Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.11 Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11.15825
RESEARCH
Discrepancies between clinical diagnoses and autopsy findings: A comparative study conducted in South Africa
D M JoubertI; S H RossouwII; C SolomonIII, IV; P W A MeyerV
IMB ChB; Department of Forensic Medicine, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
IIMB ChB; MMed (Med Forens); Department of Forensic Medicine, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
IIIMMed (Path); FC Path (SA) Anat; Department of Anatomical Pathology, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
IVMMed (Path); FC Path (SA) Anat; Department of Anatomical Pathology, National Health Laboratory Service, Pretoria, South Africa
VPhD (Medical Immunology); Department of Immunology, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
BACKGROUND: The anatomical pathology autopsy serves several purposes, notably as a quality management tool for evaluation of accuracy in clinical diagnosis. Despite its value, for various reasons there has been an international decline in autopsies conducted. In the modern medical era, with all its advances in technology, diagnostic techniques and interventions, there is still a high discrepancy between clinical diagnoses and postmortem findings
OBJECTIVES: To establish the discrepancies between clinical diagnoses and postmortem findings in anatomical pathology autopsies
METHODS: A retrospective, descriptive study was conducted over the 4-year-period 2014 - 2017. The clinical diagnoses and postmortem findings of cases referred to the Department of Anatomical Pathology at the University of Pretoria, South Africa, were evaluated and compared using the modified Goldman criteria
RESULTS: A total of 288 cases qualified for the study and were evaluated. The gender distribution was 155 (53.8%) male and 133 (48.2%) female, with the majority of cases in the age group 19 - 60 years (mean 36.4). The majority of the cases were referred by internal medicine, followed by paediatrics. The most common cause of death in major missed diagnoses was pulmonary conditions. Of the cases, 115 (39.3%) had a major discrepancy and 62 (21.5%) a minor discrepancy
CONCLUSION: This study showed that there is still a high discrepancy between clinical diagnoses and postmortem findings, similar to studies conducted globally. The current COVID-19 pandemic may be a driver for revival of the anatomical pathology autopsy, and future studies are recommended to evaluate whether the decline can be reversed
The autopsy has been pivotal in understanding the pathological basis of disease and in establishing the cause of death.[1] Over time, two settings for the autopsy developed.[2] The first of these is the academic/anatomical pathology autopsy, which is conducted to establish the nature and extent of underlying natural disease. In South Africa (SA), academic/anatomical pathology autopsies are conducted in terms of the National Health Act (Act 61 of 2003).[3] The second is the medicolegal autopsy, which is performed in terms of statutory provisions that mandate the examination of bodies of individuals who have died as a result of other than natural causes.[2] In SA, these autopsies are regulated in terms of the Inquests Act (Act 58 of 1959).[2]
Autopsies serve several purposes. Notably, they serve as a quality management tool to evaluate accuracy in clinical diagnoses, diagnostic imaging and other special investigations.[1,4,5] Although the autopsy and autopsy histology are being undermined, these modalities are ultimately the most accurate means of detecting clinicopathological discrepancies and are therefore considered the gold standard in determining the cause of death, as well as in the audit of clinical diagnoses, diagnostic tests and death certification.[6,7]
Other fields of quality assurance are evaluation of efficacy and potential adverse effects of new drugs, new surgical techniques and genetic engineering.[8] Furthermore, the autopsy is of great value for parents and siblings when genetic causes play a role in sudden and unexpected deaths and intervention can aid surviving family members.[8,9]
The autopsy assists us in understanding the pathogenesis of disease, facilitates the detection of new disease entities, and helps establish new patterns in known diseases.[1,8] Unexpected findings at autopsy contribute to the increasing pool of medical knowledge and improved clinical acumen, which may lead to better patient care.[10] The autopsy facilitates the investigation of occupational, environmental and lifestyle-related diseases and helps with the creation of accurate health policies.[1,8] It serves as a teaching tool for students by correlating pathology with clinical context, and also provides tissue for research purposes. To date, it remains unrivalled: no equivalent alternative exists.[1,9,11]
