Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 n.11 Pretoria Nov. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i11.16452
RESEARCH
The unmet need for critical care at a quaternary paediatric intensive care unit in South Africa
E ClarenceI, II; P M JeenaIII, IV
IMB ChB, FC Paed (SA); Department of Paediatrics, Inkosi Albert Luthuli Central Hospital, Durban, South Africa
IIMB ChB, FC Paed (SA); Department of Paediatrics and Child Health, University of KwaZulu-Natal, Durban, South Africa
IIIMB ChB, PhD Department of Paediatrics, Inkosi Albert Luthuli Central Hospital, Durban, South Africa
IVMB ChB, PhD Department of Paediatrics and Child Health, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Paediatric intensive care, a valuable resource that improves the outcomes of critically ill children, is often scarce
OBJECTIVE: To evaluate the need for paediatric intensive care beds and compare the outcomes of admitted and non-admitted deserving cases
METHODS: A prospective evaluation of all bed requests, in terms of need for intensive care and outcomes of those admitted and not admitted to a paediatric intensive care unit (PICU), was performed between July 2017 and June 2018. Factors for refusal and for poor outcomes were evaluated
RESULTS: Of the 811 bed requests, 32.6% (n=264, p<0.001) were denied access. Of the 231 deserving cases who were denied access, 85.7% (n=198) were due to unavailability of a PICU bed. Patients not admitted to PICU had a twofold increased risk of dying compared with those admitted (34.4% v. 15.5% respectively, p<0.001), even though the patient characteristics of both groups were similar (age, gender and nutritional status). In those admitted, risk factors for mortality were requiring transfusion of blood and platelets (56.0%, p<0.001), requiring two or more inotropes (52.5%, p<0.001), instability on admission (41.3%, p<0.001), prior cardiac arrest (32.0%, p=0.021), severe acute malnutrition (26.9%, p=0.043), fungal infection (22.2%, p=0.004) and emergency admission (18.0%, p<0.001). In those not admitted, prior cardiac arrest (100%, p<0.001) and emergency referral (42.3%, p<0.001) were associated with adverse outcomes
CONCLUSION: The need for PICU beds exceeds availability, with a consequent twofold increase in mortality among cases not admitted to PICU. Paediatric critical care services have increased at appropriate sites of need following completion of this study
Intensive care is an expensive resource worldwide,[1,2] with the need for paediatric critical care increasing.[3] There is a marked disparity in the availability of paediatric critical care beds between low-income and high-income countries (e.g. 0.3 beds per 100 000 children in Ghana[4] and 8 beds per 100 000 children in the USA[5]). Low- and middle-income countries carry a disproportionately high burden of cases that require intensive care,'31 yet healthcare professionals here have significantly fewer resources than their industrialised counterparts. The child mortality rate in South Africa (SA) is on a downward trend, from 78.1 per 1 000 live births in 2003 to 40.5 in 2015.[6] The country is still lagging behind other upper-middle-income countries such as Brazil and Mexico, where child mortality rates were recorded as 16 and 13 per 1 000 live births, respectively, in 2015.[7] Shortages of intensive care services were noted to be the most frequent modifiable factors in the 2nd Triennial Report of the Committee on Morbidity and Mortality in Children under 5 years.[8] It was the third-most common avoidable administrative factor in the latest Saving Babies report,[9] and an avoidable factor in 15.1% of deaths in patients aged <18 years in the most recent Saving Children report.[10] The scarcity of paediatric intensive care services has an adverse effect on outcomes of children of all ages.
KwaZulu-Natal Province (KZN) has the largest provincial paediatric population in SA, with 3 420 000 children <15 years old.[11] There have been no studies specifically evaluating paediatric intensive care resources across the country, but a national audit of all (adult, paediatric and neonatal) critical care (intensive care and high care) services published in 2007 revealed a bed/population ratio in the KZN public healthcare sector of 3.1 per 100 000 population.[12] Of all the critical care beds in KZN, 9.5% were in dedicated paediatric units, 4.8% were in mixed paediatric/neonatal units and 28.6% were in mixed medical/surgical paediatric/neonatal units.[12] At the time of our study, there were 25 paediatric intensive care beds in KZN, which equated to 0.73 beds per 100 000 children.
SA data that evaluate the need for paediatric intensive care, and outcomes of patients denied and provided access to a paediatric intensive care unit (PICU), are scarce. The identification of factors influencing outcomes of patients admitted to PICU to guide effective triaging of patients is essential.[1,2,13] A review of SA paediatric emergency and intensive care resources focusing on infrastructure, hospital characteristics, staffing (physicians and nurses) and availability of equipment, drugs and laboratory services, similar to other multi-country surveys conducted in resource-limited settings, is necessary.[14,15] In planning for the expansion of paediatric intensive care services in KZN, we provide local data on the unmet need at the province's largest PICU. We evaluated reasons for denial of PICU access and compared the outcomes of patients who were admitted and not admitted to PICU, and evaluated factors affecting these outcomes.
