Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11b Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11b.16820
RESEARCH
Establishing high-tech surgical procedures in the Limpopo Academic Complex, Polokwane, South Africa
M Tun
MMed (Surg), FACS Department of General Surgery, Limpopo Academic Health Complex and School of Medicine, University of Limpopo, Polokwane, South Africa
ABSTRACT
BACKGROUND. The two hospitals comprising the Limpopo Academic Complex are the only referral institutions for Limpopo Province, which is the fifth most populated province of South Africa. The Department of General Surgery has a policy of establishing high-tech surgical procedures to improve patient care.
OBJECTIVES. To review the model of establishing high-tech surgical procedures in the Limpopo Academic Complex.
METHODS. The Department of General Surgery followed the DIRA model (D = Directive, I = Informative, R = Reconfiguration, A = Appraisal), which is dynamic and continuously evolving. The high-tech surgical procedures performed after a departmental workshop in January 2022, at which the DIRA model was conceptualised, are included in this survey.
RESULTS. There were 48 laparoscopic procedures performed during the period 23 February - 8 June 2022, and 13 interventional endoscopy procedures performed during the period 10 January - 31 May 2022, at Pietersburg Hospital, which is part of the Limpopo Academic Complex.
CONCLUSION. We strongly advocate use of the DIRA model, and believe that our experience may be useful to others seeking to establish high-tech surgical procedures in rural settings.
Limpopo Province, with 6.01 million inhabitants in 2021,[1] is the fifth most populated province of South Africa (SA). Health services in the province's public sector are delivered by 40 public hospitals, including two tertiary hospitals, Pietersburg Hospital and Mankweng Hospital, which comprise the Limpopo Academic Complex. These hospitals are the only referral institutions in the province for patients who need tertiary healthcare. Both provide the specialised services required.
Technological innovations are one of the main levers to improve the efficiency and quality of care at healthcare institutions. Slow adoption and utilisation of beneficial technology can result in an inefficient, poor-quality healthcare system. However, adoption of technological innovations before their efficiency has been proved may waste healthcare resources and harm patients.[2-5]
Our objective was to review the model of establishing high-tech surgical procedures in the Limpopo Academic Complex.
Methods
High-tech surgical procedures were established in the Limpopo Academic Complex following the DIRA model. The acronym DIRA stands for:
• Directive (D). Departmental policy with clear direction to adopt the high-tech surgical procedures.
• Informative (I). Providing necessary information on the adoption of the high-tech surgical procedures to all stakeholders, including administrators, policymakers, department staff, support staff, procurement staff, financial staff and healthcare industry representatives (Fig. 1).
• Reconfiguration of services (R). Implementing the model of subspecialty surgical units that provide subspecialty as well as general surgical services. All surgical units are encouraged to be involved in high-tech surgical procedures performed by colleagues with technical expertise. Recruiting persons with technical expertise is a part of re-figuration of existing services.
• Appraisal (A). Assessing the assimilated high-tech surgical procedures on a regular basis at daily morning department meetings and weekly mortality and morbidity meetings.

The high-tech surgical procedures performed in the Limpopo Academic Complex after a departmental workshop in January 2022, at which the DIRA model was conceptualised, are included in this survey. High-tech surgical procedures prior to that meeting are excluded.
Results
High-tech procedures in the Limpopo Academic Complex comprise three areas: vascular surgery, laparoscopic surgery and interventional endoscopy. We intend to report on high-tech vascular procedures in a future article on vascular surgery.
Forty-eight laparoscopic procedures, consisting of diagnostic laparoscopy (n=7 procedures), laparoscopic cholecystectomy (n=11), laparoscopic appendicectomy (n=9), laparoscopic splenectomy (n=1), laparoscopic hernia repair (n=14), laparoscopic diaphragm repair (n=1), laparoscopic adhesiolysis for intestinal obstruction (n=1), laparoscopic resection of the colon (n=1), laparoscopic Hartmann colostomy reversal (n=1), laparoscopic omental patch for perforated peptic ulcer (n=1) and laparoscopic wash-out for abdominal sepsis (n=1), were performed during the period 23 February - 8 June 2022 at Pietersburg Hospital in the Limpopo Academic Complex (Fig. 2).

