Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.8 Pretoria Ago. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i8.16271
RESEARCH
https://doi.org/10.7196/samj.2022.v112i8.16271
A paediatric pain assessment and management survey at Rahima Moosa Mother and Child Hospital, Johannesburg, South Africa
L M N MabasoI; A BhettayII; R BandiniIII; D DemopoulosIV
IFC Paed (SA), MMed (Paed Child Health); Department of Paediatrics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIFCA (SA), MMed (Anaes); Department of Anaesthesia and Perioperative Medicine, Red Cross War Memorial Children's Hospital and Faculty of Health Sciences., University of Cape Town, South Africa
IIIBSc Hons; School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; PRINCE (Project to Improve Neonatal Care), Johannesburg, South Africa
IVMMed (Paed), Cert Crit Care (Paed) (SA); Wits Donald Gordon Medical Centre, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Painful experiences are common in the paediatric inpatient population. Immaturity and cognitive impairment may preclude clear description of such experiences, and requests for analgesia when needed. Methods of pain assessment and guidelines for treatment in the paediatric population are well established, but are not widely used. Limited data suggest that the situation is similar in South Africa (SA
OBJECTIVES: To review the assessment and management of pain in SA medical paediatric inpatients. The primary objective was to determine the proportion of children who receive analgesia where indicated. The secondary objectives were to determine the prevalence of pain, at presentation and among admitted patients, whether pain evaluations were performed and pain treated, and the adequacy of such treatment
METHODS: A prospective cross-sectional survey of medical paediatric inpatients at Rahima Moosa Mother and Child Hospital (RMMCH) in Johannesburg, SA, was conducted. The tool used for data collection was specifically designed for the study, with sections for demographic data, patient or caregiver interview, and chart review. Pain assessments were done using the revised Face, Legs, Activity, Cry, Consolability Scale and the Neonatal/Infant Pain Scale. The analysis consisted of descriptive statistics of epidemiological data and comparative statistics using grouped variables, with the level of significance set at p<0.05
RESULTS: The sample consisted of 74 children, aged between 3 days and 4 years. Male patients accounted for 58% of the cohort. The prevalence of pain at admission was 73% (n=53). Eight percent (n=6) of the study sample had pain evaluation at admission, and only 1 child had been evaluated for pain within the preceding 24 hours. Of the 74 patients reviewed, 10% (n=7) received appropriate analgesia. Paracetamol was given to 31% of patients (n=23), either for pyrexia or for an undocumented indication. More than half of the study sample (59%; n=44) received no analgesia. The presence of pain, both by caregiver report (p=0.62) and by pain score (p=0.074), was not associated with the administration of analgesia
CONCLUSION: Pain in the paediatric population at RMMCH was found to be common, but it was seldom assessed, and validated pain scores were rarely used. The result was inadequate pain management in all the four domains of assessment, intervention, reassessment and ongoing management
Pain, defined as an unpleasant physical or emotional experience that is associated with actual or potential tissue damage, is a personal and subjective experience.[1,2] It is prevalent in the paediatric population, as part of both surgical and medical pathology[3-5] The gold standard of pain assessment is by self-report.[2] This method proves difficult in children whose neurodevelopmental immaturity precludes coherent description of painful experiences and competent requests for analgesia when needed. Cognitively impaired patients are a particularly vulnerable group. Depending on their level of ability some depend only on non-verbal communication. This unique set of circumstances has led to the development of several validated pain assessment tools for children of all ages, as well as for children with cognitive impairment.
Use of a pain score allows selection of appropriate analgesia for the severity of pain present. Reassessment and regular documentation after initiating management allow for adjustments to be made where necessary.[6,7] Despite the availability of this wealth of knowledge, and tools with which to manage pain well in children, pain remains poorly understood, rarely assessed and inadequately treated in paediatric clinical practice worldwide. South Africa (SA) is no exception.
