Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 n.10 Pretoria Oct. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i10.16471
IN PRACTICE
Fetal intervention (EXIT procedure) for a rare fetal abnormality in a public sector hospital in South Africa - exploring what is possible
C J M StewartI; S PeerII; A NumanogluIII; K FieggenIV; D van DykV; K BesterVI
IMB ChB, FCOG (SA); Department of Obstetrics and Gynaecology, University of Cape Town, and Groote Schuur Hospital, Cape Town, South Africa
IIMB BCh, MMed (Otol); Division of Otolaryngology, University of Cape Town and Red Cross War Memorial Children's Hospital, Cape Town, South Africa
IIIMB ChB, FCS (SA); Division of Paediatric Surgery, University of Cape Town and Red Cross War Memorial Children's Hospital, Cape Town, South Africa
IVMB ChB, FCPaed (SA); Division of Human Genetics, Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VMB ChB, FCA (SA); Department of Anaesthetics, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VIMB ChB, FCA (SA); Division of Paediatric Anaesthesia, Department of Anaesthesia and Perioperative Medicine, University of Cape Town and Red Cross War Memorial Children's Hospital, Cape Town, South Africa
ABSTRACT
Congenital high airway obstruction syndrome (CHAOS) is a rare condition that can be diagnosed antenatally by ultrasound. It is usually lethal without immediate intervention at delivery. A 24-year-old woman was diagnosed with fetal CHAOS at 27 weeks' gestation. The couple declined termination of pregnancy. A multidisciplinary team including obstetricians, geneticists, paediatric surgeons, neonatologists and anaesthetists was constituted to plan an ex utero intrapartum treatment (EXIT) procedure. After several simulations, a caesarean section was performed at 38 weeks' gestation under deep inhalational anaesthesia. The fetus was fully delivered with placenta remaining in utero to maintain perfusion. A surgical airway was established via tracheostomy in approximately 5 minutes. The operation was then completed with no maternal complications. The child remains well at 3 years of age. To our knowledge, this is the first EXIT procedure performed for CHAOS in the public sector. This procedure can be lifesaving and is possible with proper planning.
Congenital high airway obstruction syndrome (CHAOS) is a rare condition, the incidence of which is unclear, where there is complete or near-complete obstruction of the upper airway. It can be diagnosed antenatally by the characteristic ultrasonographic findings of enlarged echogenic lungs, eversion of the diaphragm and dilatation of the bronchial tree distal to the obstruction.[1] The sequelae of the condition are fetal cardiac failure with hydrops and, without fetal or intrapartum intervention, is usually fatal after birth.
The most common cause of CHAOS is laryngeal atresia, although other variations exist, and the majority result in complete occlusion of the upper airway. Given the range of causes and the spectrum of severity, careful prenatal assessment is necessary to select patients for fetal or intrapartum intervention. Before any intervention is undertaken, a careful sonographic examination should be undertaken to exclude any other structural abnormalities, and chromosomal abnormalities sought. Fetal magnetic resonance imaging (MRI) may be useful.
Delivery by ex utero intrapartum treatment (EXIT) procedure has been described as the optimal management for this condition.[2,3] Operations on placental support (OOPS), also referred to as EXIT, are performed before clamping the umbilical cord, and by maintaining delivery of oxygen to the fetus via the placental circulation while fetal airway management with intubation or tracheostomy is performed. The first successful case was described in 1992 by Catalano et al.[4] in a fetus presenting with an epignathus tumour. Since then, several cases of cervical tumours leading to airway obstruction have been successfully managed in this way.
The use of EXIT procedures in patients with CHAOS has led to reports of good mid- and long-term outcomes.[6-8] Challenges with this form of intervention are (i) identification of the aetiology and degree of fetal airway obstruction; and (ii) combining airway management on placental support with minimal maternal morbidity and good fetal outcome. In addition to management of the umbilical cord, an anaesthetic protocol that allows for complete uterine relaxation and avoidance of any decrease in uteroplacental blood flow is essential. These factors have to be balanced against the risk of uterine haemorrhage. Careful patient selection for fetus and mother are crucial to a successful outcome.
While the EXIT procedure is now commonly used, reports of its use in CHAOS syndrome are sparse. In addition, most reports are from developed countries, with developing countries bearing the burden of inadequate resources, trained personnel and necessary equipment.
Case presentation
A 24-year-old gravida 2 para 1 was referred to the Fetal Medicine Unit at our tertiary hospital at 27 weeks and 6 days' gestation with the finding of a lung abnormality. She had had an otherwise unremarkable pregnancy. Her previous pregnancy 5 years earlier had resulted in the normal delivery of a healthy boy.