Methods
Study setting
The KZN Department of Health (DoH) divides the province into three geographical health areas; each consists of three to five municipal districts, viz. Area One (eThekwini, iLembe, Ugu), Area Two (Amajuba, Harry Gwala, uMgungundlovu, uMzinyathi, uThukela) and Area Three (King Cetshwayo, uMkhanyakude, Zululand). A total of 41.7% (n=1 426 000) of children in KZN live in Area One, 32.0% (n=1 095 000) in Area Two and 26.3% (n=898 000) in Area Three.[8] There were 25 PICU beds in the public healthcare sector of KZN, viz. 14 beds at Inkosi Albert Luthuli Central Hospital (IALCH) in the eThekwini district (Area One); 7 beds at 2 hospitals in the uMgungundlovu district (Area Two); and 4 beds at 1 hospital in the King Cetshwayo district (Area Three). To maximise utilisation of PICU facilities, doctors would first contact the PICUs in their area and thereafter PICUs in other areas as they attempted to secure access for patients requiring this service. Furthermore, the provincial DoH has created the capacity at each secondary and tertiary level hospital to ventilate a critically ill patient for an interim period of 24 - 48 hours, with the aim of stabilisation prior to transfer to a commissioned PICU facility.
The PICU at IALCH is a multipurpose 'closed unit' that admits emergency and elective, medical and surgical patients, and is the only PICU in the province to offer quaternary level care. Elective admissions include cardiothoracic surgery, neurosurgery, otorhinolaryngology (ENT), paediatric general surgery and plastic surgery patients. Although the hospital has other ICUs that admit children, these services are all mixed units for adults and children. The cardiothoracic surgical ICU has two paediatric beds available for elective admissions following cardiopulmonary bypass. The trauma ICU may admit children >2 years of age with trauma or burns, but it does not have beds reserved for paediatric patients. If there is no available bed in the PICU, the neurosurgical ICU and the general adult ICU may admit selected paediatric emergency cases on an ad hoc basis. The neonatal ICU, with 12 ICU and 8 high care beds, regularly has a long waiting list. A separate 21-bed paediatric high care unit utilised for stepping-down of PICU 'graduates' and for managing high-risk patients assessed as not immediately requiring intensive care provides renal replacement therapy and non-invasive respiratory support, such as continuous positive airway pressure and high-flow humidified nasal oxygen.
Study design
We performed a prospective, descriptive evaluation of all bed requests between 1 July 2017 (when ethical approval was granted) and 30 June 2018, at the IALCH PICU, Durban, SA.
Participants
All PICU bed requests were by formal telephonic referral, with a detailed patient-structured questionnaire completed for each bed request, including characteristics, referring hospital, primary discipline (medical or surgical) and clinical condition (appendix 1 https://www.samedical.org/file/1928). The consultant on duty reviewed all requests and decided on acceptance or denial of access. Requests were collated to create an anonymous database. Outcomes of admitted patients were documented prospectively from the electronic PICU records, while outcomes of the patients not admitted were evaluated via telephonic follow-up with the referring clinician. There were no exclusion criteria. Patients admitted on 30 June 2018 were followed up until discharge or death during the hospital admission.
If a patient's clinical condition altered significantly enough to warrant a second discussion with PICU and the decision regarding acceptance was different (e.g. from refused to accepted), each discussion was counted as a separate request.
Data collected for all patients were date of admission to hospital and date of PICU bed request, name and municipal district of referring hospital, age, gender, HIV status, nutritional status, primary discipline, organ system involvement, presence of comorbidities, admission characteristics (emergency, elective, postoperative, readmission) and outcome.
Additional data collected for patients admitted to PICU were date of admission and discharge, stability and mode of ventilation on arrival, modalities of medical and surgical care provided during admission (mode of ventilation, inotropes, renal replacement therapy, blood products, surgeries) and positive microbiological cultures (site, organism, and sensitivity).
Bacterial and fungal infections were confirmed on microbiological culture, and viral infections were confirmed on either serological investigations or viral polymerase chain reaction.
Reasons for accepted patients not arriving in the PICU and reasons why patients were denied access were documented on the telephonic referral forms. Patients with missing data were included in the study for a comprehensive evaluation. We excluded patients from the outcome analyses if their outcomes were unknown.
Definitions
A secondary or regional hospital provides the second level of hospital healthcare. These hospitals receive referrals from and provide specialist paediatric support to several district hospitals (the first level of hospital healthcare).[16]
A tertiary or provincial hospital provides the third level of hospital healthcare. These hospitals receive referrals from and provide subspecialist support to several regional hospitals, including intensive care services.[16] At the time of the study, two tertiary hospitals in the province were able to provide high-frequency oscillatory ventilation (HFOV), and only one tertiary hospital was able to provide peritoneal dialysis. There were no tertiary hospitals with the capacity to offer haemodialysis, nor any staffed by paediatric anaesthesiologists.