Studies conducted in Canada, the USA, New Zealand, Brazil and Australia have shown that documentation of pain scores is poor, with rates varying from 27% to 48%.[4,8-10] Nurses use and document pain scores more frequently than doctors, but analgesia is often given without the use of a pain score. Despite the existence and knowledge of protocols for pain management in the above study populations, analgesia was found to be inadequate or infrequent in many cases, resulting in breakthrough pain. Non-pharmacological pain relief was seldom recorded.[10]
Research on the subject on the African continent is limited, with only two published studies on the epidemiology of paediatric pain and its treatment in SA.[11,12] Both studies show that management could be improved, with similar results reported in Kenya.[2]
The barriers to adequate pain management are vast and often contextually unique. Some of the known barriers to appropriate pain management in paediatrics identified in the literature are difficulties with accurate assessment and quantification of pain in children; inadequate knowledge on pain management on the part of health professionals caring for children; the misconception that children, especially infants, lack the ability to feel or experience pain; failure of health professionals to assess for pain at all; the misconception that pain management is difficult; and fear of side-effects and addiction.[13] Health professionals' personal beliefs and attitudes towards pain can also interfere with its evaluation and management.[14] One barrier that is important in the SA setting is that identified by Nortjé and Albertyn:[15] the influence of culture on the expression and derived meaning of painful experience. They found that the expression of pain is not encouraged in SA Nguni and Sesotho cultures, particularly among men.[15] Traditional medicine is more accessible and is widely accepted as the first place to seek help, except for children, for whom Western medicine should be sought first.[15] The cultural meaning of pain (unappeased ancestors or witchcraft) may also limit its expression in the medical setting.[15] Poor pain management has both acute and chronic consequences. Early pain experiences have been linked to neurodevelopmental abnormalities, decreased cortical brain volumes and axonal disturbances, heightened behavioural responses, and an increased risk of anxiety-related psychiatric illness later in life.[16,17] Untreated or inadequately treated acute pain results in central sensitisation, which causes increased central nervous system responsiveness to painful and non-painful stimuli.[18] This process contributes to the development and maintenance of chronic pain. It is vital that pain is adequately managed to prevent these short- and long-term consequences.
This study aimed to review the assessment and management of pain in medical paediatric inpatients. The primary objective was to determine the proportion of children who receive analgesia where indicated, and the secondary objectives were to determine the prevalence of pain, at presentation and among admitted patients, to determine whether pain evaluations were done, and to determine whether pain was treated, and the adequacy of such treatment.
Methods
This study was conducted as a prospective cross-sectional survey. It consisted of a survey, patient evaluation for pain at the time of the survey, and a chart review. The study was conducted at Rahima Moosa Mother and Child Hospital (RMMCH) in Johannesburg, SA. This is a secondary academic hospital affiliated to the University of the Witwatersrand, which serves women and children. All medical patients aged <12 years admitted to the general paediatric medical department at RMMCH were included. Patients with surgical diagnoses and those admitted to the intensive care unit and the neonatal unit were excluded. Data were collected prospectively by convenience sampling in the paediatric wards at RMMCH on 3 days in September 2018 and 4 days in April 2019.
A target sample size of 64 patients was determined using Fisher's formula for prevalence studies.[19] The expected prevalence of pain was 78%, as taken from the study by Mate.[2] This study was selected because it is an African study, and at the time of protocol development there were no SA studies of pain prevalence among medical paediatric patients.
The tool used for data collection was a pain management and assessment audit form developed specifically for this study. It was designed based on the information required to achieve the objectives set out above. It consisted of three sections, one for demographic data, one for an interview of the patient, parent or caregiver, and finally one for review of the patient's file for evidence of pain assessment and adequacy of pain management. The adequacy of the analgesia was assessed using the prescription chart with reference to the level of pain at the time of the interview, as perceived by the caregiver or patient. Assessment of the prescription chart also included review for timed analgesia. Timed analgesia refers to analgesia prescribed to be given at a specific time interval as opposed to pro re nata (as needed).
The tool was written in English, but when interviewing either English or isiZulu was used, depending on which was most comfortable for and common to the interviewee and the data collector. The assistance of a translator was not needed for any of the caregivers interviewed. The objective assessment of pain at the time of data collection was done using the Neonatal/Infant Pain Scale (NIPS) and the revised Face, Legs, Activity, Cry, Consolability (R-FLACC) scale.
