Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 no.5 Pretoria may. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i5.16366
RESEARCH
The profile of patients presenting with intentional self-poisoning to the Charlotte Maxeke Johannesburg Academic Hospital emergency department, South Africa
A E LaherI; F MotaraII; R GihwalaIII; M MoollaIV
IMMed (Emerg Med), PhD ; Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, MFamMed; Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMB ChB, MMed (Emerg Med); Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVMB BCh, EDIC Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. With 23.5 suicide-related deaths per 100 000 population, South Africa (SA) has the eighth-highest age-standardised suicide rate in the world. Intentional self-poisoning is associated with significant morbidity, mortality and cost. In SA, self-poisoning is the leading method of suicide in females and the second leading method in males.
OBJECTIVES. To determine the profile of patients presenting with intentional self-poisoning to the Charlotte Maxeke Johannesburg Academic Hospital emergency department.
METHODS. The study was a cross-sectional, retrospective audit of the medical records of patients who presented over a 12-month period with intentional self-poisoning.
RESULTS. Of the 288 patients included, 62.8% were female, 62.1% were aged 18 - 30 years, 22.2% were foreign nationals, 88.9% were single, 62.8% were unemployed, 82.3% reported that the episode was precipitated by an acute stressful event, 5.6% required intensive care unit (ICU) admission, and 4.5% died prior to hospital discharge. Organophosphate/carbamate pesticide ingestion was the most common method of self-poisoning (25.3%) and was responsible for the majority of ICU admissions (81.3%), cases requiring hospitalisation for >6 days (56.5%) and deaths (69.2%).
CONCLUSION. A large proportion of patients were female, 18 - 30 years of age, single, unemployed, and reported an acute stressful event as a precipitant. Organophosphate/carbamate pesticide ingestion was the most common method of self-poisoning and accounted for the majority of deaths and ICU admissions. Nationwide efforts should be aimed at enhancing awareness and implementing strategies to identify those at increased risk of suicidal behaviour.
In 2019, suicide accounted for ~703 000 deaths (1.3% of all-cause mortality) around the globe, with the African continent accounting for the highest suicide death rate (11.2 per 100 000 population). Overall, there were more deaths from suicidal behaviour than from malaria, HIV/AIDS, breast cancer, war or homicide. With 23.5 suicide-related deaths per 100 000 population, South Africa (SA) has the eighth-highest age-standardised suicide rate in the world.[1] In 2015, there were 23 recorded cases of suicide and 230 serious attempts at suicide per day in SA.[2]
The global prevalence of non-fatal suicidal behaviour is estimated to be 10 - 40 times higher than that of (fatal) suicide.[3,4] While physical methods such as hanging and firearm-related injuries are more commonly employed methods of suicidal behaviour in higher-income countries, intentional self-poisoning is the most common method employed in lower-income countries.[5,6] Risk factors for suicidal behaviour include relationship problems, family conflict, unwanted pregnancy, unemployment, type of occupation, family history of suicide, drug and alcohol abuse, mood disorders and other psychiatric illnesses, mental illness, chronic illnesses, and being diagnosed with serious medical conditions such as cancer and heart disease.[7,8]
Intentional self-poisoning is the deliberate ingestion of a substance for the purpose of committing suicide, attention-seeking behaviour or expressing distress, or as a means of seeking revenge.[5] In SA, nonfatal intentional self-poisoning accounts for ~90% of cases of non-fatal suicidal behaviour and is associated with significant morbidity and mortality.[9] A study conducted in Eastern Cape Province reported
that drug overdoses were responsible for an average of 29 intensive care unit (ICU) admissions every month.[10] Studies have shown that among patients presenting to SA hospitals with a history of intentional self-poisoning, <5% die prior to hospital discharge.[11-13] However, this figure does not account for deaths occurring prior to hospital presentation. A study that analysed trends in suicide mortality in SA between 1997 and 2016 reported that there were 8 573 recorded suicides during this period, with poisoning the leading method of suicide in females (38.8% of cases) and the second leading method in males (15.2%).[14]