A quaternary or central hospital provides the fourth and highest level of hospital healthcare.[16] These institutions provide intensive care services with advanced capabilities (such as HFOV, use of nitric oxide), haemodialysis, advanced neurological and cardiac monitoring, and the provision of paediatric anaesthesia. IALCH, a central hospital, provides highly specialised multispecialty clinical services including cardiothoracic surgery, neurosurgery, ophthalmological and otorhinolaryngological surgery, paediatric cardiology, paediatric endocrinology, paediatric gastroenterology, paediatric nephrology, paediatric neurology, paediatric pulmonology and plastic surgery.
We defined a delay in admission as >24 hours from the time of patient acceptance to the time of admission. A longer cut-off than the conventional 3 - 6 hours was used, as it is commonplace for long delays to occur owing to an inadequately resourced ambulance service in the province.
In HIV-positive patients, the HIV viral load was reviewed (recorded as virological failure if >400 copies/mL), and it was noted if the diagnosis of HIV was made during the PICU admission.
We assessed nutritional status according to the World Health Organization classification.[17] Low birthweight included all birthweights <2 500 g.
We defined readmission as a repeat admission to the PICU after discharge, during the study period. If a patient required more than one PICU admission during a single hospital stay, we counted each admission separately.
We defined patients as unstable on arrival if they required a change of endotracheal tube, increased ventilation, fluid resuscitation or new/further inotropic support on admission.
Data analysis
We created the database in Excel (Microsoft Corp., USA). It was subsequently analysed within a quantitative framework making use of R version 3.6.3, (R Core Team, USA). The results were presented in the form of descriptive and inferential statistics. Categorical variables were described as counts and percentage frequencies. Associations between the categorical variables were assessed using x2 tests, and when the distribution of the cross-tabulations contained an expected value of <5, a Fisher's exact test was applied. A p-value <0.05 was considered statistically significant.
Ethics approval
For patients admitted to the IALCH PICU, informed consent was obtained from the caregiver once the patient had been stabilised, with every attempt made to minimise any undue psychological distress. As no patient identifiers were recorded and no study-related interventions were undertaken, permission to collect data of patients not admitted to the IALCH PICU was obtained prospectively from the district manager, medical manager and head of paediatrics at all referring hospitals. Approval from the University of KZN (UKZN) Biomedical Research Ethics Committee (ref. no. BE051/17), the KZN DoH (NHRD ref. no. KZ_2016RP27_49) and the hospital management of IALCH was obtained.
Results
The need for PICU services
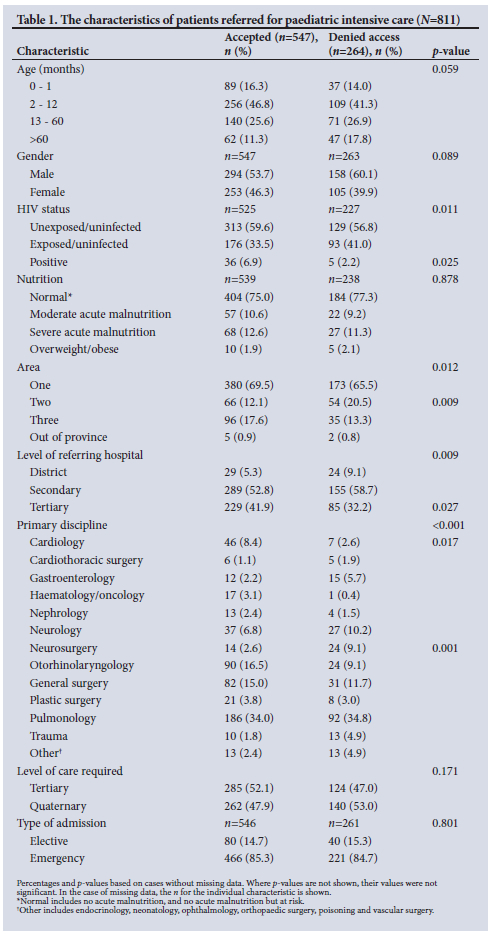
Of the 811 bed requests, 67.4% (n=547) were accepted to PICU and 32.6% (n=264) of patients denied access to PICU. The characteristics of the patients are shown in Table 1. When triaging patients for admission, there was no bias based on age, gender or nutritional status.
Of the 547 accepted patients, 9.9% (n=54) were not admitted, viz. 35.2% (n=19) died prior to arrival, 31.5% (n=17) improved and no longer required PICU, 22.2% (n=12) were admitted to high care, 7.4% (n=4) were admitted to another ICU and the outcome was unknown in 3.7% (n=2) of patients.