The NIPS tool is designed to assess six behavioural indicators of pain response in preterm (<37 weeks) and term neonates up to 6 weeks of age.[20] It is a non-invasive and validated measurement that assesses cry, motor activity, facial expression, state of arousal and breathing patterns, and is scored out of 7.[20,21] The patient is assessed as having no pain if the score is 0, mild pain with a score of 1 - 3, and moderate to severe pain with a score of >4.[20]
The R-FLACC scale uses five behavioural parameters to assess pain, each scored between 0 and 2, for children aged 2 months -18 years.[22,23] The five parameters are facial expression, leg movement activity, cry and consolability.[22] A total score of 0 means no pain, 1 - 3 is associated with mild pain, 4 - 7 is associated with moderate pain, and 8 - 10 is associated with severe pain.[23] This tool can be used to diagnose all kinds of acute pain.[22]
Both scales are well validated to accurately determine pain severity and are selected for ease of use and because they are the tools recommended by the clinical guideline for paediatric pain management at RMMCH (clinical guideline for paediatric pain management by A Bhettay, Department of Anaesthesia, RMMCH, 2016 - unpublished).
Self-report was used for patients aged >8 years, because this is the age at which self-report scales such as the numerical rating scale and the visual analogue scale are validated for use.[7] For the purposes of this review, the Wong-Baker FACES scale[24] was selected as it is already part of the pain guidelines that exist at RMMCH. The scale is currently validated for use from the age of 3 years. Children are asked to select from cartoon-type faces, designed to indicate escalating severities of pain, the one that best matches the pain they are experiencing.
For children aged <8 years, the parent or caregiver was asked their opinion of the presence of pain in the child at the time of the interview. If they considered the child to be in pain, they were asked to rate the pain as mild, moderate or severe.
The use of non-pharmacological methods for pain management was not included in the data collection tool because the survey did not include the observation of an interaction between health workers and patients for the evaluation of procedural pain, which is when such tools are likely to be used. These tools can be and often are applied without prescription, so the review of patient records would not be likely to give an accurate reflection of their use, or the lack thereof.
The study was approved by the Human Research Ethics Committee, University of the Witwatersrand (ref. no. M180116), prior to data collection. Participation was subject to the signing of an informed consent form by the parent or guardian.
Data were captured in REDCap (Research Electronic Data Capture, an online database manager hosted by the University of the Witwatersrand) and exported to Excel 2007 (Microsoft Corp., USA) for use. Analysis was done using Stata release 15 (StataCorp, USA). Categorical variables were expressed as frequencies and percentages, and continuous data were presented using means and standard deviations (SDs). Comparative analysis was done using x" tests of association for categorical variables, and odds ratios were calculated using logistic regression for significant variables. The level of significance was set at p<0.05.
Results
On all the days used to collect data, there was a total of 268 patients in the four paediatric wards at RMMCH. However, not all patients in the wards were eligible for interview, as they might have taken part in the study on the previous day. A total of 80 patients were approached; there were 5 refusals to participate, and 1 patient was excluded because they were >12 years old. Fig. 1 shows patient selection and participation.
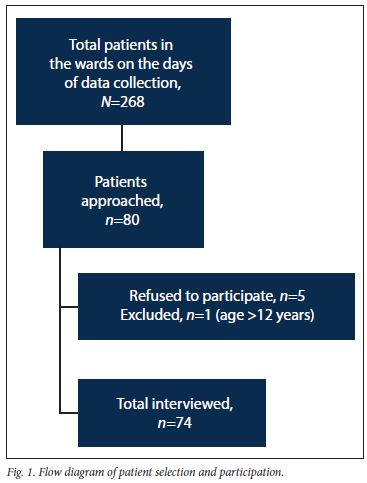
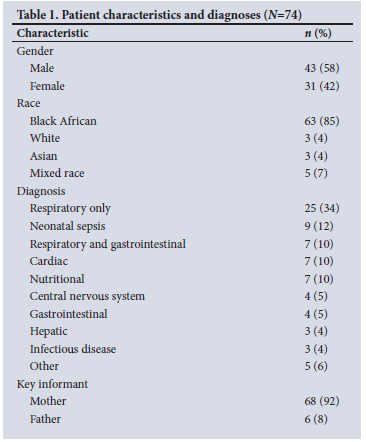
The complete data set consisted of a total of 74 patients. Their ages ranged from 3 days to 4 years and 3 months (mean (SD) 11 (12) months). Table 1 shows patient characteristics, demographics and diagnoses. All the participant surveys were conducted by caregiver report, as all the children were aged <8 years.