Despite the above, an international decline in autopsies has been observed over the past few decades, ascribed to various reasons.[1,5,10,12-16] These include major improvements in modern medicine's spectrum of diagnostic capabilities, attitudes of relatives, fear of litigation, financial implications, unmotivated pathologists, changes in the curricula of medical schools, and new approaches to autopsy procedures.[1,5,8-11,14-17]
In spite of advances in medical technology, diagnostic techniques and therapeutic interventions, there is still a high discrepancy between clinical diagnoses and postmortem findings, even in the modern medical era.[4-6,17] There has been hardly any improvement in the overall rate of discrepancies between the 1960s and the present.[13,17] A study performed in Brazil evaluated the discrepancies between clinical and autopsy diagnoses in patients who died in paediatric intensive care units, and it was concluded that a major clinicopathological discrepancy existed in 22.8% of cases and that 16.3% had unexpected autopsy findings that could have altered the outcome if these had been known before death.[8] In a similar study conducted at Toronto General Hospital in Ontario, Canada, from January to December 1999, the discrepancies between clinical and autopsy diagnoses were evaluated in patients who died in the hospital. A major missed diagnosis was identified in 40.7% of cases, and 29.6% had findings that could have altered the outcome if these had been known before death.[9] A study at Canberra Hospital in Australia evaluated deaths in the emergency department between January 1999 and June 2001. A major missed diagnosis was identified in 41% of cases, and 7% of cases had findings that could have altered the outcome.[4] A review article by Shojania et al.[16] documented discrepancies between clinical diagnoses and findings at autopsy. A study on a 53-autopsy series conducted in several countries, including the USA, the UK, Canada, Australia, Yugoslavia, India, Hong Kong, Switzerland, The Netherlands, Spain, Slovenia and Ireland, showed that the median major error rate was 23.5%.[16] Although numerous studies have been conducted abroad and in some hospitals in SA, there is a lack of published studies conducted in anatomical pathology departments in SA.
If this decline in academic autopsies continues, such procedures and the pathologists performing them will become obsolete, leaving the profession of clinical medicine blind to the many adverse consequences of clinical actions or omissions. However, by recognising that this decline is likely to have a negative impact on clinical medicine and by being proactive in reversing it, it may be possible to halt the extinction of this important tool.[11]
Advances in diagnostic technology have not diminished the value of the autopsy.[10] Its cost is reasonable, and it remains one of the most reliable ways (the gold standard, in fact) to validate clinical diagnoses.[6,7,10,11,17] It continues to provide information that is applicable to clinical management of patients and can potentially be life-saving. Medical management of the deceased patient should not be considered complete until a postmortem examination - the final consultation - has been performed.[9] To quote Atul Gawande (cited in Du Toit-Prinsloo and Saayman[2]): 'I want to think that my patient's condition is as predictable as the sun's rising, as the melting of an ice cube, and maybe I have to. But I have been around long enough to know that in human beings the simplest certainties can be dashed. Whether with living patients or cadavers, we do not know, until we look.'
Our objective was to establish the discrepancies between clinical diagnoses and postmortem findings in decedents presented to the Anatomical Pathology Department at the University of Pretoria over a 4-year period. Clinical diagnoses and postmortem findings were evaluated and compared using the modified Goldman criteria.[17]
Methods
Clearance to perform this research was obtained from the Research Ethics Committee of the Faculty of Health Sciences at the University of Pretoria (ref. no. 517/2020).
This was a retrospective, descriptive study of cases referred for autopsy and admitted to the Anatomical Pathology Department over a period of 4 years from 2014 to 2017. Data collected from the postmortem report included age, gender, body mass index, date of death, date of autopsy, department requesting the autopsy, autopsy findings and cause of death. Clinical diagnoses were obtained from the autopsy requisition report. The clinical diagnoses and postmortem findings were evaluated and compared by the primary author, using the modified Goldman criteria.[17] All decedents referred for autopsy and admitted to the Anatomical Pathology Department of the University of Pretoria over the 4-year time period were included. Excluded from the study were cases in which no clinical diagnosis was available at the time of referral (n=21) and all cases that were not finalised at the time of conducting the study (n=41).