Intentional self-poisoning is also associated with a substantial economic burden and significant healthcare costs. A study in Turkey reported that the mean (standard deviation) cost of managing a patient with intentional self-poisoning was USD144.06 (90.83) for their entire duration of hospital admission.[15] Similarly, a study in the UK reported that the estimated annual hospital cost of intentional self-poisoning was GBP56 million.[16] A study at Pelonomi Hospital in Free State Province, SA, estimated that the approximate monthly cost associated with managing all cases of intentional self-poisoning was ZAR50 000.[17
The risk of suicide following an episode of non-fatal intentional self-poisoning is high. In a Canadian population-based cohort study that comprised 65 784 patients who were discharged after a first episode of self-poisoning, 4 176 died during a median follow-up period of 5.3 years, of whom 976 (23.4%) had committed suicide. Relative to controls, there was a significantly increased risk of suicide following an episode of self-poisoning (hazard ratio 41.96; 95% confidence interval 27.75 - 63.44), corresponding to a suicide rate of 278 v. 7 per 100 000 person-years, respectively.[18]
Objectives
There is a paucity of recent data pertaining to intentional self-poisoning in the Johannesburg region of SA. The objective of this study was therefore to determine the profile of patients presenting with intentional self-poisoning to the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) emergency department (ED).
Methods
The study was a cross-sectional, retrospective review of the medical records of patients who presented to the CMJAH adult medical ED over a 12-month period (1 November 2016 - 31 October 2017) with an episode of intentional self-poisoning. CMJAH has ~1 000 beds and serves the Johannesburg inner city and surrounding suburban areas. Approximately 3 500 patients attend the ED every month[19]Permission to conduct the study was obtained from the hospital manager, and ethics clearance was granted by the Human Research Ethics Committee of the University of the Witwatersrand (ref. no. M171032).
For the purpose of this study, intentional self-poisoning was defined as the deliberate ingestion of either a poisonous substance or prescription medication in excess of the prescribed dose. Adverse events after an episode of self-poisoning were defined as in-hospital mortality, ICU admission or duration of hospital admission >6 days. As per departmental protocol, all patients presenting with an episode of intentional self-poisoning, including those who are physiologically stable, at minimum require overnight admission and may only be discharged the following morning if they are clinically stable and have undergone a psychological assessment.
The CMJAH adult medical ED registers were reviewed to identify the file numbers of patients presenting with a history of intentional self-poisoning over the data collection period. Thereafter, the medical records of these patients were obtained from the hospital records department. Where medical records were missing at the medical records department, the nursing manager at the ward where the patient was admitted was also approached in an attempt to try to locate the missing records. Patients for whom medical records could not be obtained or accessed were excluded from the study.
Relevant data from each of the available medical records were thereafter entered into individual study data collection sheets. Collected data included sex, age, nationality, marital status, employment, psychiatric history, Glasgow Coma Scale (GCS) score at ED presentation, duration of hospital admission, ICU admission, in-hospital mortality and substance ingested.
Conflicting data entries were resolved after consulting with the attending clinician (where available) or after consensus was reached among the study investigators. Inter-rater reliability was assessed by an independent researcher with experience in the methods of data collection and who was blinded to the study objectives. Data extracted from a random sample of 18 medical records were compared with data extracted by the primary investigator. Cohen's kappa coefficient (κ) was 0.83, indicating that the degree of inter-rater reliability was acceptable.
Data were thereafter captured and analysed in Excel version 16.52 (Microsoft Corp., USA). Since all the data were categorical in nature, findings were described using frequencies and percentages. Reporting of study findings conformed to STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.[20]
Results
Upon review of the relevant ED registers, the details of 356 patients with a presenting diagnosis of drug or substance poisoning were identified. The medical records of 36 of these patients could not be obtained. Upon review of the 320 available records, the final diagnosis was found not to be 'intentional self-poisoning' in 32 records. After exclusion, a total of 288 patients, equating to a frequency of 0.79 presentations per day, were therefore included in the final study sample.
