Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.112 n.3 Pretoria Mar. 2022
http://dx.doi.org/10.7196/SAMJ.2022.v112i3.16278
RESEARCH
Introducing an Ethics Framework for health priority-setting in South Africa on the path to universal health coverage
SAVE-UHC (South African Values and Ethics for Universal Health Coverage) Working Group and Research TeamWorking Group (in alphabetical order): D Blaauw; C Chambers; T Chirwa; N Duba; L Gwyther; K Hofman*; L London; T Masilela; N McKerrow*; O Modupe; L Moeng; V Mubaiwa; N Nematswerani; Y Ramkissoon; Y Saloojee*; S Tshabalala; K Valabhjee; M Versteeg-Mojanaga. Research Team (in alphabetical order): N Barsdorf; D Conco; M DiStefano; R Li; K Chalkidou; R Faden; S Goldstein; K Hofman; C B Krubiner; M W Merritt; A Mosam; S Potgieter; A Tugendhaft
ABSTRACT
BACKGROUND: South Africa (SA) has embarked on a process to implement universal health coverage (UHC) funded by National Health Insurance (NHI). The 2019 NHI Bill proposes creation of a health technology assessment (HTA) body to inform decisions about which interventions NHI funds will cover under UHC. In practice, HTA often relies mainly on economic evaluations of cost-effectiveness and budget impact, with less attention to the systematic, specific consideration of important social, organisational and ethical impacts of the health technology in question. In this context, the South African Values and Ethics for Universal Health Coverage (SAVE-UHC) research project recognised an opportunity to help shape the health priority-setting process by providing a way to take account of multiple, ethically relevant considerations that reflect SA values. The SAVE-UHC Research Team developed and tested an SA-specific Ethics Framework for HTA assessment and analysis
OBJECTIVES: To develop and test an Ethics Framework for use in the SA context for health priority-setting
METHODS: The Framework was developed iteratively by the authors and a multidisciplinary panel (18 participants) over a period of 18 months, using the principles outlined in the 2015 NHI White Paper as a starting point. The provisional Ethics Framework was then tested with multi-stakeholder simulated appraisal committees (SACs) in three provinces. The membership of each SAC roughly reflected the composition of a potential SA HTA committee. The deliberations and dedicated focus group discussions after each SAC meeting were recorded, analysed and used to refine the Framework, which was presented to the Working Group for review, comment and final approval
RESULTS: This article describes the 12 domains of the Framework. The first four (Burden of the Health Condition, Expected Health Benefits and Harms, Cost-Effectiveness Analysis, and Budget Impact) are commonly used in HTA assessments, and a further eight cover the other ethical domains. These are Equity, Respect and Dignity, Impacts on Personal Financial Situation, Forming and Maintaining Important Personal Relationships, Ease of Suffering, Impact on Safety and Security, Solidarity and Social Cohesion, and Systems Factors and Constraints. In each domain are questions and prompts to enable use of the Framework by both analysts and assessors. Issues that arose, such as weighting of the domains and the availability of SA evidence, were discussed by the SACs
CONCLUSIONS: The Ethics Framework is intended for use in priority-setting within an HTA process. The Framework was well accepted by a diverse group of stakeholders. The final version will be a useful tool not only for HTA and other priority-setting processes in SA, but also for future efforts to create HTA methods in SA and elsewhere
Policymakers responsible for health priority-setting are constantly challenged to use scarce resources fairly and efficiently. No country can afford everything, especially low- and middle-income countries (LMICs) where resources are scarce.[1,2] Policymakers must balance the needs of individuals and the population, with attention to equity, and also to which health needs to meet first and for whom. They also have to take into account the impact that health interventions have on other aspects of wellbeing.[3] South Africa (SA) has embarked on a process to implement universal health coverage (UHC) funded by National Health Insurance (NHI). The 2019 NHI Bill[4] aims to provide a framework for strategic purchasing of healthcare services. The Bill proposes creation of a health technology assessment (HTA) body to inform decisions about service packages and which interventions NHI funds will cover. HTA is 'a multidisciplinary process that uses explicit methods to determine the value of a health technology at different points in its lifecycle', and ideally its purpose is 'to inform decision-making in order to promote an equitable, efficient, and high-quality health system'.[5] Yet in practice, HTA often relies mainly on economic evaluations of cost-effectiveness and budget impact, with less attention to the systematic consideration of important social, organisational and ethical impacts of the health technology in question.[6-8]
Objectives
In the above context, the SAVE-UHC research project recognised an opportunity to help shape the health priority-setting process by providing a way to take account of multiple, ethically relevant considerations that reflect SA values. The Research Team developed and tested an SA-specific Ethics Framework for HTA assessment and analysis.