She had an unremarkable medical history and a normal body mass index. On ultrasound examination, the fetal lungs were markedly enlarged and echogenic with eversion of the diaphragm (Fig. 1). The trachea was seen throughout its length and was slightly dilated.

Moderate ascites was noted as well as polyhydramnios with an amniotic fluid index of 24. There was mild unilateral ventriculomegaly of 10 mm, and no other structural abnormalities were noted.
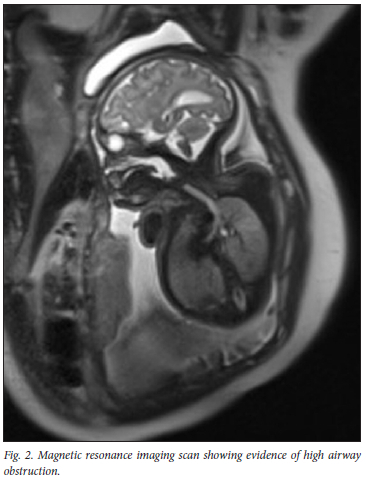
An amniocentesis revealed a 46XX karyotype. An MRI confirmed the findings (Fig. 2), and a diagnosis of CHAOS was made. The obstruction was thought to be at the level of the larynx.
The couple were offered the options of termination of pregnancy, non-intervention at delivery with likely demise, or EXIT. It was explained to the parents that an EXIT procedure had not previously been performed at our hospital. They declined termination of the pregnancy and wished to explore the option of an EXIT procedure.
After extensive counselling on the risks associated with the procedure, a multidisciplinary team was convened, consisting of obstetricians, fetal medicine specialists, neonatologists, paediatric surgeons, paediatric ear, nose and throat (ENT) surgeons and obstetric and paediatric anaesthetists. After considering all the information, it was agreed that intubation should not be attempted, but to proceed directly to a tracheostomy. The procedure was planned for 37 weeks' gestation, and two simulations were performed prior to this in the theatre with all relevant personnel.
On the day of surgery, theatre preparation included warming of the operating room to 37°C and setting up of a cell-saver and blood warming devices. Rapid-sequence induction of general anaesthesia was performed, and anaesthesia was maintained with a deep volatile-based technique, employing end-tidal concentrations of sevoflurane between 3.9% and 4.2% from the period prior to uterine incision until cord clamping. This resulted in a suitably flaccid uterus throughout fetal delivery and subsequent tracheostomy. This deep anaesthesia necessitated the use of phenylephrine and adrenaline infusions to maintain maternal haemodynamic stability within 5% of preoperative values. Higher-than-usual inspired oxygen concentrations were supplied to promote adequate fetal oxygenation during the period of fetal tracheostomy. Potent opiate analgesia was administered after induction, with the intention that placental transfer would provide fetal analgesia for the procedure.
After cleaning and draping of the mother, a sterile mayo tray was placed on her thighs to receive the fetus for the tracheostomy, while on placental support.
Two senior obstetricians performed the caesarean section. A midline skin incision was made. The placenta was posterior and fundal and the uterus was thus entered through a lower uterine segment incision. The fetus was fully delivered (as previously agreed).
Uterine relaxation was maintained and the cord was covered with plastic, avoiding any manipulation. The baby was delivered onto the mayo tray on the mother's thighs. She was patted dry and placed in a supine position with a small roll under the shoulders, facilitating mild head extension. A paediatric anaesthetist had prepared drugs and an Ayre's T-piece in the sterile field. The anaesthetist attached an oxygen saturation probe and administered 3 mg rocuronium by intramuscular injection. Three litres of warm saline were infused into the uterus to keep it from contracting. Two paediatric ENT surgeons performed a vertical tracheostomy between the second and third ring (Fig. 3). On entry into the trachea, gelatinous fluid was suctioned, confirming an occlusive larynx above. The tracheal lumen was identified and a size 3.5 NEO Shiley cuffless tracheostomy was easily inserted. The procedure was completed in <6 minutes. The Ayre's T-piece was used for rescue breaths while the cord was clamped and divided, after which the baby was transferred out of the sterile area. Auscultation of the lungs confirmed bilateral air entry together with chest rise, and confirmed correct positioning of the tracheostomy tube. During this period, assessments of both maternal and neonatal condition were made by an independent monitor at 30-second intervals.

After cord clamping, the anaesthetic management priority shifted to promotion of uterine contraction to prevent postpartum haemorrhage. The end-tidal concentration of sevoflurane was reduced and nitrous oxide was introduced to ensure adequate anaesthetic depth. An oxytocin infusion and rectal misoprostol were administered to aid uterine contraction. The total blood loss at the caesarean section was 800 mL. The mother's condition was stable throughout, and there were no intraoperative complications and no requirement for blood transfusion. Once the surgical airway was established in the baby via tracheostomy, she was moved to a neonatal incubator in the operating room for securing the airway. Left and right stay sutures were inserted, a necessary step in all babies with no proximal airway. After stabilisation in the neonatal intensive care unit, the baby was transferred to the paediatric hospital for further specialised care.