Pain epidemiology
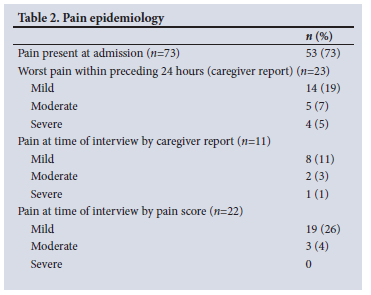
The prevalence of pain as part of the presenting complaint was 73% (95% confidence interval 60 - 82) by caregiver report. Age was not a significant determinant of pain (p=0.070).
The prevalence of pain later in the diagnosis by caregiver report was 31 % within the 24 hours preceding the interview. At the time of the interview, pain prevalence by caregiver report was 15%. When assessed using a pain score, it was found that the prevalence of pain at the time of interview was double that determined by caregivers, at 30% of the sample; however, this finding failed to meet statistical significance (p=0.051). There was no significant difference in pain score between the sexes (p=0.8). Table 2 shows the overall pain prevalence and severity at different stages of the admission.
Pain assessment
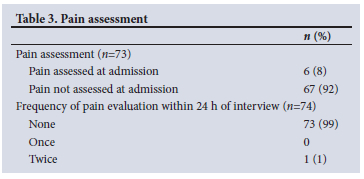
According to patient records, 6 of the 74 patients (8%) were assessed for pain at admission; of the 53 patients who reportedly had pain as part of their presenting complaint, only 4 had their pain evaluated in some way at admission. Subsequent pain evaluations were also very few, with only 1 patient having had two pain reviews documented within the 24 hours preceding the interview. The rest had no documented pain reviews in their patient files. Table 3 shows the frequency of pain assessment at admission and within the 24 hours preceding the interview.
Pain treatment and adequacy of treatment
Analgesia given was adequate for level of pain severity for only 7 (10%) of the 74 participants at some point in their care. Almost 60% of the patients reviewed had no analgesia during their admission up to the time of review. Almost a third were given paracetamol. Either the paracetamol was given for pyrexia and indicated as such, or the indication was not specified. Frequencies of pain treatment and its adequacy are set out in Table 4, and associations between pain and its management (using Fisher's exact test) are detailed in Table 5.
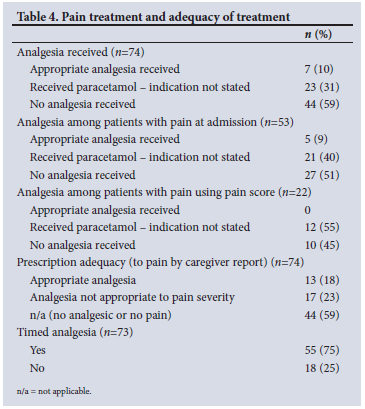
In Table 5, only 2 of the 8 parameters analysed show an association that is statistically significant. Those are the associations between assessment of pain at admission and the receipt of analgesia (p=0.006), and between the presence of pain before admission by parent report and the receipt of analgesia (p=0.021).
Discussion
The paediatric population at RMMCH at the time of the study had a prevalence of pain similar to findings in institutions around the world, and in other areas of SA. Pain was seldom assessed, validated pain scores were rarely used, and the result was poor pain management.
Pain prevalence at RMMCH at the time of admission mirrored that reported in the Red Cross War Memorial Children's Hospital trauma unit.[11] This was an important finding, because the patients reviewed in the present study all had medical illnesses, as opposed to surgical diagnoses. This finding challenges the general assumption made by healthcare workers that surgical patients experience more pain than medical patients do, as was shown by Velazquez Cardona et al.[12] and Cummings et al.[5] in their studies. It also highlights the resulting potential for increased vulnerability of medical patients to poor pain management.
The pain prevalence at admission in the present study was as high as found in studies from around the world from as far back as 1996. No improvement has been achieved in all these years of reviews, despite availability of guidelines.[35,9,11,12]
The declining prevalence of pain later in the admission, both by caregiver report and by pain score, can possibly be attributed to the use of paracetamol for pyrexia, or by routine prescription without actual assessment of a child's analgesic needs as based on pain severity. It may also have been due to the management and subsequent resolution of pathology.
