopy (mean 1.8).
CONCLUSION. Establishing a new ERCP service is a task with many challenges. We present the preliminary results of the Limpopo Academic Complex ERCP unit with a view to adding our experience to the current knowledge.
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive endoscopic procedure performed using a side-viewing endoscope for direct visualisation of the ampulla of Vater, as well as direct access into the biliary and pancreatic ducts. The procedure is typically performed with the patient under deep sedation or general anaesthesia.[1]
The first successful cannulation of the ampulla of Vater was reported in 1968. After this technical breakthrough, the side-viewing endoscope was invented, mostly as a result of research activities of Japanese working groups and endoscope manufacturers. ERCP has subsequently evolved as a modality for both diagnostic procedures and therapeutic interventions in various hepatic, pancreatic and biliary diseases.[2]
Limpopo Province, with 6.01 million inhabitants in 2021, is the fifth most populated province of South Africa.[3] Health services in the province's public sector are delivered by 40 state-owned hospitals, including two tertiary hospitals, Pietersburg Hospital and Mankweng Hospital, which comprise the Limpopo Academic Complex. These are the only referral institutions in the province for patients requiring tertiary healthcare. However, although these hospitals provide a range of specialised healthcare services, there was no ERCP unit in the Limpopo Academic Complex until the end of 2021.
Through an audit, we hoped to identify areas for improvement in the newly established ERCP unit in the Limpopo Academic Complex.
Methods
All ERCP procedures performed in the Limpopo Academic Complex from 10 January to 31 May 2022 were included in the audit. The procedures were performed in the Monday theatre slot, which was allocated to a surgical firm. The team that performed the ERCPs
included one gastrointestinal endoscopist and one endoscopy nurse with the necessary experience in assisting ERCP procedures. If no nursing staff with the necessary skills were available, representatives from the ERCP consumable accessories suppliers filled the role of endoscopy nurse. Before the procedure, the patient's fitness was assessed according to the American Society of Anesthesiologists (ASA) classification. All ERCPs were performed under fluoroscopy, utilising a mobile radiological C-arm machine operated by a radiographer, with the patient under either deep sedation or general anaesthesia, administered by an anaesthetist. Procedures were rescheduled if the fluoroscopy service was unavailable. A side-viewing endoscope was used to view the ampulla of Vater and to gain access to the biliary system. The consumable accessories for the ERCP procedures, such as sphincterotomes, guidewires and stents, were purchased on an ad hoc basis from commercial suppliers committed to helping establish our ERCP service, aiding in quality control and supporting ERCP staff.
Five components, (i) room set-up; (ii) endoscope, guidewires and consumable accessories; (iii) fluoroscopy; (iv) sedation and analgesia; and (v) ERCP endoscopist and staff, were considered the essential pillars of our ERCP unit. The quality of each of these components was graded in each ERCP procedure, as follows: grade 1 (very poor); grade 2 (below average); grade 3 (average); grade 4 (above average); and grade 5 (highly satisfactory). A procedure was only defined as successful if the therapeutic aim of ERCP in that particular patient was achieved.
Results
Nine patients (2 males and 7 females) with a mean age of 45.4 years (range 28 - 76) had ERCP performed at the Limpopo Academic Complex during the period 10 January - 31 May 2022. With regard to their fitness for ERCP, 2 were classified as ASA II, 6 as ASA III and 1 as ASA IV. The indications for the procedure were obstructive jaundice due to cancer of the pancreatic head (n=2 cases), sclerosing cholangitis (n=1), cholangiocarcinoma (n=3), periampullary tumour (n=1) and choledocholithiasis (n=2).