Of the 264 patients who were denied access, 56.1% (n=148) remained at the referring hospital, 22.7% (n=60) were admitted to another ICU, 12.9% (n=34) were admitted to a paediatric high care, 5.3% (n=14) were admitted to a paediatric ward and 3.0% (n=8) had unknown outcomes. In 12.5% (n=33) of the cases denied access, the patient's condition did not warrant PICU admission. Reasons for denying access to the remaining deserving cases (n=231) included no PICU beds (all beds in the unit were occupied) in 85.7% (n=198), that the patient was a poor candidate for PICU (unlikely to survive illness without significant morbidity regardless of whether they received intensive care or not) in 5.6% (n=13) and in 8.7% (n=20) of cases, the patient was either too unstable for transfer, the PICU had insufficient nursing staff (a physical bed was available but there was no nurse to care for the patient) or the bed request was cancelled.
Of the 13 patients who were denied access on the grounds of being poor candidates, 30.8% (n=4) survived, 61.5% (n=8) died and 7.7% (n=1) had unknown outcomes. It is unknown whether the patients who survived suffered any significant morbidity following their illness.
The need for PICU beds was 23.7 per 100 000 children (compared with an availability of just 0.73). The need was highest from Area One (38.8), and lower from Areas Two (11.0) and Three (14.6), where tertiary-level PICU facilities were available. Tertiary-level care was sought in 55.7% (n=308/553) of Area One, 47.5% (n=57/120) of Area Two and 32.8% (n=43/131) of Area Three referrals.
The outcomes of critically ill patients referred for paediatric intensive care
Of the 811 bed requests, 4.1% (n=33) were assessed as not warranting PICU admission. Of these 33 patients, 90.9% (n=30) survived and 9.1% (n=3) died. Of these, 21.2% (n=7) were admitted to other ICUs and 78.8% (n=26) were not admitted to any ICU. We excluded patients not warranting PICU admission from the outcome analyses. Of the 778 bed requests deserving of PICU, 70.7% (n=550) were admitted to a PICU (493 at the IALCH PICU and 57 at other ICUs).
Two admissions to the IALCH PICU had unknown outcomes and were excluded from the analyses.
Of the 491 patients admitted to the IALCH PICU, 15.9% (n=78) were 0 - 1 months of age, 47.0% (n=231) 2 - 12 months, 25.7% (n=126) 13 - 60 months and 11.4% (n=56) >60 months. There was a slight predominance of males (54.6%, n=268); 6.9% (n=33) were HIV positive; 34.9% (n=166) were HIV exposed but uninfected; and 12.9% (n=63) had severe acute malnutrition (SAM). The overall mortality rate was 15.7% (n=77).
The median length of stay in the IALCH PICU was 7 (interquartile range 4 - 14) days in patients who survived and 8 (interquartile range 3 - 17) days in patients who died.
Fifty-seven patients were admitted to other ICUs. Their ages were 10.5% (n=6) 0 - 1 month of age, 49.1% (n=28) 2 - 12 months, 28.1% (n=16) 13 - 60 months and 12.3% (n=7) >60 months. A total of 70.2% (n=40) were male, 2.2% (n=1) were HIV-positive, 40.0% (n=18) were HIV-exposed but uninfected,and 7.7% (n=4) had SAM. The overall mortality rate was 14.0% (n=8).
As the characteristics and outcomes of the patients admitted to the IALCH PICU and the patients admitted to other ICUs were similar (appendix 2: https://www.samedical.org/file/1929), we pooled the data to create 548 PICU admissions, with a mortality rate of 15.5%.
Of the 228 patients who were not admitted to PICU, 75.0% (n=171) remained in the emergency area at the referring hospital, where 42.1% (n=72) died; 14.9% (n=34) were admitted to the paediatric high care at IALCH, where 8.8% (n=3) died; and 5.7% (n=13) were admitted to a paediatric ward at IALCH and survived. We excluded 10 patients where the outcomes were unknown.
Patients not admitted to PICU had a twofold increased risk of dying compared with those admitted (34.4% v. 15.5% respectively, p<0.001) even though both groups had similar referral characteristics.
The characteristics influencing outcomes in critically ill patients
A comparison of the relative risk for mortality according to different characteristics of pooled patients admitted and not admitted to any PICU is shown in Table 2. Mortality rates were high in patients who were not admitted if they had a history of any of the following: preterm delivery 36.0% (p<0001), low birthweight 50.0% (p=0.001) or prior cardiac arrest 100% (p<0.001).
The factors affecting outcomes of patients admitted to PICU
The factors influencing the outcomes of patients admitted to the IALCH PICU are shown in Table 3.

Discussion
During this study, the provincial need for PICU beds at IALCH (23.7 per 100 000 children) exceeded availability (0.73); 32.6% of all bed requests were denied access to PICU, the majority due to insufficient beds. As the only PICU in Area One, it was not unexpected that the greatest need was from the same area. Despite the IALCH PICU being a quaternary-level service, half the bed requests sought tertiary-level care. These data show that there is an unmet need for tertiary-level paediatric intensive care beds in Area One of KZN. The high numbers of tertiary-level patients requiring critical care at quaternary services impacts negatively on the ability of quaternary services to deliver on their mandate. Pulmonology, otorhinolaryngology and paediatric general surgery were the disciplines with the greatest need for more tertiary-level intensive care services. In 2012 - 2013, 47.6% of SA paediatric deaths were due to infection or parasitic disease, and 26.9% to illnesses of the respiratory system. This aligns with the high numbers of critically ill children with respiratory disease requiring PICU.[10] In keeping with recommendations of previous studies,[18] patients with HIV or malnutrition were not excluded from admission, despite this being a common misconception.
