Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.10 Pretoria Out. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i10.16590
RESEARCH
Evaluating the neutrophil-to-lymphocyte ratio as an indicator for early referral of patients with COVID-19 pneumonia to a high-care facility
C A RetiefI; H J RetiefI; S van der MerweII
IMB ChB; Universitas Academic Hospital, Free State Department of Health, Bloemfontein, South Africa
IIBSc (Actuarial Science); Senior Lecturer: Mathematical Statistics and Actuarial Science and Co-ordinator: UFS Statistical Consultation Unit, Faculty of Natural and Agricultural Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Early identification of patients at high risk of severe disease requiring referral and treatment at a high-care facility is imperative in the management of COVID-19 pneumonia in a limited-resource setting, as transfer of unstable patients can be detrimental
OBJECTIVES: To examine the value of the neutrophil-to-lymphocyte ratio (NLR) calculated on admission to a healthcare facility as a predictor of the need for early referral to a high-care facility for further treatment
METHODS: We designed a cohort analytical study of 198 patients with COVID-19 pneumonia admitted to the COVID-19 unit at Universitas Academic Hospital in Bloemfontein, South Africa, between 20 May and 30 September 2021
RESULTS: Of the 198 patients enrolled in the study, 134 (67.7%) were admitted to high care and 93 (46.9%) died. The median (interquartile range (IQR)) NLR measured on admission to the hospital was 8.09 (4.90 - 14.86), and the NLR ranged from 0.26 to 136.7. The admission NLR was statistically significantly higher in the high-care group v. the general ward group (p<0.001). After converting the NLR to log scale, to bring it closer to conditional normality, logistic regression analysis identified log NLR (odds ratio (OR) 4.089; 95% confidence interval (CI) 2.464 - 6.787; p<0.001) and age (OR 1.029; 95% CI 1.004 - 1.056; p=0.024) as significant in determining who will require high care. The area under the receiver operating characteristic curve for the combined model of NLR and age was 0.829 (95% CI 0.767 - 0.891). An NLR cut-off value of 7.5 (sensitivity 0.7462, specificity 0.7968j has been calculated as the optimal cut-off value to determine who will need high care. Admission log NLR and age were significant in determining who died (OR 2.067; 95% CI 1.404 - 3.045; p<0.001, and OR 1.043; 95% CI 1.018 - 1.068; p=0.001, respectively
CONCLUSION: The NLR measured on admission and age can be used to predict whether a patient with COVID-19 pneumonia will require high care
The ongoing COVID-19 pandemic has placed significant strain on the South African (SA) public healthcare sector, emphasising pre-existing weaknesses in the system. One such challenge brought to light at Universitas Academic Hospital, Bloemfontein, during the pandemic was the difficulty surrounding interhospital patient transfers in Free State Province. With our facility being one of the main high-care treatment centres in the province, we received referrals from hospitals up to 300 km from Bloemfontein. In addition to large travelling distances, the poor road conditions, scarcity of ambulances, and increased overall pressure on the emergency medical services caused by the pandemic further hampered efficient transfer of patients.
Peripheral hospitals in Free State are equipped to provide basic supplemental oxygen therapy to patients with COVID-19 pneumonia via nasal cannula or face mask. Only select hospitals can escalate care to high-flow nasal cannula oxygen therapy. Non-invasive ventilation (NIV) is only available at the high-care centres established at the larger referral hospitals in Bloemfontein, so patients who fail to improve when receiving the highest available oxygen modality at their local hospital, or present with severe disease requiring NIV, need to be referred to these high-care units.
The transfer of critically ill and unstable patients with high oxygen demands can be hazardous, and can result in respiratory deterioration during transit that negatively affects patient outcomes.[1] To avoid this additional insult, every possible attempt at early identification and referral of patients who may require further treatment in a high-care unit should be made.
The neutrophil-to-lymphocyte ratio (NLR) is an inflammatory marker calculated by using the absolute neutrophil and lymphocyte counts measured in the peripheral blood.[2] The NLR has been established as a valid prognostic factor in various chronic diseases and solid tumours.[3] Recent studies have concluded that the NLR can also be used in COVID-19 patients as a prognostic tool for early risk stratification on hospital admission, and that the NLR is independently associated with progression to critical illness.[2-7]
Our objective with this study was to determine whether the NLR can be used to assist clinicians in peripheral hospitals to identify patients who will benefit from early referral to a high-care facility.
