Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11b Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11b.16819
RESEARCH
An audit of emergency admissions to the adult general surgery department at Pietersburg Hospital, Polokwane, Limpopo Province, South Africa, during an 8-month period in 2021
R MavhunguI; A B (Sebastian) van AsII
IBSc (Med Sci); Department of General Surgery, Pietersburg Hospital, Limpopo Academic Health Complex, and School of Medicine, University of Limpopo, Polokwane, South Africa
IIMMed (Surg), PhD; Department of General Surgery, Pietersburg Hospital, Limpopo Academic Health Complex, and School of Medicine, University of Limpopo, Polokwane, South Africa
ABSTRACT
BACKGROUND. Emergency general surgery represents illnesses of very diverse pathology, related only by their urgent nature. The burden of general surgery emergency admissions at Pietersburg Hospital in Polokwane, Limpopo Province, South Africa, is currently unknown.
OBJECTIVES. To describe the demographic characteristics and clinical presentation of general surgical patients admitted to Pietersburg Hospital, as well as their surgical management, in order to plan future resource allocation.
METHODS. This was a retrospective descriptive audit of patients admitted to the adult general surgery department over the 8-month period April - November 2021.
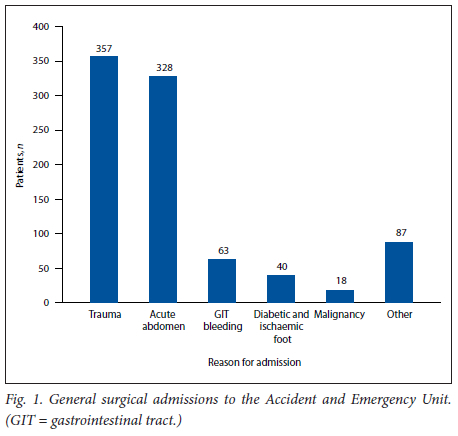
RESULTS. A total of 893 surgical emergency patients treated during the study period were included in the analysis. Of these, 357 were trauma and 536 non-trauma emergency cases. The majority of the patients (61%) were managed non-operatively. Of the 39% who required surgical management, only 24% had their operation performed within the first 24 hours, with the remainder only operated on after a delay owing to unavailability of space in theatre and/or unavailability of an intensive care unit (ICU) bed.
CONCLUSION. The lack of a dedicated surgical emergency theatre and the shortage of ICU beds are burning issues at Pietersburg Hospital and should be addressed as a matter of the greatest urgency.
Emergency general surgery represents illnesses of very diverse pathology, related only by their urgent nature.[1] Its burden is substantial, particularly in low- and middle-income countries where workforce, operational, organisational and financial challenges continue to have a negative impact on the rendering of timely, safe and affordable emergency surgery care.[2] In Limpopo Province, South Africa (SA), emergency surgical procedures often result in cancellation of elective surgery owing to the lack of an emergency operating theatre. The addition of emergency cases was found to have seriously interrupted 64.4% of the elective lists at Pietersburg Hospital.[3] Pietersburg Hospital is a teaching hospital for the University of Limpopo, located 30 km east of Polokwane, the provincial capital. The hospital shares referral responsibilities with Mankweng Hospital for regional and district hospitals in the province. There is as yet no dedicated trauma unit to deal with trauma cases at this hospital, so all trauma and other general surgical emergency cases are managed in the same unit by the same team. The Accident and Emergency Unit (AEU) at Pietersburg Hospital has 5 treatment rooms with 11 beds in total shared among all specialties in the hospital excluding obstetrics. In addition, the unit has 2 resuscitation rooms with a total of 6 beds. The unit admits an average of 20 patients per day. As a result of unavailability of beds, patients often stay in the AEU for more than 24 hours, partly because the COVID-19 pandemic has made it necessary to allocate surgical wards in the hospital to patients infected with the virus for purposes of infection control. Every day, an average of 7 patients from the previous day remain waiting in casualty for a hospital bed. The actual burden of general surgical emergency admissions to the AEU at Pietersburg Hospital is not known, so this study was designed to describe the demographic characteristics and clinical presentation of general surgical patients admitted to the AEU, as well as their surgical management. This information should guide the appropriate use and allocation of available resources. Accurate allocation will reduce unnecessary surgical delays, which are known to have a negative impact on patient outcome.
Methods
We conducted a retrospective descriptive audit of patients admitted to the adult general surgery department at Pietersburg Hospital over the 8-month period April - November 2021. The patient data were captured by the admitting doctor using a data collection tool. All adult patients reported to have been admitted the previous day were included in the study. We excluded all patients managed in and discharged from the AEU, and patients who died in the AEU. The senior consultant recorded the information using the same data collection tool during the daily weekday morning meeting. The data recorded included gender, age, presenting symptoms, provisional diagnosis, surgical intervention, and affected body site. In addition, if the surgical intervention required had not yet been performed, reasons for not performing the operation were recorded. The clinical diagnoses were further classified into trauma and non-trauma (medical emergency) cases. Trauma cases were subdivided according to the nature of the injury suffered. The collected data were captured using Microsoft Excel 2010 (Microsoft Corp., USA). The data were analysed using Stata software, version 16 (StataCorp., USA). Patient ages were grouped into categories. Categorical variables are expressed as proportions, and continuous variables as means and standard deviations.