The mortality rate of critically ill patients not admitted to PICU (34.4%) was more than double that of patients admitted to PICU (15.5%) (p<0.001). This confirms the adverse effect that lack of paediatric intensive care services has on patient outcomes. The mortality rate of patients admitted to PICU in our study was 15.5%, compared with a rate of 15.6% reported by another PICU in KZN in 2016.[19] This is related to the frequent use of quaternary services for emergency tertiary-level care. In 2021, a multisite SA study reported a mortality rate of 9.6%. This difference may be due to patients <30 days old, premature infants, children who died within 2 hours of admission and children transferred to other PICUs being excluded from that cohort.[20] There have been no other SA studies that reviewed the outcomes of critically ill patients denied access to PICU. Of critically ill patients who were accepted to PICU, 3.4% were not admitted because they died prior to arrival. The latest Saving Children report[10] notes many factors affecting paediatric mortality that can be addressed at home (in 34.4% of patients), in the clinic or outpatient department (10.2%), in the admission or emergency care area (22.9%), in the ward at the referring facility (28.3%) or in transit (4.2%).
The difference in mortality rates in patients admitted to PICU compared with those not admitted was significant regardless of age, gender or level of care required. There was a significant impact on outcomes in those who were HIV-negative (p<0.001), were HIV-exposed uninfected (p<0.001), of normal nutrition (p<0.001), had moderate acute malnutrition (MAM) (p=0.001) and whose primary needs were neurology (p<0.001) or pulmonology (p<0.001). A prior cardiac arrest had a mortality rate of 100% (p<0.001) if not admitted to PICU, and remained high even with PICU admission. The difference in mortality rates was significant if the patient was referred from a district hospital (p<0.001), which can be explained by the comparative lack of resources available at these hospitals. Similarly, the mortality rates in patients not admitted to PICU were higher in patients referred from secondary (p<0.001) hospitals compared with those referred from tertiary hospitals. This may be due to the level of supportive care provided by paediatricians in the emergency resuscitation rooms and wards of tertiary hospitals. Surprisingly, patients referred from tertiary hospitals had similar mortality rates regardless of their PICU admission status, which may be related to the severity of illness at presentation. Transfer of patients who were more ill, and possibly unstable, would have transferred the mortality to the PICU. There was no statistically significant difference in mortality if patients were HIVpositive (p=0.740) or had SAM (p=0.830).
Of the patients denied access because they did not warrant PICU admission, 9.1% died. This highlights the fact that our assessment per telephone may be suboptimal and is dependent on the clinical assessment of a medical officer or registrar. Of the patients denied access because they were unlikely to survive without major morbidity, 30.8% survived. Of the patients who were accepted but not admitted to PICU, 35.2% died and 31.5% survived. These data show that outcomes are not always predictive during the process of triage.
The mortality rate of HIV-positive patients admitted to PICU was 32.4% (p=0.084), compared with a range of 18.4% - 25.0% reported in previous SA studies.[19,21,22] This is similar to findings from a Mozambican study where neither HIV exposure nor infection had a statistically significant association with mortality in PICU.[23] Despite the success of the elimination of mother-to-child transmission programme and higher rates of paediatric HIV-positive patients on antiretroviral therapy, the PICU mortality rate in HIV-positive patients doubled if the patient was not virologically suppressed (61.5% v. 25.0%, p=0.013), and also increased if newly diagnosed (23.5%, p=0.169).
The mortality rate in malnourished children was lower than in a previous study from KZN that showed mortality rates of 40.0% - 46.7%. [19]Notably, this study was undertaken >6 years earlier, and there has been a concerted effort on behalf of the DoH to train healthcare workers on the integrated management of acute malnutrition during recent years. A study in India found an overall mortality rate of 38.8% in malnourished patients admitted to PICU, with increasing odds of mortality, ventilation, prolonged PICU stay and duration of mechanical ventilation with greater severity of malnutrition.[24] This rate is higher than that of our patients with SAM (26.9%, p=0.043). The mortality rate of children admitted with overweight or obesity was 30.0% (p=0.772), which correlates with a previous study that found that risk-adjusted PICU mortality significantly increases as weight-for-height or body mass index increases into the overweight and obese ranges.[25]
Clinical instability on admission, history of prior cardiac arrest and emergency admission are variables known to be included in mortality prediction models,[19,26,27] and in our study were associated with mortality rates of 41.3% (p<0.001), 32.0% (p=0.021), and 18.0% (p<0.001), respectively. As expected for seriously ill patients, higher mortality rates corresponded with greater requirements for organ support, such as increasing inotrope needs (p<0.001), more invasive modes of respiratory support (p<0.001) and renal replacement therapy (p=0.004).