Methods
Study design and participants
This was a retrospective single-centre study of 198 patients with COVID-19 pneumonia admitted to the COVID-19 unit at Universitas Academic Hospital, Bloemfontein, between 20 May and 30 September 2021. The diagnosis was based on either a positive throat swab antigen test or a polymerase chain reaction test, with features of COVID-19 pneumonia on a chest radiograph. Based on clinical parameters, patients were admitted to either the high-care or the general ward of our COVID-19 unit. Only patients with documented absolute neutrophil and lymphocyte counts on admission and with a length of hospital stay >24 hours were included in the study. Our primary aim was to evaluate the prognostic value of the NLR at admission in prediction of the level of care required. Our secondary aim was to validate NLR on admission as a predictor of outcome in our population.
The study was approved by the Health Sciences Research Ethics Committee of the University of the Free State (ref. no. UFS-HSD2021/1771/2501), and by the Free State Department of Health.
Data collection
Eligible patient files were assigned a study number to ensure confidentiality, and no personal information was entered on a standardised electronic datasheet. The admission NLR was calculated for every patient by dividing the admission neutrophil count by the admission lymphocyte count. Demographic (age and gender), treatment (high care or general ward) and outcome (death or discharge) data were extracted from the participant files and added to the datasheet.
Statistical analysis
Descriptive statistics were presented as counts (percentages) tor categorical variables and as medians (lower quartile, upper quartile) for continuous variables. Box plots were used to visualise the distribution of data and to verify the assumptions of the statistical tests. The primary explanatory variable, NLR, where measurements were skew, was converted to a log scale to avoid distortion of results and bring it closer to approximate conditional normality.
To model the impact of log NLR on the probability of a treatment level or outcome, while adjusting for the influence of age and gender, logistic regression models were used. A p-value <0.05 was considered statistically significant. After fitting, the proposed model was visualised using line plots and its predictive power was evaluated via a receiver operating characteristic (ROC) curve. The effect of age and gender on treatment and outcome was also evaluated in univariate tests, specifically f-tests and x2 tests as appropriate. The results of these tests, along with information criteria (Akaike information criterion and Bayesian information criterion), were used to determine the appropriate model form.
Finally, non-linear equivalents of the logistic regression models were also considered in the form of classification trees, specifically recursive partitioning trees.'8 These can produce simple-to-follow decision pathways for clinical use, particularly when relationships are non-linear. All statistical analysis was conducted by the Statistical Consultation Unit, University of the Free State, using R (R Core Team, Austria, 2021).[9]
Results
Descriptive statistics and demographics
Of the 198 patients included in the study, 86 (43.4%) were male, and the median (interquartile range (IQR)) age of the study group was 59 (48.0 - 66.75) years; 134 patients (67.7%) were admitted to high care and 93 (46.9%) died.
Fig. 1 provides visual confirmation of the statistical difference in admission NLR between the high-care and general ward groups. The median (IQR) NLR measured on admission to hospital was 8.09 (4.90 - 14.86), and the NLR ranged from 0.26 to 136.7. When comparing the high-care group with the general group, the median NLR for patients admitted to high care was 11.19 (7.30 - 17.78) and that for patients admitted to the general ward was 4.04 (2.78 - 6.81). A Wilcoxon rank-sum test indicated that the admission NLR was statistically significantly higher in the high-care group than in the general group (p<0.001).
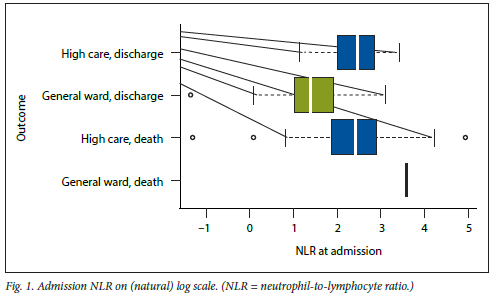
Fig. 2 demonstrates the kernel density plots of NLR on a log scale for the high-care and general ward groups. Visual discrimination based on the point of intersection suggested that the optimal point of discrimination in NLR was at e2.01 = 7.5. At this point, the overlap of high-care cases with a lower NLR was 25%.

When considering NLR in isolation, simple discrimination using a confusion matrix showed that an NLR >7.5 had a sensitivity of 0.7462 and a specificity of 0.7968 in predicting admission to high care. Logistic regression analysis was applied to identify factors that influenced admission to high care. The log NLR (p<0.001) and older age (p=0.024) were significant. Gender did not play a role in the level of care. The final model, with the implied odds ratios, is given in Table 1.