The infant was small for gestational age at 2.5 kg. A solid cricoid plate with no lumen and fused vocal cords was noted on direct laryngoscopy at 1 month of age. A ventricular septal defect was repaired at the age of 6 months. No other structural congenital abnormalities were identified, but the child has some soft dysmorphic features and global developmental delay. A chromosomal microarray revealed only a variant of uncertain significance that was not thought to explain the dysmorphic features. Despite numerous short admissions for respiratory tract infections, the child is making steady developmental progress and is an integral part of her family. She is being worked up for laryngeal reconstruction when older.
Discussion
Our case report describes a case of CHAOS due to laryngeal atresia where the baby was delivered at term by EXIT/OOPS procedure for an immediate tracheostomy to bypass the laryngeal obstruction, with good outcome for the mother and child.
Operations on placental support were developed to improve the prognosis for fetuses where a prenatal diagnosis of upper airway obstruction had been made. This has sometimes been due to compression by cervical teratomas or other tumours.[9] While CHAOS is a further indication for this method of intervention, there are few reported cases in the literature where EXIT procedure followed by intubation or tracheostomy has been performed for this indication with successful outcome.[2,5,7,8,10-13]
With advances in imaging technology, CHAOS can be diagnosed relatively easily antenatally by ultrasound findings of enlarged echogenic lungs, eversion of the diaphragm and tracheal dilatation, as was the case in our patient. MRI has been used to delineate more accurately the level of the lesion and its aetiology. More recently, attempts have been made to define poor prognostic factors and, in these cases, fetal bronchoscopy and tracheoplasty have been attempted prior to EXIT procedure and tracheostomy at delivery.[14] Without intervention, the condition is usually fatal shortly after birth.
As with all fetal surgery, ethical dilemmas exist regarding the risks to the mother compared with the benefit to the fetus. In the case of EXIT procedure, deep general anaesthesia is required to allow complete uterine relaxation while the surgery to the partially delivered baby is undertaken. This carries a risk of haemorrhage in the mother, which increases with the duration of surgery. Deep anaesthesia also results in maternal hypotension, often necessitating the use of adrenaline, as in our case. The baby runs the risk of hypoxia during the surgery and therefore it is essential to monitor its oxygenation with pulse oximetry to prevent hypoxic brain damage.
In our case, laryngeal atresia was considered highly likely following the serial imaging. It was therefore decided that intubation would not be an option, and that immediate resort to tracheostomy carried the least risk to the mother and baby, and this was likely to be a shorter procedure. It was also decided to fully deliver the baby while keeping the umbilical cord attached to the placenta. This decision was made to facilitate ease of access during surgery. To avoid any undue stretch on the umbilical cord, a tray was placed on the mother's thighs to receive the fetus, thereby performing the tracheostomy a short distance from the uterus. The procedure was successfully completed in under 6 minutes, with adequate oxygenation to the baby and no excessive maternal bleeding. We regarded it as an essential part of the management to have in situ simulations prior to the surgery, so that key players knew their roles well, and any potential issues could be addressed. We also considered it essential to have full and extensive counselling of the couple that included psychological support during the latter half of the pregnancy. The multidisciplinary collaboration included several meetings and discussions prior to delivery.
We therefore report this rare case of CHAOS where the parents declined termination of the pregnancy and an EXIT/OOPS procedure with tracheostomy was performed with a good outcome.
Several small series have reported similar couples who elected to terminate their pregnancies, with a small number proceeding to term with variable outcomes following intervention. We describe the first case of intervention for this condition performed in our centre that functions in a low-resource setting. A multidisciplinary team of specialists is therefore able to successfully perform a highly skilled procedure through careful and thorough planning. Good maternal and fetal patient selection is also key to a successful outcome. It may serve as a guide to other units in similar settings and emphasises the important aspects of counselling, multidisciplinary collaboration, knowledge and surgical expertise, ethical considerations, pre-delivery simulations and decisions regarding the best procedure in the specific circumstances.
Teaching points and conclusion
• CHAOS, a rare condition most commonly due to laryngeal atresia, which is generally fatal without intervention can be effectively managed with successful outcome.
• EXIT procedures can be successful even in a low-resource setting, with adequate planning, simulations and multidisciplinary collaboration.
• Pre-operative decision-making regarding the best method of establishing the airway is important.
• Full delivery of the baby with maintenance of placental support is an option that decreases operative time and bleeding risk.