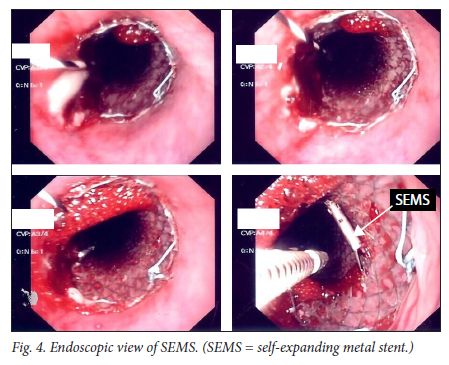
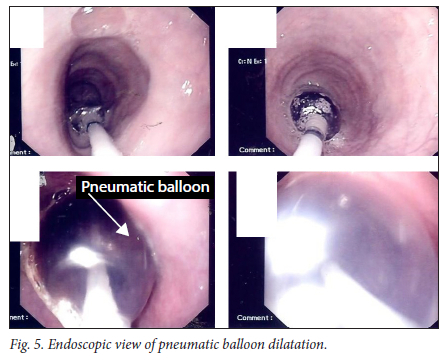
Thirteen interventional endoscopy procedures, consisting of therapeutic endoscopic retrograde cholangiopancreatography (n=9), insertion of a partially covered self-expanding metal stent for advanced oesophageal cancer (n=1) and pneumatic balloon dilatation for oesophageal stricture (n=3), were performed during the period 10 January - 31 May 2022 at Pietersburg Hospital (Figs 3 - 5).

Discussion
In the current medical literature, there is no shortage of high-level policy-focused commentaries relating to technology adoption in healthcare systems, and policymakers' attempts to improve the efficiency and quality of healthcare by encouraging technical innovations and accelerating their wider adoption. However, diffusion of these technical innovations within healthcare organisations is a huge, diverse and complex process. Even in the current literature, articles on the subject tend to lack clear and distinct recommendations and conclusions.[2,6] The Limpopo Academic Complex is not exempted from the complexity of these processes or from lack of clear direction.
Establishing high-tech surgical procedures in the Limpopo Academic Complex is directed by departmental policy. The present academic head, who is also chief of the province's surgical services, has clearly outlined the department's policy on adopting highcare technologies, including high-tech surgical procedures. This departmental policy has been the directive step towards establishing high-tech surgical procedures in the Limpopo Academic Complex. The numerous organisational factors contributing to the complexity of diffusion of technical innovations within a healthcare institution and determining whether it will be successful include the hospital culture, the influence of opinion leaders, the institution's readiness to accept innovations in technology, decision-making policy processes, and the power balance between supporters of and opponents to innovations in technology.[2,6] However, in the literature, three main preconditions have been recommended for healthcare organisations pursuing an efficient healthcare system. These are: (i) the provision of necessary information to all stakeholders; (ii) a system of government appropriate for relevant accountable parties; and (iii) sufficient will and capacity to pursue efficiency objectives.[7]
Spearheaded by the academic head, we provided the relevant information on high-tech surgical procedures to all stakeholders in the Limpopo Academic Complex as the 'informative step' in establishing these procedures. We felt that this was one way to overcome the complexity of the process of diffusion.
During this informative step, we conducted many departmental workshops and formal meetings with stakeholders, including management, administrators, the finance department, procurement, support staff, and health industry representatives. We met these stakeholders in informal ways and took opportunities to provide information on the essence of adopting high-tech surgical procedures. In our experience, such informal meetings and 'buddylike' communication are very productive in terms of providing the required information to all stakeholders.
Health practitioners play a major role as the key target for initiatives to improve efficiency in healthcare. They are responsible for the allocation of a large proportion of healthcare resources. It has been reported that there are immense variations in costs and uses of resources between healthcare providers, highlighting the importance of a 'reconfiguration of services' in which organisational weaknesses are identified and skills are transferred from efficient service providers.[7]
The reconfiguration of services in the Limpopo Academic Complex is an integral and crucial component in the process of establishing high-tech surgical procedures. The academic head chaired the department workshops and consultant meetings. A major item on the agenda has been to establish subspecialty units, which are vital for adopting technological innovations. Because the academic head was also chief of the province's surgical services, Limpopo's unique healthcare requirements were always on the meeting agenda. In view of SA's current healthcare challenges as well as the capacity of well-trained health practitioners,[8,9] headhunting and recruiting practitioners with technical expertise is one of the priorities in the reconfiguration of services. Recently, two vascular surgeons, two specialist surgeons with a special interest in surgical gastroenterology and two cardiothoracic surgeons have joined the Limpopo Academic Complex workforce.
During this reconfiguration stage, the Department of General Surgery in the Limpopo Academic Complex has established surgical subspecialty units with a unique set-up. Every surgical unit is encouraged to establish a centre of excellence in its field. However, every surgical unit is independent in terms of performing its own high-tech surgical procedures. The procedures take place with support from colleagues with the necessary technical expertise. In our experience, this process prevents monopolising of the high-tech procedures by only one unit and avoids academic rivalry among colleagues, creating a balance between establishment of centres of excellence and academic independence.