Results
A total of 908 adult general surgical patients were entered into the Excel worksheet during the 8-month study period. Fifteen were removed from the list because of spoiled data collection tools, so 893 were included in the analysis. Reasons for admission of patients to the general surgery department via the AEU are presented in Fig. 1. The mean age of all the patients was 40 years, 71% were males, and trauma (40%) was the most common reason for presentation to the AEU and subsequent admission to the general surgery department. The majority of the non-trauma (medical emergency) patients presented with an acute abdomen (n=328), followed by upper gastrointestinal bleeding (n=63), diabetic and ischaemic foot (n=40), malignancies (n=18) and other conditions (n=87). When we analysed the data according to calendar month, the busiest month was October, with 67 trauma and 69 non-trauma emergency cases (Fig. 2). Motor vehicle accidents (n=82) were the most common trauma surgical emergency (Fig. 3). A large proportion (n=195/357; 55%) of trauma admissions to the AEU were related to interpersonal violence including stab wounds, assaults and gunshot wounds. Victims of mob assaults constituted 4% of the total trauma admissions. Patients injured in mob assaults were all males and typically sustained crush injuries. Suicide attempts (1.7%) and burn injuries (2.5%) contributed a relatively small number of reasons for admission (n=15). Of those who attempted suicide, 5 were males. Ingestion of car battery acid and self-inflicted grinder injuries were the mechanisms of self-harm in half of the suicide attempts. The majority of patients (47%) admitted to the general surgery department were young adults aged 18 - 35 years (Fig. 4). Nearly 60% of this age group were admitted for trauma. Although 39% (n=350) of the patients admitted needed emergency surgical intervention, only 24% had the operation performed on the day of admission. In the majority of cases (76%) the operation had to be delayed owing to unavailability of space in theatre (no dedicated surgical emergency theatre) and/or a shortage of ICU beds.
Discussion
We have described the spectrum of general surgical emergency admissions at a tertiary hospital in Limpopo Province, SA. Nearly three-quarters of patients admitted to the unit were males. Men living in rural areas are known to be self-reliant individuals and persons in positions of power and strength,[4] who may not want to be perceived as weak by seeking medical care when they are not feeling well. They may therefore delay seeking medical care until their condition worsens. Compared with females, men are also known to indulge more in risky behaviours such as drinking and driving late at night, exposing them to a greater risk of injury. Males constituted 62.4% of the workload in a non-trauma surgical emergency unit in Lagos State University Hospital.[5] A Chinese study reported a 89.68% male predominance among patients screened for alcohol-related trauma in Suzhou, China.[6]
Nearly 50% of the patients admitted to the AEU at our hospital during the study period were young adults aged 18 - 35 years, and nearly 60% of this age group were admitted for trauma (Fig. 4). We observed a decline in trauma-related emergencies with age, with patients progressively more likely to be admitted due to non-trauma (medical emergency) the older they were. The predominance of trauma surgical emergencies in our study may explain the young adult peak. The proportion of young adult (20 - 39 years) trauma admissions was also found to be high in the Princess Marina Hospital emergency department, Botswana.[7] We found that trauma constituted 40% of general surgical admissions during the study period.
Our facility has not yet been able to establish a dedicated trauma unit, so all trauma and non-trauma general surgical emergencies are managed in a single clinical emergency unit. The most common cause for admission in the young age group (18 - 35 years) in the present study was interpersonal violence-related injuries including stab wounds, injuries due to assault and gunshot wounds (n=195 out of 357 trauma admissions; 55% of all admissions due to trauma). In their study on interpersonal violence in SA, Bola et al.[8] found that 38% of trauma admissions were due to interpersonal violence. Interpersonal violence was responsible for 69.4% of trauma admissions in a study by Lewis and Wood[9] in KwaZulu-Natal. In our study, mob assaults were responsible for 4% of the trauma admissions. Mob assault is generally associated with extralegal justice ('kangaroo court') being meted out by community members. The victims are typically young adult males accused of robbing people of their belongings. In our study, all victims of mob assault were males aged between 23 and 41 years. Although the proportion (4%) was numerically small, it was clinically significant because all victims of mob assault presented to the AEU with the clinical features of crush syndrome. Of all interpersonal violence-related injuries, those sustained in mob assaults are associated with the highest proportion of fatalities. An analysis of mob justice fatalities in SA showed that 50.6% of the victims died on the scene, while 49.4% of those who were admitted to hospital died within 24 hours of admission.[10]
The majority of cases in the present study (60%) were non-trauma general surgical emergencies, of which acute abdomen (37% of total admissions) was the most common. This finding contrasts with a Nigerian study at a tertiary hospital, in which non-trauma surgical emergencies constituted 41.6% of the population studied.[11] In the present study, the majority of patients (61%) were managed non-operatively. Of the 39% who required surgical management, only 24% had their operation performed within the first 24 hours. The remaining patients were only operated on after a delay owing to unavailability of space in theatre and/or unavailability of an ICU bed. Lack of an emergency theatre is shown to be a problem that significantly reduces the effectiveness of the surgical department. This ineffectiveness comes at a huge price in terms of both financial cost and emotional trauma.[3]
Conclusion
Our 8-month audit of emergency cases demonstrates the large burden of trauma in our surgical department. We treated a total of 908 surgical emergency patients during this period. Of the 893 analysed, 357 were trauma cases and 536 non-trauma emergency cases. The most common mechanisms of injury were motor vehicle accidents (n=82), stab wounds (n=81), blunt assaults (n=67) and firearm-related injuries (n=47). Less common mechanisms of injury were suicide attempts (n=6), burns (n=9) and snakebites (n=5). The majority of the non-trauma (medical emergency) patients presented with signs and symptoms of acute abdomen (n=328), upper gastrointestinal bleeding (n=63), diabetic and ischaemic foot (n=40), malignancies (n=18) and other conditions (n=87). The striking epidemiological features of this audit are the high proportion of males (71%) compared with females, and the large number of patients in the young age group (18 - 35 years), which comprised 47% of all admissions. Another striking finding is the very high proportion of delayed surgical procedures due to the unavailability of a dedicated surgical emergency theatre and/or a shortage of ICU beds. We have repeatedly reported on the shortage of theatre availability;[3,1213] however, we are still waiting for the problem to be resolved.