Of all patients admitted to the PICU, 36.6% experienced a delay of >24 hours between the time of acceptance and the time of admission, and a substantial group of patients were regarded as unstable at the time of admission, which suggests that they had not been adequately stabilised either prior or during transfer. A total of 9.9% of the accepted patients were not admitted, with 35.2% of these dying prior to arrival. These data highlight that the quality and timing of transportation of critically ill children can impact negatively on patient outcomes. A study undertaken in the same province in 2015 found that transfer to PICU took a mean of 9.5 (range 3.80 - 18.75) hours, 31.5% of patients were unstable on arrival and 8.8% of children died prior to transportation to PICU.[28]
Patients requiring tertiary-level care had a mortality rate of 20.6% compared with 10.2% in those requiring quaternary-level care (p<0.001). In contrast to the quaternary-level patients, most of those requiring tertiary-level care were referred from other facilities as emergencies, similarly to findings from other studies where patients who were transferred to PICUs from outside hospitals as emergencies had worse outcomes, increased severity of illness and increased use of resources compared with patients admitted from within the same hospital.[29] The mortality rate in readmitted patients of 23.5% was not statistically significant (p=0.104) and is in keeping with the findings of a PICU in another middle-income country where no statistically significant association between readmission and mortality was seen.[30]
The mortality rate (27.4%, p<0.001) of patients who were transfused blood products (blood, platelets or both) was similar to that found in a study in the same unit that reviewed blood transfusion strategies and found a mortality rate of 27.9% in patients who were managed according to a modified liberal transfusion strategy.[31] This was not in keeping with a previous SA study that showed that transfusion with blood products was not statistically significant for mortality.[32] Infection, particularly healthcare-associated infection, is commonplace in the PICU setting.[33] An increased mortality rate was noted in patients who had confirmed fungal infection (22.2%, p=0.004), which is in keeping with a previous finding that fungal infection (whether invasive or colonisation) has a significant contribution to mortality rates in the PICU.[33]
Factors influencing higher mortality rates in patients not admitted to PICU included moderate acute malnutrition (61.1%, p=0.011), prior cardiac arrest (100%, p<0.001), respiratory illness (53.5%, p<0.001) and referral from Area One or Two (32.9% and 51.3%, respectively, p=0.040). In patients denied access to PICU referred from a district or secondary-level hospital, mortality rates were 66.7% and 42.3%, respectively (p=0.039). District hospitals are without paediatricians and mostly in rural areas, with poor resources and inadequate facilities. This combination of factors, in addition to the long distances travelled to paediatric intensive care facilities, likely contributes to the high mortality rate. It is known that there is a high incidence of adverse events that occur during transfers of critically ill children.[34] A previous study showed increasing mortality rates with greater inter-hospital distances, but did not prove this to be statistically significant.[19]
A limitation of this study was that it was conducted at a single site and failed to evaluate the needs of the entire province; however, the other PICUs in KZN serve different geographical areas and none offer quaternary level care. Furthermore, there may have been a positive bias regarding the data of patients needing PICU facilities as the trauma, cardiothoracic, and neurosurgical ICUs also admit paediatric patients. Additionally, there was no objective assessment of severity of illness (Paediatric Index of Mortality 3 Score) prior to triaging for PICU, although the consultant attempted to evaluate severity via a telephonic consultation. Patients in extremis and those who died unexpectedly prior to a request for PICU care, or where appropriate referrals may not have been made due to the perception that they were unlikely to be accepted, could have led to an underestimation of the need for paediatric critical care. Despite these limitations, the quality and completeness of the data collected through the electronic system, the relatively large data set, and the detailed evaluation of site and level of care required of critically ill children, make these findings useful and relevant to local, national, and international policymakers.
Following this study, there has been growth of PICU services in KZN; with expanded bed numbers in Area One, at the new Dr Pixley Ka Isaka Seme Memorial Hospital in KwaMashu (eThekwini) and the revamped General Justice Gizenga Mpanza Regional Hospital in KwaDukuza (iLembe); and Area Three, at Queen Nandi Regional Hospital in Empangeni (King Cetshwayo).
Conclusion
We affirmed the value of PICU admission by the statistically significant difference in mortality rates between patients admitted and not admitted to PICU. There is a shortage of intensive care services. When utilising these resources, special consideration should be given with regard to the disease spectrum, the level of the referral hospital, a history of prior cardiac arrest and the stability of the patient prior to transfer. The current process of triaging, the quality and availability of inter-hospital transportation and the high rates of mortality associated with blood transfusions warrant further review. While the unmet need for PICU services is being addressed by increasing the capacity of tertiary-level critical care services in KZN, further studies are required to assess the impact of these additional services on the outcomes of critically ill children.