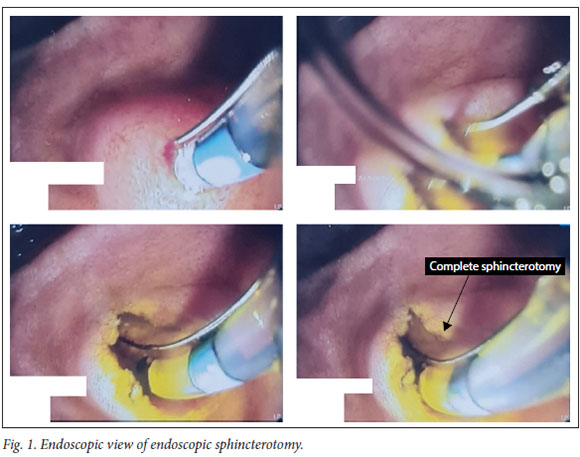
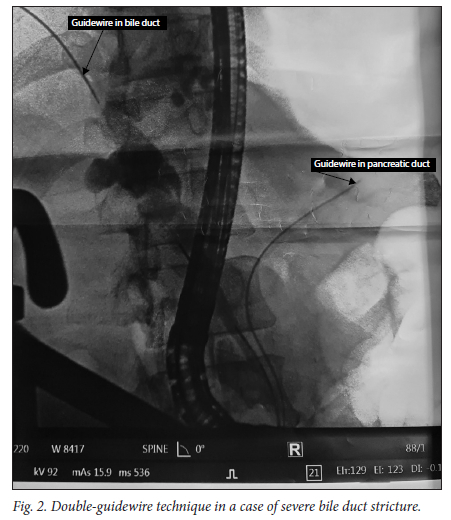
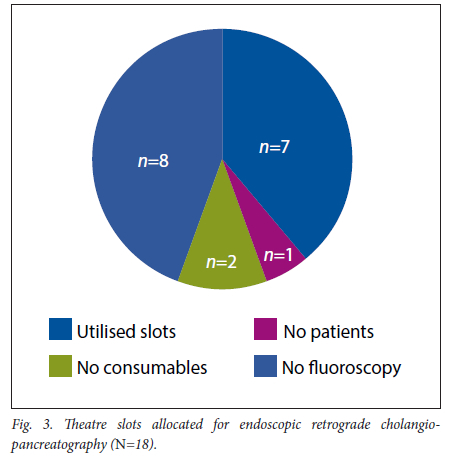
Seven ERCP procedures (n=7/9) were successful and achieved their therapeutic aim. Two procedures were not successful because of gastric outlet obstruction. Therapeutic procedures performed were endoscopic sphincterotomy (n=7/7), needleknife pre-cut papillotomy (n=1/7) and biliary stenting (n=5/7) (Figs 1 and 2). One diabetic patient (n=1/9) developed post- ERCP pancreatitis, but required conservative management only. There were no procedurerelated deaths. Eighteen theatre slots were allocated for ERCP procedures from 10 January to 31 May 2022, of which only seven were utilised (Fig. 3). The reasons for not utilising allocated slots (n=11/18) were no patients requiring ERCP at that time (n=1/11), unavailability of consumable accessories (n=2/11), and unavailability of the fluoroscopy service (n=8/11).
The quality of the ERCP unit pillars, as assessed using the five grades described above, is shown in Table 1.
Discussion
An epidemiological study by Gear et al.[4] published in 1990 suggested that 50 ERCP examinations are needed per 100 000 population each year, while in 1991 the Working Party of the Clinical Services Committee of the British Society of Gastroenterology[5] reported that the use of ERCP was rising and provided estimates of likely workload. With the advent of noninvasive tests such as magnetic resonance cholangiopancreatography and endoscopic ultrasound, ERCP has become a procedure used mostly for therapeutic purposes, and rarely for diagnostic indications.[6,7] From this perspective, the ERCP requirements reported in the epidemiological study[4] may not apply today. However, it would be difficult for a health system to provide comprehensive healthcare without ERCP services. The ERCP unit at Limpopo Academic Complex was established to provide therapeutic ERCP procedures as part of the healthcare service for the province.
The fundamentals and essentials of ERCP procedures have been extensively described in the medical literature.[2,8] Based on the available information, the ERCP unit in the Limpopo Academic Complex identified the five essential pillars of (i) room set-up; (ii) endoscope, guidewires and accessories; (iii) fluoroscopy; (iv) sedation and analgesia; and (v) ERCP endoscopist and staff.
Although the important role of ERCP is well established, evaluation of ERCP procedures is a complex process. Its clinical success may be obvious in certain procedures, such as removal of stones from the common bile duct or relief of obstructive jaundice by biliary stenting. However, in scenarios such as chronic pancreatitis or sphincter dysfunction, evaluation may not be as simple. Cost and patient satisfaction should also be considered in evaluating ERCP procedures.[2,5-7] Our initial results of successful ERCPs included 7 patients with obstructive jaundice, 2 of whom had common bile duct stones and 5 malignant lesions. In all these cases, ERCP achieved obvious clinical success. However, in patients with advanced malignant lesions, it was very difficult to judge whether treatment was worthwhile in terms of both its cost and the patients' expectations. For these patients, therapeutic ERCP offered only a palliative minimally invasive treatment and enabled them to avoid palliative surgical procedures.