References
1. Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS. The public health burden of emergency general surgery in the United States: A 10-year analysis of the nationwide inpatient sample 2001 - 2010. J Trauma Acute Care Surg 2014;77(2):202-208. https://doi.org/10.1097/TA.0000000000000362 [ Links ]
2. World Health Organization. WHO guidelines for safe surgery 2009: Safe surgery saves lives. Geneva: WHO, 2013. https://europepmc.org/article/MED/23762968 (accessed 20 September 2022). [ Links ]
3. Bhuiyan MMZU, Mavhungu R, Machowski A. Provision of an emergency theatre in tertiary hospitals is cost-effective: Audit and cost of cancelled planned elective general surgical operations at Pietersburg Hospital, Limpopo Province, South Africa. S Afr Med J 2017;107(3):239-242. https://doi.org/10.7196/SAMJ.2017v107i3.10687 [ Links ]
4. Beia T, Kielmann K, Diaconu K. Changing men or changing health systems? A scoping review of interventions, services and programmes targeting men's health in sub-Saharan Africa. Int J Equity Health 2021;20:87. https://doi.org/10.1186/s12939-021-01428-z [ Links ]
5. Ibrahim NA, Oludara Ma, Ajani A, et al. Non-trauma surgical emergencies in adults: Spectrum, challenges and outcome of care. Ann Med Surgery 2015;4(4):325-330. https://doi.org/10.1016/j.amsu.2015.09.004 [ Links ]
6. Junfang Q, Qi L, Long B, Fenf X, Du C. Characteristics of alcohol-related trauma: A retrospective analysis of 1997 cases. Research Square; 2020. https://doi.org/10.21203/rs.3.rs-37217/v1 [ Links ]
7. Bedada AG, Tarpley MJ, Tarpley JL. The characteristics and outcomes of trauma admissions to an adult general surgery ward in a tertiary teaching hospital. Afr J Emerg Med 2021;11:303-308. https://doi.org/10.1016/j.afjem.2021.04.002 [ Links ]
8. Bola S, Dash I, Naidoo M, Aldous C. Interpersonal violence: Quantifying the burden of injury in a South African trauma centre. Emerg Med J 2016;33(3):208 -212. https://doi.org/10.1136/emermed-2014-204160 [ Links ]
9. Lewis C, Wood D. Interpersonal violence as a major contributor towards the skewed burden of trauma in KwaZulu-Natal, South Africa. S Afr Med J 2015;105(10):827-830. https://doi.org/10.7196/SAMJnew.8380 [ Links ]
10. Medar S, Keyes CA, Stuart SJ. Mob justice fatalities in South Africa: A forensic mortuary study. Forensic Sci Med Pathol 2021;17(4):602-610. https://doi.org/10.1007/s12024-021-00415-8 [ Links ]
11. Onyemaechi NOC, Urube SU, Ekenze SO. Pattern of surgical emergencies in a Nigerian tertiary hospital. Afr Health Sci 2019;19(1):1786-1777. https://doi.org/10.4314/ahs.v19i1.53 [ Links ]
12. Mavhungu R, Jonas L, van As AB. Audit of surgical specialty patients and beds at Pietersburg Hospital, Limpopo Province, South Africa. S Afr Med J 2021;111(11b):1120-1124. https://doi.org/10.7196/SAMJ.2021.v111i11b.16124 [ Links ]
13. Ngwenya S, Mavhungu R, Mokwena MK, Robertson A, van As AB. Audit of surgical procedures in regional and central hospitals in Limpopo Province, South Africa. S Afr Med J 2021;111(11b):1126-1128. https://doi.org/10.7196/SAMJ.2021.v111i11b.16123 [ Links ]
 Correspondence:
Correspondence:
A B van As
sebastian.vanas@uct.ac.za
Accepted 5 September 2022