Declaration. The research for this study was done in partial fulfilment of the requirements for EC's MMed (Paed) degree at UKZN.
Acknowledgements. The authors would like to thank Dr Partson Tinarwo (Department of Biostatistics, UKZN) for his assistance with the statistical analysis.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. Naidoo K, Singh J, Lalloo U. A critical analysis of ICU/HC beds in South Africa: 2008 - 2009. S Afr Med J 2013;103(10):751-753. https://doi.org/10.7196%2Fsamj.6415 [ Links ]
2. Rhodes A, Moreno RP. Intensive care provision: A global problem. Rev Bras Ter Intensiva 2012;24(4):322-325. https://doi.org/10.1590/S0103-507X2012000400005 [ Links ]
3. Vukoja M, Riviello E, Gavrilovic S, et al. A survey on critical care resources and practices in low-and middle-income countries. Glob Heart 2014;9(3):337-342.e331-335. https://doi.org/10.1016/j.gheart.2014.08.002 [ Links ]
4. Siaw-Frimpong M, Touray S, Sefa N. Capacity of intensive care units in Ghana. J Crit Care 2021;61:76-81. https://doi.org/10.1016/j.jcrc.2020.10.009 [ Links ]
5. Horak RV, Griffin JF, Brown AM, et al. Growth and changing characteristics of pediatric intensive care 2001 - 2016. Crit Care Med 2019;47(8):1135-1142. https://doi.org/10.1097%2Fccm.0000000000003863 [ Links ]
6. Bamford LJ, McKerrow NH, Barron P, Aung Y. Child mortality in South Africa: Fewer deaths, but better data are needed. S Afr Med J 2018;108(3 Suppl 1):S25-S32. https://doi.org/10.7196/samj.2017.v108i3b.12779 [ Links ]
7. United Nations Children's Fund. Countdown 2015: Maternal, newborn and child survival. New York: World Health Organization, 2015. http://countdown2030.org/documents/2015Report/Countdown_to_2015_final_report.pdf (accessed 22 January 2022). [ Links ]
8. McKerrow N, Mulaudzi M. 2nd triennial report of the committee on morbidity and mortality in children under 5 years (COMMIC). South Africa: National Department of Health, 2014. http://www.kznhealth.gov.za/mcwh/2nd-CoMMiC-Triennial-Report-2014.pd (accessed 21 July 2016). [ Links ]
9. Gebhardt S. Saving Babies 2014 - 2016: Triennial report on perinatal mortality in South Africa. Pretoria: National Department of Health, 2018. https://www.westerncape.gov.za/assets/departments/health/napemmco_triennial_report_2014-2016_saving_babies.pdf (accessed 10 December 2021). [ Links ]
10. Stephen C. Saving Children 2012 - 2013: An eighth survey of child healthcare in South Africa. Pretoria: Tshepesa Press, MRC, CDC, 2016. https://www.up.ac.za/media/shared/717/Child%20PIP/Saving%20children%20reports/saving-children-2012-2013.zp207156.pdf (accessed 15 June 2016). [ Links ]
11. Lehohla P. Census 2011: Census in brief. Pretoria: Statistics South Africa, 2012. http://www.statssa.gov.za/census/census_2011/census_products/Census_2011_Census_in_brief.pdf (accessed 13 June 2016). [ Links ]
12. Scribante J, Bhagwanjee S. National audit of critical care resources in South Africa - research methodology S Afr Med J 2007;97(12 Pt 3):1308-1310. https://www.ncbi.nlm.nih.gov/pubmed/18265910 (accessed 14 June 2016). [ Links ]
13. Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med 2012;38(10):1647-1653. https://doi.org/10.1007/s00134-012-2627-8 [ Links ]
14. Muttalib F, González-Dambrauskas S, Lee JH, et al. Pediatric emergency and critical care resources and infrastructure in resource-limited settings: A multicountry survey. Crit Care Med 2021;49(4):671-681. https://doi.org/10.1097/ccm.0000000000004769 [ Links ]
15. Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: A systematic review. PLoS One 2015;10(1):e0116949. https://doi.org/10.1371/journal.pone.0116949 [ Links ]
16. Department of Health, KwaZulu-Natal. Referral system: Levels of health care. KwaZulu-Natal Department of Health Corporate Communication, 2014 (updated 4 January 2022). https://www.kznhealth.gov.za/Referral-system.ht (accessed 8 January 2022). [ Links ]
17. World Health Organization. Guideline: assessing and managing children at primary health-care facilities to prevent overweight and obesity in the context of the double burden of malnutrition. Updates for the Integrated Management of Childhood Illness (IMCI). Geneva: WHO, 2017. https://www.who.int/publications/i/item/9789241550123 (accessed 10 December 2021). [ Links ]