At the time of the interview, the prevalence of pain by caregiver report was half of that found by pain score. Other studies have found better agreement between caregiver reports and objective pain scores.[25,26] Although not specifically evaluated in this study this disparity in reported pain between caregiver assessment and pain score could be explained by the cultural nuances of our diverse society, by language differences, and by historical power dynamics associated with SAs political past.[15] These potential influences require further study, and awareness on the part of clinicians.
Pain was rarely assessed at RMMCH during this study. The best opportunity for pain assessment was found to be at admission. Pain assessments during the days following admission rarely occurred. Investigational and therapeutic procedures carried out during a hospital admission are known to be painful. Although not specifically investigated in this study, the absence of subsequent pain evaluations exposed a period of risk where procedural pain was unlikely to be addressed.
Unsurprisingly, the low rate of pain evaluation correlated with inadequate analgesic use and pain management. More than half of the patients did not receive any analgesia despite its being indicated. Most patients were inappropriately given single-agent analgesia (paracetamol), even when moderate or severe pain necessitated stronger agents and a multimodal approach. Pain management should consist of four basic steps: pain assessment, intervention, reassessment of treatment adequacy and for side-effects, and ongoing management. Optimal pain control is achieved by using an interdisciplinary approach utilising non-pharmacological pain management strategies and multimodal analgesia. Mild pain is treated with non-pharmacological strategies and simple analgesics such as paracetamol and non-steroidal anti-inflammatory drugs. Moderate pain should be treated with the addition of a weak opioid. Severe pain requires the use of intravenous strong opioids.[27] Adjuvant analgesic agents should be utilised where appropriate.
Of the patients who had pain at admission, only 7% received analgesia appropriate for their pain severity. When paracetamol is included, the odds of receiving analgesia when pain was present at admission was 3.85 (p=0.021); however, when paracetamol was removed, there was no significant association between the presence of pain at admission and the receipt of analgesia. It is likely that many patients benefited from the routine use of paracetamol for fever without formal pain evaluation with a validated pain score.
There was no statistically significant association between the presence of pain by caregiver report and the receipt of analgesia. However, when pain was clinically evaluated, there was statistically and clinically significant evidence that analgesia was more likely to be given.
The study population did not include any child aged >8 years. Therefore, none of the study participants was the primary informant. The study relied on caregiver assessments and pain scores without the use of self-report, which is the gold standard for pain assessment. This study population reflects that of RMMCH and therefore the reality of pain assessment and management in this institution.
The barriers to pain assessment and management specific to RMMCH should be explored in future studies. If identified, they could provide useful insight and a great starting point towards quality improvement.
This study enriches the currently sparse body of knowledge about the epidemiology of paediatric pain and its management in SA. It provides SA paediatric clinicians of all disciplines insight into their own behaviour, and an opportunity for a deliberate effort towards improvement.
Study limitations
While enquiry into the presence of pain at admission took place, the severity of that pain was not documented, making comparison of progression difficult.
The exact analgesics prescribed were not recorded at the time of data collection. Only data on the use of paracetamol for pyrexia (as indicated in the clinical notes), or without a written indication, were noted. This was an unfortunate error in study design, which meant that a pain management index (PMI) could not be calculated. A PMI could have made analysis of adequacy of care more accurate. The PMI is a score, ranging from 3- to 3+, used to quantify the pharmacological management of pain. Pain severity is subtracted from the analgesic used.[27]
The study was conducted in a single centre with a relatively small sample size.
The study design allowed for the patient to be the primary respondent only if >8 years of age, because that was the age from which assent was to be acquired from the child, and the RMMCH paediatric pain protocol was designed for self-report at the age of >7 years. Therefore, none of the pain evaluations was by self-report.
Conclusion
Pain in the paediatric population at RMMCH was found to be common, and its management was poor in all four domains: assessment, intervention, reassessment and ongoing management. This is despite the wealth of knowledge, tools and guidelines on the management of pain in the paediatric population and the presence of a pain management guide written specifically for use at RMMCH. This finding is not unique to this hospital, and the situation is likely to be similar in many SA healthcare institutions.