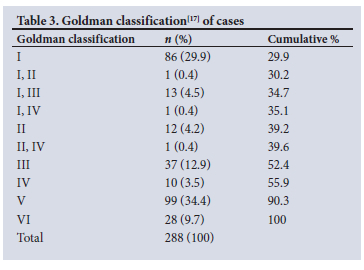
The Goldman criteria serves as a system for classifying errors in autopsy findings (Table 1). In brief, class I and class II are regarded as major discrepancies, whereas class III and class IV are regarded as minor discrepancies. Cases without discrepant diagnoses are designated class V, and non-classifiable cases are designated class VI.
Where multiple clinical diagnoses were suggested and any one of them was correct, it was accepted as such. No two major or two minor diagnoses per case were allocated, but a major and minor diagnosis could be allocated.
The postmortem findings were established in conjunction with an anatomical pathology registrar and consultant. The clinical diagnoses were made by the clinicians in the referring departments.
Descriptive statistics were compiled using one-way tabulation of variables in Stata 16.1 (StataCorp., USA).
Results
A total of 288 cases qualified for the study and were evaluated.
Demographic information
Of the study sample of 288 cases, 58 (20.1%) were aged <1 year, 15 (5.2%) were aged 1 - 11 years, 7 (2.4%) were aged 12 - 18 years, 145 (50.4%) were aged 19 - 60 years, and 63 (21.9%) were aged >60 years. The gender distribution was 155 (53.8%) male and 133 (48.2%) female. Most referrals (n=266; 92.4%) were from two state tertiary facilities and the remainder were from smaller state facilities and private hospitals.
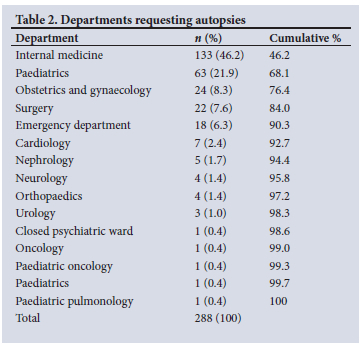
The postmortem interval (time from death to autopsy) ranged from 1 to 11 days, with an average of 2 - 3 days. The department that requested autopsies most often was internal medicine (n=133; 46.2%), followed by paediatrics (n=63; 21.9%) and obstetrics and gynaecology (n=24; 8.3%) (Table 2).
Medical information
Of the 288 cases, 16 (5.6%) had both a major and a minor discrepancy. The total discrepancies were 177 (61.4%), of which 115 (39.9%) were major and 62 (21%) minor. Of the major discrepancies, 101 (35.1% of the total of 288) were class I and 14 (4.9% of the total) were class II.
Of the minor discrepancies, 50 (17.4% of the total) were class III and 12 (4.2% of the total) were class IV. There were 99 cases of absolute agreement (34.4%), and in 28 cases (9.7%) a postmortem diagnosis could not be established with certainty (Table 3).
In the class I and class II categories, the lungs constituted the organ site where the most major diagnoses were missed. Causes of death included pulmonary parenchymal disease and infections, pulmonary thromboembolism, aspiration and tumours, as well as pulmonary haemorrhage and infarction. Pulmonary conditions were followed by cardiovascular causes for class I and cardiovascular and genitourinary causes and nonspecific infections for class II. Specific pathological entities comprising major missed diagnoses were 21 (18.3%) pulmonary infections, 10 (8.7%) nonspecific infections, 9 (7.8%) pulmonary thromboembolisms, 7 (6.1%) gastrointestinal necrosis/perforation, 3 (2.6%) ischaemic heart disease, 3 (2.6%) myocardial infarction, 3 (2.6%) rupture/leak of an abdominal aorta aneurysm, 2 (1.7%) pelvic inflammation and 2 (1.7%) septic abortion.