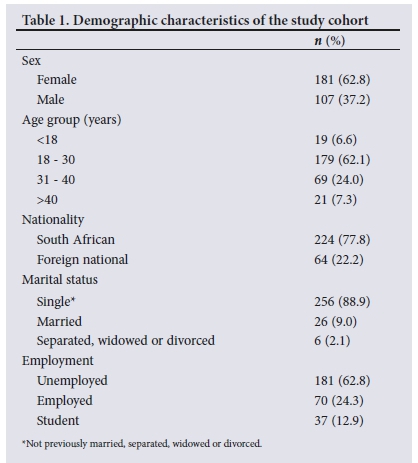
Demographic characteristics of the study cohort are presented in Table 1. Most of the patients were female (n=181; 62.8%), 18 - 30 years old (n=179; 62.1%), single (n=256; 88.9%) and unemployed (n=181; 62.8%). Foreign nationals comprised approximately one-fifth of the patients in the study (n=64; 22.2%).
Clinical characteristics of the study cohort are presented in Table 2. Of note, 237 patients (82.3%) reported that the suicidal attempt was precipitated by an acute stressful event, 58 (20.1%) had previously attempted suicide, 58 (20.1%) presented with a GCS score <15, 16 (5.6%) required ICU admission, and 13 (4.5%) died prior to hospital discharge. All 288 patients (100%) were admitted, 111 (38.5%) for a duration of <1 day.
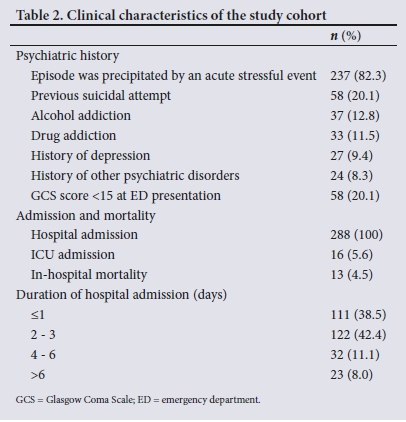
Fig. 1 presents the frequency of each of the substances that were ingested by the study cohort. Organophosphate/carbamate pesticide ingestion (n=73; 25.3%), followed by non-steroidal anti-inflammatory drug overdose (n=40; 13.9%) and household chemical ingestion (n=32; 11.1%) were the most common methods utilised. Polypharmacy ingestion was documented in 61 patients (21.2%).
The breakdown of substances ingested and their frequency of adverse events (in-hospital mortality, ICU admission and hospital admission >6 days) is presented in Table 3. Of note, the majority of adverse events were secondary to organophosphate/carbamate pesticide ingestion.
Discussion
This study comprised 288 patients who had presented to the CMJAH ED over a 1-year period (1 November 2016 - 31 October 2017; 0.79 cases per day) with a history of intentional self-poisoning. In comparison, Laubscher and Van Rooyen[11] reported that 196 patients presented to Paarl Hospital in Western Cape Province over a 6-month period (1 July 2005 - 31 December 2005), averaging 1.13 cases per day, while Du Toit et al.[21] reported that 234 patients presented to Pelonomi Hospital in Bloemfontein over a 1-year period (1 May 2005 - 30 April 2006), averaging 0.64 cases per day. A study by Benedict et al.,[12]also conducted at Pelonomi Hospital, reported that 260 patients presented over an 18-month period (1 January 2010 - 30 June 2011), averaging 0.47 cases per day. In a study by Van Hoving et al.[13]conducted at Khayelitsha Hospital in Western Cape, 192 patients presented over a 6-month period (1 November 2014 -30 April 2015), averaging 1.05 cases per day. Except for the study by Laubscher and Van Rooyen,[11] who only included patients with an overdose of prescription drugs, the remaining studies included all patients with a history of intentional self-poisoning. It must be noted that the number of cases reported at each of the above facilities is dependent on various factors, including the capacity and capability of surrounding healthcare facilities. The reported figures may therefore not necessarily reflect the actual extent and profile of intentional self-poisoning in each of these regions.