These findings suggest that more than a written protocol is needed to improve pain management.
Recommendations
Training of medical staff on pain assessment and management may raise awareness. The training should begin with consultants, as they are the drivers of behaviour among junior staff, and because they remain constant in an academic environment with a high trainee doctor turnover. This high turnover would necessitate regular training every few months. Nurses, who spend the most time with patients, should be placed at the forefront for training opportunities.
Visible pain assessment posters may prompt use by health professionals and may also prompt caregivers to speak up when they feel that their childs pain is not being managed. Perhaps the inclusion of a section for pain score evaluation in both the nurses' triage form and the doctors' admission file template would encourage accurate and regular documentation of assessments, interventions, management and reassessments.
A policy that allows nurses to initiate pain management by a predetermined algorithm, both at admission triage and in the wards while they await review by a doctor, could minimise a child's distress while waiting to be seen in busy academic and public hospitals, where waiting times are often long.
Declaration. The research for this study was done in partial fulfilment of the requirements for LMNM's MMed (Paediatrics and Child Health) degree at the University of the Witwatersrand.
Acknowledgements. None.
Author contributions. LMNM: primary investigator and author; AB: co-author and thesis supervisor, involved in study design and manuscript review; RB: manuscript review; DD: thesis supervisor, involved in manuscript review.
Funding. None.
Conflicts of interest. None.
References
1. Singh H, Banipal RPS, Singh B. Assessment of adequacy of pain management and analgesic use in patients with advanced cancer using the Brief Pain Inventory and Pain Management Index Calculation J Glob Oncol 2016;3(3):235-241. https://doi.org/10.1200/jgo.2016.004663 [ Links ]
2. Mate JW. Prevalence, severity and initial management of pain among children admitted in Kenyatta national hospital general paediatric wards. MMed (Paediatrics and Child Health) dissertation. Nairobi Kenya. University of Nairobi, 2014. http://erepository.uonbi.ac.ke/handle/l1295/77865 (accessed 8 July 2022). [ Links ]
3. Naughton KN. The combined use of sucrose and nonnutritive sucking for procedural pain in both term and preterm neonates. An integrative review of the literature. Adv Neonatal Care 2013;13(1):9-19. https://doi.org/10.1097/anc.0b013e31827ed9d3 [ Links ]
4. Taylor EM, Boyer K, Campbell FA. Pain in hospitalised children. A prospective cross-sectional survey of pain prevalence, intensity, assessment and management in a Canadian pediatric teaching hospital. Pain Res Manag 2008;13(1):25-32. https://doi.org/10.1155/2008/478102 [ Links ]
5. Cummings EA, Reid GJ, Finley AG, McGrath PJ, Ritchie JA. Prevalence and source of pain in pediatric inpatients. Pain 1996;68(l):25-31. https://doi.org/10.1016/s0304-3959(96)03163-6 [ Links ]
6. Fink R. Pain assessment. The cornerstone to optimal pain management. Proc (Bayl Univ Med Cent) 2000;13(3):236-239. https://doi.org/10.1080/08998280.2000.11927681 [ Links ]
7. World Health Organization. Persisting pain in children package. WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses. WHO, 2012. https://apps.who.int/iris/handle/10665/44540 (accessed 5 February 2017). [ Links ]
8. Kozlowski LJ, Kost-Byerly S, Colantuoni E, et al. Pain prevalence, intensity, assessment and management in a hospitalized pediatric population. Pain Manag Nurs 2014;15(1):22-35. https://doi.org/10.1016/j.pmn.2012.04.003 [ Links ]