Cotton[2] favoured the term 'unplanned events' over the more common 'complications' and 'adverse events'. Since ERCPs are technically very demanding endoscopies and therapeutic modalities, it can be difficult to determine at what level an unplanned event should be considered an adverse ERCP event.[2] One of our patients, who had diabetes, underwent ERCP to clear her bile duct stones, and developed post-ERCP pancreatitis. In our operation record, it was classified as an uneventful ERCP procedure. Her bile duct was cannulated with a guidewire-assisted technique, and there were no inadvertent pancreatic duct cannulations. However, we had to use a cutting diathermy mode to perform endoscopic sphincterotomy, as there was no diathermy machine with ENDO CUT mode, which is a better way to perform endoscopic sphincterotomy, in our ERCP unit. We agree with the literature that although ERCP is recognised as a relatively safe procedure, it does have high complication rates. The most common complication is post-ERCP pancreatitis. The importance of standardised recording for every ERCP procedure has also been emphasised in the literature.[9]
We performed our ERCPs with the patient under either deep sedation or general anaesthesia, in every case administered by an anaesthetist, in line with the ASA recommendation[10] that a qualified anaesthetist should always be available, especially for ASA III and IV patients. There was no procedure-related mortality in our series, and we consider that the presence of an anaesthetist, to administer sedation or anaesthesia during the ERCP, was a major contributing factor in this regard.
ERCP is a complex endoscopic procedure, and the staff involved require a specialised set of skills and knowledge.[11] To achieve proficiency in all aspects of ERCP requires several years of practical training and continuous refinement of knowledge. Moreover, the shift towards ERCP being an endoscopic procedure used mostly for therapeutic indications has posed further challenges in terms of training and transfer of skills to young endoscopists.[12-15]
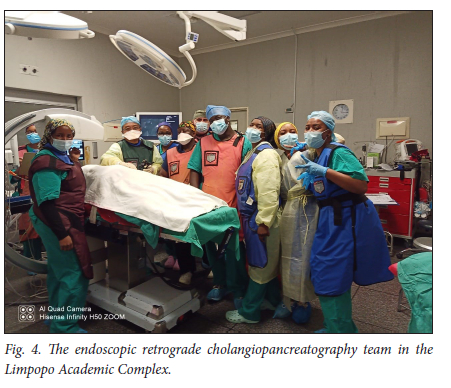
Our new ERCP unit has not been exempted from the challenges posed by lack of skilled staff. However, with the enthusiasm of the ERCP team (graded as a mean of 4.5 and a maximum of 5), we are optimistic that the process of skills transfer will be implemented successfully in the near future (Fig. 4).
ERCP is an endoscopic procedure that uses radiological imaging. It is vital for every ERCP unit to have quality fluoroscopy with minimal radiation exposure to the staff.[2,16] In our initial audit, fluoroscopy was graded as a mean of only 1.8, with a maximum of 3. This is an area that we are trying to improve.
During the study period in our initial audit, only 9 patients had therapeutic ERCP performed, 5 of whom had advanced cancer. For these procedures, we utilised 7 of 18 available theatre slots. As ours is the only ERCP unit in the public health sector in Limpopo, with its over 6 million population, these low figures could indicate a need for improvements in our current referral system and in health education for the public.
Availability of the necessary information is one of the preconditions that has been recommended to achieve an efficient healthcare system.[17] During the period of our study, there were 18 theatre slots allocated for ERCP procedures, of which only 7 were utilised. In one case, the slot was not used because no patients required ERCP at that time. However, 2 slots were not used because of unavailability of consumable accessories and 8 because no fluoroscopy service was available. These figures in our initial audit highlight areas to which we should direct extra efforts for further improvements.
Conclusion
Establishing a new ERCP service is a task with many challenges. However, ERCP is an integral part of a healthcare system providing the necessary care to the community it serves. We hope that the results of this audit will contribute to the current knowledge and assist other units in establishing ERCP services in the future.
Declaration. None.