Visualisation
The logistic regression model connects the observed explanatory variable values (in this case log NLR and age) to the latent probability of requiring high care, which underlies where the patient ends up. Fig. 3 shows that patients with an NLR of 7.5 at admission have at least a 50% probability of requiring high care, regardless of age. For older patients the probability of requiring high care is systematically higher at any NLR, to the extent that the oldest patients are very likely to require high care, even with a relatively low NLR at admission.

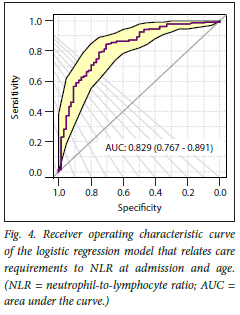
While it may seem intuitive to choose a threshold for NLR at a 50% probability of requiring high care, this is not optimal in two respects. Firstly, we can achieve high rates of total classification accuracy by varying the threshold probability. In Fig. 4, the sensitivity and specificity of the classification are evaluated at various thresholds, resulting in the curve shown. It appears that there is a distinct turn in the curve at a specificity of 0.7, corresponding with a probability threshold of 0.61 (61%). This is also the point on the ROC curve furthest away from the 45° line of random classification. Secondly, this analysis does not weigh the costs of a false positive against the costs of a false negative, which can vary by context.
Patient outcomes
Further analysis of the group of patients who survived to discharge and those who died shows that the median (IQR) admission NLR for patients who were alive on discharge was 6.57 (3.49 - 11.13) v. 11.24 (6.62 - 18.25) for patients who died. The admission NLR was significantly higher in patients who died (p<0.001). Applying logistic regression to adjust for age and gender, considering the three factors additively on the logistic scale, the log NLR (p<0.001) and age (p=0.001) had a significant effect on outcome (Table 2). Gender played no role.
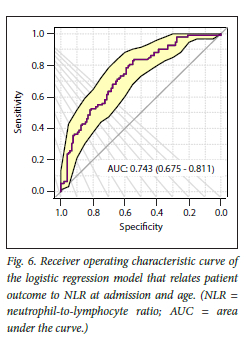
Considering the model visualisations in Figs 5 and 6, we see that patient outcome does not allow for clear discrimination based on the factors considered alone.

Discussion
This study confirmed that there is asignificant association between the admission NLR and the level of care required for a patient with COVID-19 pneumonia, and that a higher NLR was associated with increased mortality. Our study findings revealed that an NLR of 7.5 is the optimal early point of discrimination for our population. Recursive partitioning decision tree analysis of the level of care is shown in Fig. 7. The result is a set of rules that can be applied in a clinical setting. If the admission NLR is >7.5, the patient needs to be admitted to high care, regardless of other factors. If it is lower, the patients age should be considered. Patients can be admitted to the general ward if they are <42 years of age with an NLR <7.5, <53 years of age with an NLR <4.1, or >53 years of age with an NLR <2.2. Other groups have inconclusive classifications, where other factors may play a stronger role.

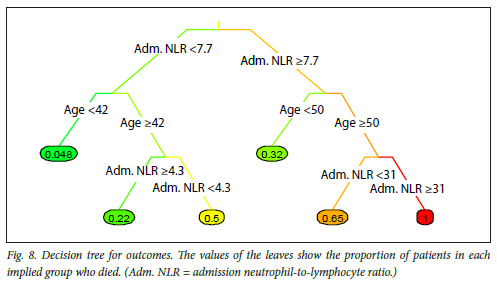
In Fig. 7, the values of the leaves show the proportion of patients in each implied group who were given high care. For patient outcome (Fig. 8), the decision tree analysis was inconclusive, other than suggesting that younger patients may expect more favourable outcomes, while those with a high NLR may expect worse outcomes.
In general, older individuals were found to have an increased likelihood of requiring admission to high care and to have an increased mortality rate. Our results are consistent with those of previous reports.[7] Gender did not have any statistically significant influence on level of care or mortality.
There are several limitations of the study. Firstly, the admission NLR used was calculated from the laboratory values obtained on admission to our institution, but many patients had been admitted to other local hospitals prior to referral to us. The impact of any treatment and/or disease progression during this initial admission period on the NLR that we calculated on admission to our facility cannot be determined. Secondly, this was a single-centre retrospective study with a small study population, and we only assessed the influence of age, gender and NLR on the level of care required. A study (N=352) recently reported that the NLR can be used to predict disease deterioration and serious clinical outcomes with an NLR >2.6937,[4] and this could indicate that the ideal NLR cut-off value for our population may be lower than our calculated value. We advise that further studies should include other relevant data, such as comorbidities that may influence level of care and outcome. This will enable researchers to refine the NLR cut-off point.