Declaration. The parents of the child have given their written informed consent to publish their case (including publication of images).
Acknowledgements. Neonatology Unit, Groote Schuur Hospital, for assistance during the peripartum period.
Author contributions. All authors were involved in the clinical management of the patient. CS, KF and DvD were involved in the drafting of the manuscript with input from the other authors. All authors reviewed the intellectual content and approved the final version of the document.
Funding. None.
Conflicts of interest. None.
References
1. Hedrick MH, Ferro MM, Filly RA, Flake AW, Harrison MR, Adzick NS. Congenital high airway obstruction syndrome (CHAOS): A potential for perinatal intervention. J Pediatr Surg 1994;29(2):271-274. https://doi.org/10.1016/0022-3468(94)90331-x [ Links ]
2. Saadai P, Jelin EB, Nijagal A, et al. Long-term outcomes after fetal therapy for congenital high airway obstructive syndromse. J Pediatr Surg 2012;47(6):1095-1100. https://doi.org/10.1016/j.jpedsurg.2012.03.015 [ Links ]
3. Nicolas CT, Lynch-Salamon ED, Bendel-Stenzal E, et al. Fetoscopically-assisted percutaneous decompression of the distal trachea and lung reverses fetal hydrops and fetal distress in a fetus with laryngeal atresia. Fetal Diagn Ther 2019;46(1):75-80. https://doi.org/10.1159/000500455 [ Links ]
4. Catalano PJ, Urken ML, Alvarez M, et al New approach to the management of airway obstruction in 'high-risk' neonates. Arch Otolaryngol Head Neck Surg 1992;108(3):306-309. https://doi.org/10.1001/archotol.1992.01880030094019 [ Links ]
5. Bouchard S, Johnson HP, Flake AW, Howell LJ, Myers LB, Adzick NS. The EXIT procedure: Experience and outcome in 31 cases. J Pediatr Surg 2002;37(3):418-426. https://doi.org/10.1053/jpsu.2002.30839 [ Links ]
6. Hirose S, Harrison MR. The ex utero intrapartum (EXIT) procedure. Semin Neonatol 2003;8(3):207-214. [ Links ]
7. Shimabukuro F, Sakumoto K, Masamoto H, et al A case of congenital high airway obstruction syndrome managed by ex utero intrapartum treatment: Case report and review of the literature. Am J Perinatol 2007;24(3):197-201. https://doi.org/10.1055/s-2007-972928 [ Links ]
8. Crombleholme TM, Sylvester K, Flake AW, Adzick NS. Salvage of a fetus with congenital high airway obstruction syndrome by ex utero intrapartum (EXIT) procedure. Fetal Diagn Ther 2000;15(5):280-282. https://doi.org/10.1159/000021022 [ Links ]
9. Barthod G, Teissier T, Bellarbi N, et al. Fetal airway management on placental support: Limitations and ethical considerations in seven cases. J Obstet Gynaecol 2013;33:787-794. https://doi.org/10.3109/01443615.2013.823924 [ Links ]
10. Paek BW, Callen PW, Kitterman J, et al. Successful intervention for congenital high airway obstructions syndrome. Fetal Diagn Ther 2002;17(5):272-276. https://doi.org/10.1159/000063179 [ Links ]
11. Yaneza MM, Cameron A, Clement WA, et al. An interventional airway delivery service for congenital high airway obstruction. J Laryngol Otol 2015:129(8):795-800. https://doi.org/10.1017/s0022215115000900 [ Links ]
12. Elliott R, Vallera C, Heitmiller ES, et al. Ex utero intrapartum treatment procedure for management of high airway obstruction syndrome in a vertex/ breech twin gestation. Int J Pediatr Otorhinolaryngol 2012;77:439-442. https://doi.org/10.1016/j.ijporl2012.11.023 [ Links ]
13. Botto HA, Boailchuk ID, Garcia C, Decaro M, Aiello H, Copich J. Ex utero intrapartum treatment-management of neonatal congenital high airway obstruction syndrome: A case report. Arch Argent Pediatr 2010;108(4):e92-95. https://doi.org/10.1590/s0325-00752010000400013 [ Links ]
14. Nolan HR, Gurria J, Peiro JL, et al. Congenital high airway obstruction syndrome (CHAOS): Natural history, prenatal management strategies, and outcomes at a single comprehensive fetal center. Neonat Fetal Cond 2019;54(6):1153-1158. https://doi.org/10.1016/j.jpedsurg.2019.02.034 [ Links ]
 Correspondence:
Correspondence:
C Stewart
Chantal.Stewart@westerncape.gov.za
Accepted 30 May 2022