Acknowledgements. We thank all staff of the ERCP Unit, Limpopo Academic Complex, for their dedication and help in setting up the unit. Without them, this article could not have been written. We also thank Mr C M Aung for his help formatting the figures.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Haisley KR, Hunter JG. Gallbladder and extra-biliary system. In: Brunicardi FC, Andersen DK, Billiar TR, et al., eds. Shwartz's Principles of Surgery. 11th ed. New York: McGraw-Hill, 2019: chapter 32. [ Links ]
2. Cotton PB. ERCP overview - a 30 year perspective. In: Cotton P, Leung J, eds. Advanced Digestive Endoscopy. Hoboken, NJ: Blackwell Publishing, 2008:1-8. [ Links ]
3. Statista. Total population of South Africa 2021, by province. 7 September 2022. https://www.statista.com/statistics/1112169/total-population-of-south-africa-by-province (accessed 10 September 2022). [ Links ]
4. Gear MWL, Dent NA, Colin-Jones DG, Lennard-Jones JE, Colley JRT. Future needs for ERCP: Incidence of conditions leading to bile duct obstruction and requirements for diagnostic and therapeutic biliary procedures. Gut 1990;31(10):1150-1155. https://doi.org/10.1136/gut.31.10.1150 [ Links ]
5. Working Party of the Clinical Services Committee of the British Society of Gastroenterology. Special reports: Provision of gastrointestinal endoscopy and related services for a district general hospital. Gut 1991;32(1):95-105. https://doi.org/10.1136/gut.32.L95 [ Links ]
6. Carr-Locke DL, Conn MI, Faigel DO, et al. Technology status evaluation: Magnetic resonance cholangiopancreatography: November 1998. Gastrointest Endosc 1999;49(6):858-861. https://doi.org/10.1016/S0016-5107(99)70318-4 [ Links ]
7. Mergener K, Korazek RA. Therapeutic pancreatic endoscopy. Endoscopy 2005;37(3):201-207. https://doi.org/10.1055/s-2005-860999 [ Links ]
8. Leung J. Fundamentals of ERCP. In: Cotton P, Leung J, eds. Advanced Digestive Endoscopy. Hoboken, NJ: Blackwell Publishing, 2008:17-80. [ Links ]
9. Talukdar R Complications of ERCP. Best Pract Res Clin Gastroenterol 2016;30(5):793-805. https://doi.org/10.1016/j.bpg.2016.10.007 [ Links ]
10. Ferreira AO, Cravo M. Sedation in gastrointestinal endoscopy: Where are we at in 2014? World J Gastrointest Endosc 2015;7(2):102-109. https://doi.org/10.4253/wjge.v7.i2.102 [ Links ]
11. Nayar M, Nicolson G, Gray H, Hodgson L. Experiences of the '1st Newcastle ERCP and EUS Course for Nurses. Gastrointest Nurs 2010;8(8):38-40. https://doi.org/10.12968/gasn.2010.8.8.79165 [ Links ]
12. Baron TH, Peterson BT, Mergrener K, et al. Quality indicators for endoscopic retrograde cholangiopancreatography. Am J Gastroenterol 2006;63(4 Suppl):S29-S34. https://doi.org/10.1016/j.gie.2006.02.019 [ Links ]
13. American Society for Gastrointestinal Endoscopy. Renewal of endoscopic privileges: Guidelines for clinical application. Gastrointest Endosc 1999;49(6):823-825. https://doi.org/10.1016/S0016-5107(99)70310-X [ Links ]
14. American Society for Gastrointestinal Endoscopy. Principles of training in gastrointestinal endoscopy Gastrointest Endosc 1999;49(6):845-853. https://doi.org/10.1016/S0016-5107(99)70316-0 [ Links ]
15. American Society for Gastrointestinal Endoscopy. Guidelines for credentialing and granting privileges for gastrointestinal endoscopy. Gastrointest Endosc 1998;48(6):679-682. https://doi.org/10.1016/S0016-5107(98)70059-8 [ Links ]
16. Morgan DE. Radiologic issues in ERCP. In: Baron TH, Korazek R, Carr-Locke DL, eds. ERCP. Philadelphia: Saunders Elsevier, 2008:19-30. [ Links ]
17. European Observatory on Health Systems and Policies and Smith PC. What is the scope for health system efficiency gains and how can they be achieved? Eurohealth 2012;18(3):3-7. https://apps.who.int/iris/handle/10665/333131 (accessed 23 October 2014). [ Links ]
 Correspondence:
Correspondence:
M Tun drmyinttun@outlook.com
Accepted 5 September 2022