With the results obtained from our study, we hope to be able to formulate a simple risk stratification tool that can be implemented in the management of patients with COVID-19 pneumonia. Our primary goal will be to enable clinicians in peripheral hospitals to identify patients with COVID-19 pneumonia who will benefit from early referral to a facility with access to a high-care unit, aiming to prevent delays in referral resulting in the transfer of patients in an unstable condition. Existing scoring systems such as the Acute Physiology and Chronic Health Evaluation (APACHE II) score and the COVID-GRAM require advanced laboratory examinations, and implementing these scoring systems in a resource-limited peripheral hospital setting is therefore not feasible.[2] Furthermore, a meta-analysis revealed the NLR to be a valuable independent prognostic marker with higher diagnostic accuracy than other risk assessment tools, such as the CURB-65 score.[10]
Conclusion
We conclude that the admission NLR has a high value in predicting disease progression and therefore the level of care that will be required to manage a patient with COVID-19 pneumonia. Our findings support use of the NLR on admission to perform early risk stratification in remote resource-limited settings. Patients with a higher NLR on admission (our study findings suggested a threshold value of 7.5) are candidates for early referral to a high-care facility. A higher NLR and increasing age were also associated with poorer prognoses. However, further research (perhaps taking hospital-specific factors into account) should be conducted to obtain an exact consensus cut-off value with optimal sensitivity and specificity.
Declaration. None.
Acknowledgements. None.
Author contributions. H JR and CAR were responsible for the conception of the study and data collection. HJR and SvdM analysed and interpreted the data. CAR and HJR drafted the manuscript. All authors participated in the editing of the manuscript. All authors approved the final draft.
Funding. None.
Conflicts of interest. None.
References
1. Mendelson M, Booyens L, Boutajl A, et al. The mechanics of setting up a COVID-19 response. Experiences of the COVID-19 epidemic from Groote Schuur Hospital, Cape Town, South Africa. S Afr Med J 2020;110(10):968-972. https://doi.org/10.7196/SAMJ.2020.vll0il0.15215 [ Links ]
2. Simadibrata D, Calvin J, Wijaya A, Ibrahim N. Neutrophil-to-lymphocyte ratio on admission to predict the severity and mortality of COVID-19 patients. A meta-analysis. Am J Emerg Med 2021;42:60-69. https://doi.org/10.1016/j.ajem.2021.01.006 [ Links ]
3. Ciccullo A, Borghetti A, Zileri dal Verme L, et al. Neutrophil-to-lymphocyte ratio and clinical outcome in COVID-19. A report from the Italian front line. Int J Antimicrob Agents 2020;56(2):106017. https://doi.org/10.1016/j.ijantimicag.2020.106017 [ Links ]
4. Zeng Z-Y, Feng S-D, Chen G-P, Wu J-N. Predictive value of the neutrophil to lymphocyte ratio for disease deterioration and serious adverse outcomes in patients with COVID-19. A prospective cohort study BMC InfectDis 2021;21(1):80. https://doi.org/10.1186/sl2879-021-05796-3 [ Links ]
5. Cheng B, Hu J, Zuo X, et al Predictors of progression from moderate to severe coronavirus disease 2019. A retrospective cohort. Clin Microbiol Infect 2020;26(10):1400-1405. https://doi.org/10.1016/j.cmi.2020.06.033 [ Links ]
6. Kong M, Zhang H, Cao X, Mao X, Lu Z Higher level of neutrophil-to-lymphocyte is associated with severe COVID-19. Epidemiol Infect 2020;148:el39. https://doi.org/10.1017/S0950268820001557 [ Links ]
7. Lian J, Jin C, Hao S, et al. High neutrophil-to-lymphocyte ratio associated with progression to critical illness in older patients with COVID-19. A multicenter retrospective study Aging 2020;12(14):13849-13859. https://doi.org/10.18632/agingl03582 [ Links ]
8. Gordon A, Breiman L, Friedman J, Olshen R, Stone C. Classification and regression trees. Biometrics 1984;40(3):874. [ Links ]
9. R Core Team. R A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria, 2021. https://www.R-project.org/ (accessed 7 March 2022) [ Links ]
10. Alkhatip A, Kamel M, Hamza M, et al The diagnostic and prognostic role of neutrophil-to-lymphocyte ratio in COVID-19. A systematic review and meta-analysis. Expert Rev Mol Diagn 2021;21(5):505-514. https://doi.org/10.1080/14737159.2021.1915773 [ Links ]
 Correspondence:
Correspondence:
C A Retief
vw.carin@gmail.com
Accepted 23 May 2022