18. Jeena PM, Adhikari M. Provision of critical care services to HIV-infected children in an era of advanced intensive care and availability of combined antiretroviral therapy. Paediatr Int Child Health 2017;37(3):166-171. https://doi.org/10.1080/20469047.2016.1254892 [ Links ]
19. Hendricks CL, McKerrow NH, Hendricks RJ. Factors present on admission associated with increased mortality in children admitted to a paediatric intensive care unit (PICU). S Afr J Child Health 2016;10(1):57-62. https://doi.org/10.7196/SAJCH.2016.v10i1.1048 [ Links ]
20. Solomon LJ, Naidoo KD, Appel I, et al. Pediatric index of mortality 3 - an evaluation of function among ICUs in South Africa. Pediatr Crit Care Med 2021;22(9):813-821. https://doi.org/10.1097/pcc.0000000000002693 [ Links ]
21. Cowburn C, Hatherill M, Eley B, et al. Short-term mortality and implementation of antiretroviral treatment for critically ill HIV-infected children in a developing country. Arch Dis Child 2007;92(3):234-241. https://doi.org/10.1136/adc.2005.074856 [ Links ]
22. Argent AC, Ahrens J, Morrow BM, et al. Pediatric intensive care in South Africa: An account of making optimum use of limited resources at the Red Cross War Memorial Children's Hospital. Pediatr Crit Care Med 2014;15(1):7-14. https://doi.org/10.1097/PCC.0000000000000029 [ Links ]
23. Punchak M, Hall K, Seni A, et al. Epidemiology of disease and mortality from a PICU in Mozambique. Pediatr Crit Care Med 2018;19(11):e603-e610. https://doi.org/10.1097/pcc.0000000000001705 [ Links ]
24. Bagri NK, Jose B, Shah SK, Bhutia TD, Kabra SK, Lodha R. Impact of malnutrition on the outcome of critically ill children. Indian J Pediatr 2015;82(7):601-605. https://doi.org/10.1007/s12098-015-1738-y [ Links ]
25. Ross PA, Newth CJ, Leung D, Wetzel RC, Khemani RG. Obesity and mortality risk in critically ill children. Pediatrics 2016;137(3):e20152035. https://doi.org/10.1542/peds.2015-2035 [ Links ]
26. Straney L, Clements A, Parslow RC, et al. Paediatric index of mortality 3: An updated model for predicting mortality in pediatric intensive care. Pediatr Crit Care Med 2013;14(7):673-681. https://doi.org/10.1097/PCC.0b013e31829760cf [ Links ]
27. Straney LD, Schlapbach LJ, Yong G, et al Trends in PICU admission and survival rates in children in Australia and New Zealand following cardiac arrest. Pediatr Crit Care Med 2015;16(7):613-620. https://doi.org/10.1097/pcc.0000000000000425 [ Links ]
28. Royal C, McKerrow NH. A retrospective review of the transfer of critically ill children to tertiary care in KwaZulu-Natal Province, South Africa. S Afr J Child Health 2015;9(4):112-118. https://doi.org/10.7196/SAJCH.2015.v9i4.913 [ Links ]
29. Gregory CJ, Nasrollahzadeh F, Dharmar M, Parsapour K, Marcin JP. Comparison of critically ill and injured children transferred from referring hospitals versus in-house admissions. Pediatrics 2008;121(4):e906-911. https://doi.org/10.1542/peds.2007-2089 [ Links ]
30. Mat Bah MN, Syed Mohamed SA, Abdullah N, Alias EY. Unplanned PICU readmission in a middle-income country: Who is at risk and what is the outcome? Pediatr Crit Care Med 2020;21(11):e959-e966. https://doi.org/10.1097/pcc.0000000000002406 [ Links ]
31. Radebe PBS, Jeena PM. Red blood cell concentrate transfusion strategies utilised at a tertiary-level paediatric intensive care unit: A descriptive study on impact and cost. S Afr J Child Health 2018;12(4):164-169. https://doi.org/10.7196/SAJCH.2018.v12i4.1517 [ Links ]
32. Kruger I, Gie RP, Harvey J, Kruger M. Outcome of children admitted to a general high care unit in a regional hospital in the Western Cape, South Africa. S Afr J Child Health 2016;10(3):156-160. https://doi.org/10.7196/SAJCH.2016.v10i3.981 [ Links ]
33. Hlophe ST, Govender NP, Masekela R. Invasive fungal infections among critically ill children: Epidemiology, risk factors and outcomes. Afr J Thorac Crit Care Med 2018;24(1):11-14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8432925/pdf/AJTCCM-24-1-172.pdf (accessed 12 January 2021). [ Links ]
34. Hatherill M, Waggie Z, Reynolds L, Argent A. Transport of critically ill children in a resource-limited setting. Intensive Care Med 2003;29(9):1547-1554. https://doi.org/10.1007/s00134-003-1888-7 [ Links ]
 Correspondence:
Correspondence:
E Clarence
eclarence@gmail.com
Accepted 18 July 2022