The higher incidence of intentional self-poisoning among females than males in the present study (62.8%) is in keeping with studies conducted both locally and internationally. In studies in SA, females comprised 73.5%,[11] 68.9%,[21] 66.0%[12] and 68.8%[13] of patients. In Australia, Buykx et al.[22]found that 63.6% of patients were female, as opposed to 78% and 86.1% reported by Zaidan et al.[23] in Oman and Donovan et al.[24] in the UK, respectively. In general, males have a tendency to employ more violent methods of self-harm such as hanging and have higher rates of fatal suicide compared with females, who are more likely to resort to less violent methods such as self-poisoning.[21,25,26] Prevention strategies such as self-coping mechanisms and behavioural therapies should therefore be targeted at both males and females.
The age group 18 - 30 years accounted for the highest incidence of intentional self-poisoning in the present study. These results are consistent with both of the studies conducted at Pelonomi Hospital,[12,21-as well as the study conducted at Khayelitsha Hospital.[13] In contrast, the study conducted at Paarl Hospital found that the highest incidence was in the 10 - 19-year age group (29.4%), followed by the 30 - 39-year (27.5%) and 20 - 29-year (25.6%) age groups.[11]
Since foreign nationals constitute ~7% of people living in SA,[27] the percentage of foreign nationals presenting with intentional self-poisoning in this study (22.2%) is disproportionately high. Similarly, a European study of 27 048 patients also reported that rates of attempted suicide were higher in immigrant populations compared with the host populations.[28] Language barriers, separation from family with concerns about their wellbeing, loss of status, loss of social network and acculturation were identified as triggers and risk factors for the higher rates of suicidal behaviour among immigrant populations.[29]
Since approximately half of the SA population is classified as single,[30] the percentage of patients in this study who were single (88.9%) is disproportionately high. In comparison, two other SA-based studies reported that 38.4%[21] and 88.0%[12] of patients were single. A study conducted in Zambia noted that 58.7% of parasuicide patients were married,[31] while a study conducted in Spain noted that 31.8% of patients were single.[32] Reasons for the large variation in marital status between these studies are unclear.
The unemployment rate of patients in the present study was 62.8%. In comparison, studies in Spain,[32] South Korea[33] and Australia[34] reported unemployment rates of 59.1%, 41.0% and 20.3%, respectively. In other SA-based studies where employment status was reported, 53.7%[11] and 65.6%[12] of patients were reported as unemployed. It is therefore of importance to target the unemployed population when providing preventive strategies.
Over 80% of the patients in the present study reported that the current episode was precipitated by an acute stressful event, 24.3% reported comorbid alcohol/drug addiction, and 17.7% reported a history of depression or another psychiatric disorder. In a study in China, 40% of patients with non-fatal suicidal behaviour also had a concurrent diagnosable mental illness, while 35% indicated that they first considered harming themselves within 10 minutes before the attempt.[35] Ki et al.[33] reported that anxiety or depression was present in 13.3% of patients and a drinking problem in 26.1%, while Du Toit et al.[21] reported that a psychiatric disorder was present in 22.1% of patients. Benedict et al.[12] found that among patients who provided a reason for suicidal behaviour, 49.4% reported that troubled relationships was the primary reason.[12] A study conducted in Sri Lanka also reported that interpersonal conflict was a common trigger of suicidal behaviour.[36]