Discussion
In the modern medical era, with all its diagnostic and therapeutic advances, there is still a high discrepancy between clinical diagnoses and postmortem findings.[4-6,17] The autopsy has a principal role in serving as a quality management tool to evaluate accuracy in clinical diagnoses.[1,4,5] The present study showed a major discrepancy (class I and II) in 115 (39.9%) of cases presented to the Anatomical Pathology Department of the University of Pretoria. This finding is similar to the findings of the studies mentioned above, where major discrepancies were found in 22.8% of cases (study conducted in Brazil on paediatric deaths), 40.7% of cases (study conducted in Canada on hospital deaths), 41% of cases (study conducted in Australia on emergency department deaths) and 23% (a series of case studies conducted in multiple countries on hospital deaths).[4,8,9,16] Keeping in mind that the majority of cases in the present study were referred because of uncertainty in clinical diagnoses, there is a possible increased likelihood of a major discrepancy. The numbers reflect and confirm a high discrepancy between clinical diagnoses and postmortem findings and the need for continuous and increasing referral of cases for anatomical pathology autopsies, for auditing the accuracy of clinical findings.
Although most of the literature shows declining autopsy rates, an article published in December 2020 shows that the COVID-19 pandemic may be resulting in a promising revival of the autopsy.[19] At hospital morgues, pathologists were busily dissecting the disease's first victims, in an effort to understand this new disease entity better. Their results have shaped physicians' understanding of what COVID-19 does to the body and how they might combat it. At New Orleans University Medical Center, pathologists had performed ~50% more autopsies than they had done in recent years, and other hospitals in Alabama, California, Tennessee, New York and Virginia declared that they would also surpass their usual annual tally for the procedure.[19]
The present study had an age range from stillborn to 85 years, and the majority of cases (50.4%) were in the age group 19 - 60 years, with a mean age of 36.4 years. All ages of the population were therefore represented, although not equally.
The department requesting most of the autopsies was internal medicine, with 133 (46.2%) of the cases, followed by paediatrics with 63 cases (21.9%). The remaining 92 cases (31.9%) represent all the rest of the requesting departments, indicating a lack of true understanding of the value of academic autopsies in those departments.
The most common cause of death in major missed diagnoses was pulmonary conditions, with pulmonary infections and thromboembolism topping the list, partly reflecting internal medicine as the major referral department.
The results of this study may be limited by various factors. Only cases in which there was an uncertainty in clinical diagnosis were referred for autopsy, increasing the likelihood of a major discrepancy. Hospital files were not available for perusal prior to conducting the autopsy, only the autopsy requisition form containing a limited history and possible diagnoses, thereby limiting the amount of data that can be incorporated into the study. Length of stay in hospital, for example, could influence a discrepant/congruent diagnosis. Internal medicine was the department that referred the majority of cases, influencing the most common cause of death in major missed diagnoses. The fact that not all ages were represented equally could influence the most common cause of death, as patients in different age groups die from different illnesses. The number of cases that did not qualify for the study (total n=62) is large and may have affected not only the percentage of missed diagnoses, but also the causes of death in major missed diagnoses.
Conclusion
There is still a high discrepancy between clinical diagnoses and postmortem findings, despite advances in diagnostic and therapeutic interventions.[4-6,17] It has been highlighted by the results of the present study, focused on a population of anatomical pathology cases referred for autopsy in the setting of uncertain clinical findings. The need exists for a revival of anatomical pathology autopsies, and the current COVID-19 pandemic might just be the driver thereof.[19]
Declaration. The research for this study was done in partial fulfilment of the requirements for DMJ's MMed (Path) (Forens) degree at the University of Pretoria.
Acknowledgements. The authors thank Ms Barbara van Deventer for assistance.
Author contributions. DMJ: primary researcher, design, manuscript preparation, editing, administration and interpretation; SHR: study supervisor, editing; CS: study co-supervisor, editing; PWAM: statistical assistance.
Funding. None.
Conflicts of interest. None.