9. Herd DW, Babl FE, Giihotra Y, Huckson S, PREDICT group. Pain management practices in paediatric emergency departments in Australia and New Zealand. A clinical and organizational audit by National Health and Medical Research Councils National Institute of Clinical Studies and Paediatric Research in Emergency Departments International Collaborative. Emerg Med Australas 2009;21(3):210-221. https://doi.org/10.1111/j.1742-6723.2009.01184.x [ Links ]
10. Linhares MBM, Doca FNP, Martinez FE, et al. Pediatric pain. Prevalence, assessment, and management in a teaching hospital. Braz J Med Biol Res 2012;45(12):1287-1294. https://doi.org/10.1590/s0100-879x2012007500147 [ Links ]
11. Thiadens T, Vervat E, Albertyn R, van Dijk M, van As AB. Evaluation of pain incidence and pain management in a South African paediatric trauma unit. S Afr Med J 2011;101(8):533-536. https://doi.10.7196/SAMJ.4456 [ Links ]
12. Velazquez Cardona C, Rajah C, Mzoneli YN, et al. An audit of paediatric pain prevalence, intensity, and treatment at a South African tertiary hospital. Pain Rep 2019;4(6):e789. https://doi.org/10.1097/pr9.0000000000000789 [ Links ]
13. American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health, Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 2001;108(3):793-797. https://doi.org/10.1542/peds.108.3.793 [ Links ]
14. Twycross A, Dowden S, Stinson J, eds. Managing Pain in Children. A Clinical Guide for Nurses and Healthcare Professionals. Chichester, UK. John Wiley & Sons, 2013:274-275. [ Links ]
15. Nortie N, Albertyn R. The cultural language of pain. A South African study. S Afr Fam Pract 2015;57(1):24-27. https://doi.org/10.1080/20786190.2014.977034 [ Links ]
16. Grunau R. Early pain in preterm infants. Clin Perinatol 2002;29(3):373-394. http://doi.org/10.1016/s0095-5108(02)00012-x [ Links ]
17. Ranger M, Grunau RE. Early repetitive pain in preterm infants in relation to the developing brain. Pain Manag 2014;4(1):57-67. https://doi.org/10.2217/pmt.l3.61 [ Links ]
18. Latremoliere A, Woolf CJ. Central sensitization. A generator of pain hypersensitivity by central neural plasticity. J Pain 2009;10(9):895-926. https://doi.org/10.1016/j.jpain.2009.06.012 [ Links ]
19. Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci 2006;1:9-14. [ Links ]
20. Galio A-M. The fifth vital sign. Implementation of the Neonatal Infant Pain Scale. J Obstet Gynecol Neonatal Nurs 2003;32(2):199-206. https://doi.org/10.1177/0884217503251745 [ Links ]
21. Marin Gabriel MA, del Rey Hurtado de Mendoza B, Jimenez Figueroa L, et aL Analgesia with breastfeeding in addition to skin-to-skin contact during heel prick. Arch Dis Child Fetal Neonatal Ed 2013;98(6):F499-F503. https://doi.org/10.1136/archdischild-2012-302921 [ Links ]
22. Manworren RC, Hynan LS. Clinical validation of FLACC. Preverbal patient pain scale. Pediatr Nurs 2003;29(2):140-146. [ Links ]
23. Merkel S, Voepel-Lewis T, Malviya S. Pain assessment in infants and young children. The FLACC Scale. Am J Nurs 2002;102(10):55-58. https://doi.org/10.1097/00000446-200210000-00024 [ Links ]
24. Wong-Baker FACES Foundation. Wong-Baker FACES history. 2020. https://wongbakerfaces.org/us/wong-baker-faces-history/ (accessed 13 September 2020). [ Links ]
25. Singer AJ, Gulia J, Thode HC Jr. Parents and practitioners are poor judges of young chiidrens pain severity. Acad Emerg Med 2002;9(6):609-612. https://doi.org/10.1111/j.l553-2712.2002.tb02298.x [ Links ]
26. Brudvik C, Moutte S-D, Baste V, Morken T. A comparison of pain assessment by physicians, parents and children in an outpatient setting. Emerg Med J 2016;34(3):138-144. https://doi.org/10.1136/emermed-2016-205825 [ Links ]
27. South African Society of Anaesthesiologists. Guidelines for the management of acute pain in specific scenarios 2022. South Afr J Anaesth Analg 2022;28(1 Suppl 1):S1-S226. https://sasaapi.sasaweb.com/Document/AcutePainGuidelines2022_637814616383629668.pdf (accessed 8 July 2022). [ Links ]
 Correspondence:
Correspondence:
L M N Mabaso
lmnmabasoll@gmail.com
Accepted 22 April 2022