In the present study, organophosphate/carbamate pesticides (25.3%), non-steroidal anti-inflammatory drugs (13.9%) and household chemicals (11.1%) were the most frequently ingested substances. In comparison, in other SA-based studies, Laubscher and Van Rooyen[11] reported that the most frequently ingested substances were tricyclic antidepressants (20.4%) and paracetamol (20.4%), Du Toit et al.[21] reported that they were antidepressants (19.7%), household chemicals (12.0%) and analgesics (8.2%), Benedict et al.[12] reported that they were paracetamol (21.7%), household chemicals (19.3%) and HIV medication (9.9%), and Van Hoving et al.[13] reported that they were paracetamol (25.0%) and cardiovascular drugs (22.9%). Polypharmacy ingestion was documented in 21.2% of cases in the present study, compared with 42.3% reported by Laubscher and Van Rooyen,[11] 40.1% reported by Benedict et al.[12] and 43.8% reported by Van Hoving et al.[13] Pesticide ingestion has been reported as the most frequent method of intentional self-poisoning in the Asia-Pacific region, accounting for ~300 000 annual deaths.[37] In studies from other African countries such as Ethiopia, Burkina Faso and Zambia, pesticide ingestion accounted for between 22% and 42% of acute poisoning presentations.[38]
In the present study, 5.6% of patients were admitted to the ICU, while 4.5% died prior to hospital discharge. In comparison, in three other SA-based studies, 8.5%,[11] 2.5%[12] and 7.3%[13] of patients were admitted to the ICU, while 0%,[11] 1.0%[12] and 2.0%[13] of patients died. However, none of these studies, including our study, had accounted for mortality prior to hospital arrival. A study showed that intentional self-poisoning was the leading cause of suicidal mortality in women in SA and the second leading cause of suicidal mortality in men.[14]
Study limitations
There are some limitations to this study. Firstly, it was a single-centre study, so our findings may not be applicable to other facilities, as patterns of suicidal behaviour may differ between regions. Secondly, the study was conducted at a tertiary-level hospital ED, and we did not account for milder cases that may not have been referred to our facility. Thirdly, we did not account for cases that were self-managed at home or for people who may have died out of the hospital. Our findings are therefore probably an underestimation of the actual extent and outcomes of intentional self-poisoning in the region.
Conclusion
The majority of patients in our study were female, 18 - 30 years old, single, unemployed, and reported that the suicidal attempt was precipitated by an acute stressful event. A substantial proportion of patients were foreign nationals. Organophosphate/carbamate pesticide ingestion was the most common method of self-poisoning and accounted for the majority of deaths and ICU admissions. Nationwide efforts should be aimed at enhancing awareness, implementing strategies to identify those who are at high risk of suicidal behaviour, and strengthening support structures.
Declaration. None.
Acknowledgements. We thank Drs Caroline Buckland, Ektha Govind, Nicole Maclean, Joshua Masojada, Palesa Mokoena, Putso Motubatse, Sammy Nganga, Tumelo Phasha, Ronelle Rajin, Tasnim Sallie, Shelby Smith, Chwayita Tenza and Gabriel Zollman for their assistance with data collection.
Author contributions. AEL: primary author, study design, data collection, data analysis, manuscript write-up and approval of the final manuscript. FM, RG and MM: assisted with study design, data analysis, interpretation of results, editing of the manuscript and approval of the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. World Health Organization. Suicide worldwide in 2019: Global Health Estimates. 16 June 2021. https://www.who.int/publications/i/item/9789240026643 (accessed 5 December 2021). [ Links ]