References
1. Van den Tweel JG, Wittekind C. The medical autopsy as quality assurance tool in clinical medicine: Dreams and realities. Virchows Arch 2016;468(1):75-81. https://doi.org/10.1007/s00428-015-1833-5 [ Links ]
2. Du Toit-Prinsloo L, Saayman G. Performance of autopsies in South Africa: Selected legal and ethical perspectives. CME 2012;30(2):53-55. [ Links ]
3. South Africa. National Health Act No. 61 of 2003. https://www.gov.za/sites/default/files/gcis_document/201409/a61-03.pdf (accessed 12 October 2020). [ Links ]
4. O'Connor AE, Parry JT, Richardson DB, Jain S, Herdson PB. A comparison of the antemortem clinical diagnosis and autopsy findings for patients who die in the emergency department. Acad Emerg Med 2002;9(9):957-959. https://doi.org/10.1197/aemj.9.9.957 [ Links ]
5. Tavora F, Crowder CD, Sun C, Burke AP. Discrepancies between clinical and autopsy diagnoses: A comparison of university, community, and private autopsy practices. Am J Clin Pathol 2008;129(1):102-109. https://doi.org/10.1309/9M7DFE62RTDKHH4D [ Links ]
6. Carlotti AP, Bachette LG, Carmona F, Manso PH, Vicente WV, Ramalho FS. Discrepancies between clinical diagnoses and autopsy findings in critically ill children: A prospective study. Am J Clin Pathol 2016;146(6):701-708. https://doi.org/10.1093/ajcp/aqw187 [ Links ]
7. Bernardi F, Saldiva P, Mauad T. Histological examination has a major impact on macroscopic necropsy diagnoses. J Clin Pathol 2005;58(12):1261-1264. https://doi.org/10.1136/jcp.2005.027953 [ Links ]
8. Fernando L. Place of autopsy in quality assurance of curative service. Galle Med J 2008;13:51-54. https://doi.org/10.4038/gmj.v13i1.897 [ Links ]
9. Aljerian K. The final consultation: The autopsy. J Forensic Leg Investig Sci 2017;3(1):018. https://doi.org/10.24966/flis-733x/100018 [ Links ]
10. Tai DY, El-Bilbeisi H, Tewari S, Mascha EJ, Wiedemann HP, Arroliga AC. A study of consecutive autopsies in a medical ICU: A comparison of clinical cause of death and autopsy diagnosis. Chest 2001;119(2):530-536. https://doi.org/10.1378/chest.119.2.530 [ Links ]
11. Ayoub T, Chow J. The conventional autopsy in modern medicine. J R Soc Med 2008;101(4):177-181. https://doi.org/10.1258/jrsm.2008.070479 [ Links ]
12. Turnbull A, Osborn M, Nicholas N. Hospital autopsy: Endangered or extinct? J Clin Pathol 2015;68(8):601-604. https://doi.org/10.1136/jclinpath-2014-202700 [ Links ]
13. Roulson J, Benbow E, Hasleton PS. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology: A meta-analysis and review. Histopathology 2005;47(6):551-559. https://doi.org/10.1111/j.1365-2559.2005.02243.x [ Links ]
14. Venter N, du Plessis N, Cloete A, Joubert F, Goedhals J. Autopsies performed at Universitas Academic Hospital, South Africa, 1990 - 2010, and perceptions and opinions of health professionals on the importance of autopsies in modern medicine. S Afr J Infect Dis 2015;30(2):2849-2856. https://doi.org/10.1080/23120053.2015.1054178 [ Links ]
15. Hamza A. Declining rate of autopsies: Implications for anatomic pathology residents. Autops Case Rep 2017;7(4):1-2. https://doi.org/10.4322/acr.2017.036 [ Links ]
16. Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: A systematic review. JAMA 2003;289(21):2849-2856. https://doi.org/10.1001/jama.289.21.2849 [ Links ]
17. Wittschieber D, Klauschen F, Kimmritz A, et al. Who is at risk for diagnostic discrepancies? Comparison of pre- and postmortal diagnoses in 1800 patients of 3 medical decades in East and West Berlin. PLoS ONE 2012;7(5):e37460. https://doi.org/10.1371/journal.pone.0037460 [ Links ]
18. Goldman L, Sayson R, Robbins S, Cohn LH, Bettmann M, Weisberg M. The value of the autopsy in three medical eras. N Engl J Med 1983;308(17):1000-1005. https://doi.org/10.1056/nejm198304283081704 [ Links ]
19. Renault M. The autopsy, a fading practice, revealed secrets of COVID-19. Associated Press, 28 December 2020. https://www.medscape.com/viewarticle/943245#vp_1 (accessed 15 February 2021). [ Links ]
 Correspondence:
Correspondence:
D M Joubert
doretmjoubert@lantic.net
Accepted 31 August 2022