Mortality and morbidity (M&M) meetings are an integral part of current surgical practice. Traditionally, an M&M meeting is an educational conference at which the surgical management of a case and any resulting complications are discussed. However, the role of M&M meetings has evolved over time from a primarily educational process to an important guide to improve surgical practice. A well-conducted M&M meeting can be a platform for continuing professional development, applying clinical governance frameworks and improving health systems.[10-13]
M&M meetings are the essential component of the appraisal stage in establishing high-tech surgical procedures in the Limpopo Academic Complex. We conduct weekly M&M meetings, weekly academic meetings and daily morning hand-over meetings. Although these meetings are not conducted in the context of perfect, welldefined formats, we sincerely try to identify the factors that are crucial in making them effective, as outlined by Vreugdenburg et al.[10] in their article published in 2018. In our experience, daily hand-over meetings can be as effective a platform as M&M meetings, especially when they include feedback on high-tech surgical procedures performed in the department.
Conclusion
The establishment of high-tech surgical procedures in the Limpopo Academic Complex continues to be a dynamic and evolving process. We utilised the DIRA model (an integration of Directive, Informative, Reconfiguration and Appraisal components) to initiate, develop and grow these procedures. We strongly advocate utilisation of this model, with its limitations, to establish high-tech surgical procedures in more rural areas. We believe that our experience in this regard may contribute positively to endeavours to improve efficiency of healthcare systems, especially for medical institutions with limited resources.
Declaration. None.
Acknowledgements. We thank all staff of the Department of General Surgery, Limpopo Academic Complex, for their contributions to establishing high-tech surgical procedures. Without them, this article could not have been written. We also thank Mr C M Aung for his help in formatting the figures.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Statista. Total population of South Africa 2021, by province. 7 September 2022. https://www.statista.com/statistics/1112169/total-population-of-south-africa-by-province/ (accessed 10 September 2022). [ Links ].
2. Robert G, Greenhalgh T, Mac Farlane F, Peacock R. Adopting and assimilating new non-pharmaceutical technologies into health care: A systemic review. J Health Serv Res Policy 2010;15(4):243-250. https://doi.org/10.1258/jhsrp.2010.009137 [ Links ]
3. Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med 2009;360(15):1477-1449. https://doi.org/10.1056/NEJMp0901592 [ Links ]
4. Department of Health. High quality care for all: NHS next stage review final report. London: The Stationery Office, 2008. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_ data/file/228836/7432.pdf (accessed 13 September 2022). [ Links ]
5. Wilson CB. Adoption of new surgical technology. BMJ 2006;332(7533):112-113. https://doi.org/10.1136/bmj.332.7533.112 [ Links ]
6. Greenhalgh T, Robert G, Bate SP, Macfarlane F, Kyriakidou O. Diffusion of Innovations in Health Service Organizations. Oxford: Blackwell, 2005. [ Links ]
7. Smith PC. What is the scope for health system efficiency gains and how can they be achieved? Eurohealth 2012;18(3):3-6. https://apps.who.int/iris/handle/10665/333131 (accessed 13 September 2022). [ Links ]
8. Still L. South Africa at a glance: Health indicators. In: Still L, ed. Health Care in South Africa 2014. Johannesburg: Profile Media, 2014:65-70. [ Links ]
9. Benatar SR. The challenges of health disparities in South Africa. S Afr Med J 2013;103(3):154-155. https://doi.org/10.7196/SAMJ.6622 [ Links ]
10. Vreugdenburg TD, Forel D, Marlow N, et al. Morbidity and mortality meetings: Gold, silver or bronze? Aust N Z J Surg 2018;88(10):966-974. https://doi.org/10.1111/ans.14380 [ Links ]
11. Travaglia J, Debono D. Mortality and Morbidity Reviews: A Comprehensive Review of the Literature. Sydney: Centre for Clinical Governance Research in Health, 2009. [ Links ]
12. Singh HP, Durani P, Dias JJ. Enhanced morbidity and mortality meeting and patient safety education for specialty trainees. J Patient Saf 2019;15(1):37-48. https://doi.org/10.1097/PTS.0000000000000208 [ Links ]
13. Bal G, Sellier E, Tchouda SD, François P. Improving quality of care and patient safety through morbidity and mortality conferences. J Healthc Qual 2014;36(1):29-36. https://doi.org/10.1111/j.1945-1474.2011.00203.x [ Links ]
 Correspondence:
Correspondence:
M Tun
drmyinttun@outlook.com
Accepted 5 September 2022