2. Health24. Why are people in SA trying to kill themselves? 5 January 2016. https://www.news24.com/health24/Mental-Health/Mental-health-in-SA/why-are-people-in-sa-trying-to-kill-themselves-20160105 (accessed 5 December 2021). [ Links ]
3. Schlebusch L. Suicidal Behaviour in South Africa. Pietermaritzburg: University of KwaZulu-Natal Press, 2005. [ Links ]
4. World Health Organization. Figures and facts about suicide. 1999. http://apps.who.int/iris/bitstream/handle/10665/66097/WHO_MNH_MBD_99.1.pdf;jsessionid =ABA08DE39685CA0B02382630062722 BB?sequence=1 (accessed 5 December 2021). [ Links ]
5. Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ 2004;328(7430):42. https://doi.org/10.1136/bmj.328.7430.42 [ Links ]
6. Quarshie EN-B, Waterman MG, House AO. Self-harm with suicidal and non-suicidal intent in young people in sub-Saharan Africa: A systematic review. BMC Psychiatry 2020;20:234. https://doi.org/10.1186/s12888-020-02587-z [ Links ]
7. Joe S, Stein DJ, Seedat S, Herman A, Williams DR. Non-fatal suicidal behavior among South Africans. Soc Psychiatry Psychiatr Epidemiol 2008;43(6):454-461. https://doi.org/10.1007/s00127-008-0348-7 [ Links ]
8. Mars B, Burrows S, Hjelmeland H, Gunnell D. Suicidal behaviour across the African continent: A review of the literature. BMC Public Health 2014;14:606. https://doi.org/10.1186/1471-2458-14-606 [ Links ]
9. Schlebusch L. Suicide prevention: A proposed national strategy for South Africa. Afr J Psychiatry 2012;15(6):436-440. https://doi.org/10.4314/ajpsy.v15i6.56 [ Links ]
10. Rowe K. The burden of drug overdose on critical care units in East London, South Africa. S Afr Med J 2016;106(3):227-228. https://doi.org/10.7196/SAMJ.2016.v106i3.9933 [ Links ]
11. Laubscher C, van Rooyen E. The profile of the overdose patient presenting at Paarl Hospital Emergency Department. S Afr Fam Pract 2007;49(2):16. [ Links ]
12. Benedict M, van Loggerenberg C, Steinberg W The profile of deliberate self-poisoning cases presenting at the emergency department of Pelonomi Regional Hospital, Bloemfontein. S Afr Fam Pract 2019;61(1):11-17. https://doi.org/10.4102/safp.v61i1.5057 [ Links ]
13. Van Hoving DJ, Hunter LD, Gerber RJ, Lategan HJ, Marks CJ. The burden of intentional self-poisoning on a district-level public hospital in Cape Town, South Africa. Afr J Emerg Med 2018;8(3):79-83. https://doi.org/10.1016/j.afjem.2018.03.002 [ Links ]
14. Kootbodien T, Naicker N, Wilson KS, Ramesar R, London L. Trends in suicide mortality in South Africa, 1997 to 2016. Int J Environ Res Public Health 2020;17(6):1850. https://doi.org/10.3390/ijerph17061850 [ Links ]
15. Serinken M, Karcioglu O, Sengul C, Turkcuer I, Keysan MK. Hospital costs of managing deliberate self- poisoning in Turkey. Med Sci Monit 2008;14(3):CR152-8. [ Links ]
16. Kapur N, House A, Dodgson K, et al. Management and costs of deliberate self-poisoning in the general hospital: A multi-centre study. J Ment Health 2002;11(2):223-230. https://doi.org/10.1080/1-09638230020023606 [ Links ]
17. Benedict MA, Mofolo N, Adefuye AO. The economic burden of deliberate self-poisoning: Insight from a tertiary hospital in the Free State Province, South Africa. Pan Afr Med J 2020;36:35. https://doi.org/10.11604/pamj.2020.36.35.22346 [ Links ]
18. Finkelstein Y, Macdonald EM, Hollands S, et al. Risk of suicide following deliberate self-poisoning. JAMA Psychiatry 2015;72(6):570-575. https://doi.org/10.1001/jamapsychiatry.2014.3188 [ Links ]
19. Etlouba Y, Laher A, Motara F, Moolla M, Ariefdien N. First presentation with psychotic symptoms to the emergency department. J Emerg Med 2018;55(1):78-86. https://doi.org/10.1016/j.jemermed.2018.04.014 [ Links ]
20. Von Elm E, Altman DG, Egger M, Pocock SJ, G0tzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007;335:806. https://doi.org/10.1136/bmj.39335.541782.AD [ Links ]
21. Du Toit EH, Kruger JM, Swiegers SM, et al. The profile analysis of attempted-suicide patients referred to Pelonomi Hospital for psychological evaluation and treatment from 1 May 2005 to 30 April 2006. S Afr J Psychiatry 2008;14(1):a40. https://doi.org/10.4102/sajpsychiatry.v14i1.40 [ Links ]
22. Buykx P, Dietze P, Ritter A, Loxley W. Characteristics of medication overdose presentations to the ED: How do they differ from illicit drug overdose and self-harm cases? Emerg Med J 2010;27(7):499-503. https://doi.org/10.1136/emj.2009.075549 [ Links ]
23. Zaidan ZAJ, Burke DT, Dorvlo ASS, et al Deliberate self-poisoning in Oman. Trop Med Int Health 2002;7(6):549-556. https://doi.org/10.1046/j.1365-3156.2002.00887.x [ Links ]
24. Donovan S, Clayton A, Beeharry M, et al. Deliberate self-harm and antidepressant drugs. Br J Psychiatry 2000;177(6):551-556. https://doi.org/10.1192/bjp.177.6.551 [ Links ]
25. Anthony L, Kulkarni C. Patterns of poisoning and drug overdosage and their outcome among in-patients admitted to the emergency medicine department of a tertiary care hospital. Indian J Crit Care Med 2012;16(3):130-135. https://doi.org/10.4103/0972-5229.102070 [ Links ]
26. Doak MW, Nixon AC, Lupton DJ, Waring WS. Self-poisoning in older adults: Patterns of drug ingestion and clinical outcomes. Age Ageing 2009;38(4):407-411. https://doi.org/10.1093/ageing/alp046 [ Links ]
27. Wikipedia. Immigration to South Africa. 2021. https://en.wikipedia.org/wiki/Immigration_to_South_Africa (accessed 24 December 2021). [ Links ]
28. Bursztein Lipsicas C, Mäkinen IH, Apter A, et al Attempted suicide among immigrants in European countries: An international perspective. Soc Psychiatry Psychiatr Epidemiol 2012;47(2):241-251. https://doi.org/10.1007/s00127-010-0336-6 [ Links ]
29. Forte A, Trobia F, Gualtieri F, et al. Suicide risk among immigrants and ethnic minorities: A literature overview. Int J Environ Res Public Health 2018;15(7):1438. https://doi.org/10.3390/ijerph15071438 [ Links ]
30. Statista. Gender distribution of the South African population in 2019, by marital status. 2021. https://www.statista.com/statistics/1114298/distribution-of-population-in-south-africa-by-marital-status/ (accessed 24 December 2021). [ Links ]
31. Mutale P, Kusanthan T, Ravi P. Gender risk factors associated with parasuicide in the city of Lusaka. Int J Dev Res 2015;5(11):6039-6046. [ Links ]
32. Sánchez-Teruel D, Muela-Martínez J-A, González-Cabrera M, y Herrera M-RF-A, García-León A. Variables related to suicide attempt in a Spanish province over a three-year period (2009 - 2011). Cien Saude Colet 2018;23(1):277-286. https://doi.org/10.1590/1413-812320182231.23752015 [ Links ]
33. Ki M, Seong Sohn E, An B, Lim J. Differentiation of direct and indirect socioeconomic effects on suicide attempts in South Korea. Medicine (Baltimore) 2017;96(51):e9331. https://doi.org/10.1097/md.0000000000009331 [ Links ]
34. Carter GL, SafTanko I, Lewin TJ, Whyte IM, Bryant JL. Psychiatric hospitalisation after deliberate self-poisoning. Suicide Life Threat Behav 2006;36(2):213-222. https://doi.org/10.1521/suli.2006.36.2.213 [ Links ]
35. Li X, Xu Y, Wang Y, et al Characteristics of serious suicide attempts treated in general hospitals. Chinese Ment Health J 2002;16(10):681-684. [ Links ]
36. Rajapakse T, Griffiths KM, Christensen H, Cotton S. A comparison of non-fatal self-poisoning among males and females, in Sri Lanka. BMC Psychiatry 2014;14(1):221. https://doi.org/10.1186/s12888-014-0221-z [ Links ]
37. Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: A continuing tragedy in developing countries. Int J Epidemiol 2003;32(6):902-909. https://doi.org/10.1093/ije/dyg307 [ Links ]
38. Mew EJ, Padmanathan P, Konradsen F, et al. The global burden of fatal self-poisoning with pesticides 2006 - 15: Systematic review. J Affect Disord 2017;219:93-104. https://doi.org/10.1016/j.jad.2017.05.002 [ Links ]
 Correspondence:
Correspondence:
A E Laher
abdullahlaher@msn.com
Accepted 15 February 2022.