Methods
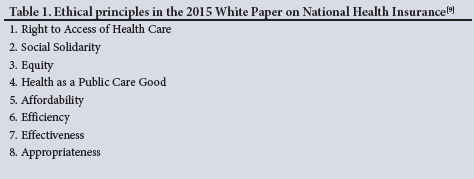
The Research Team convened a multidisciplinary panel of health and economics experts, ethicists, patient advocates and representatives of public interest groups -the 'Working Group' - to co-develop a provisional Ethics Framework through a consensus-driven process across three meetings over an 18-month period. Starting from the eight principles outlined in SA's 2015 White Paper on National Health Insurance (Table 1),[9] the Research Team and Working Group developed a tailored set of refined and supplemented values considerations for the specific context of evaluating individual health interventions for UHC funding in SA. The Framework development included a document review, facilitated discussions and hypothetical case studies to enable concretisation of the ethical issues. The Research Team provided plain-language editing for an iterated draft of the Framework and tested its use with three different simulated HTA appraisal committees (SACs), one in each of three provinces (KwaZulu-Natal, Gauteng and Western Cape). The membership of each SAC roughly reflected the composition of a potential SA HTA committee. Each 2-day simulation began with training on the Framework and health priority-setting, after which the SAC deliberated on two case studies applying the Framework. The data collected during each SAC consisted of audio recordings of the simulation, post-appraisal questionnaires, and a focus group with participants following the case study appraisals. The Research Team analysed data inductively and deductively to inform further Framework refinement. We presented the revised Framework virtually to the Working Group for final amendments and approval. This approach drew upon a similar project in Sweden to develop an ethics framework. [10] The difference was the use of illustrative case studies for the deliberations, and the testing of the framework in simulated situations. A more detailed description of our methodology has been submitted to the International Journal of Health Technology Assessment.
The study was approved by the University of the Witwatersrand Human Research Ethics Committee (R14/49, ref. no. H1907/11).
This article presents a snapshot of the resulting Ethics Framework. The full Ethics Framework (http://save-uhc.org/) and other supporting documents can be accessed (http://save-uhc.org/).
Results: The Framework
The final SAVE-UHC Ethics Framework (see Fig. 1 for a snapshot) consists of 12 domains to consider when making an HTA recommendation. We discuss each domain in detail below. The Systems Factors and Constraints domain may impact on all other domains, so it is central to the Ethics Framework.
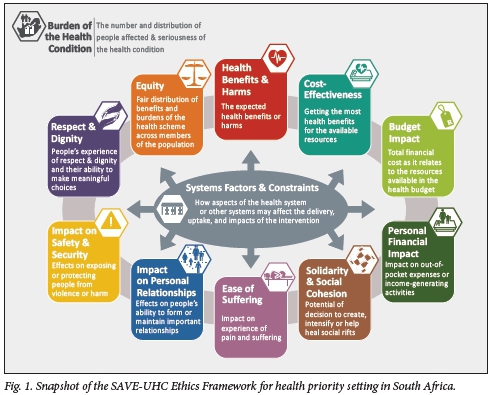
The first four domains are currently in common use internationally for health priority-setting and HTA.
1. Burden of the Health Condition provides information on scale, severity, and distribution regarding who is affected by the health issue, with respect to age, sex, geographical location and other population characteristics. The domain also looks at trends that can inform future planning. Understanding the burden contextualises the need for the intervention and whether a decision to adopt it would be in line with broader government priorities.
2. Expected Health Benefits or Harms covers information about the intervention, evidence of its effectiveness, and size and duration of health improvement(s) as well as any harms or side-effects, based on international and local studies. This domain also prompts consideration of real-world implementation, recognising that various systems factors and human behaviours can impact on the benefits and harms when interventions are rolled out.
3. Cost-Effectiveness is a common economic evaluation used for HTA analysis. It helps evaluate the comparative cost per unit of health gained, in rands spent and resources allocated, for medicines, vaccines, medical devices, diagnostics and health services. Cost-effectiveness analysis enables policymakers to look at different options to see how much more health benefit can be realised by investing in one health intervention v. other options. This is measured through incremental cost-effectiveness ratios and commonly compared against a national threshold which is developed to assess cost-effectiveness in a particular country.[11]
4. Budget Impact estimates the total cost for the government to cover the intervention for all who are eligible, to assess how affordable and sustainable that investment will be given the health budget.
The following eight domains of the Framework (in no particular order) were included to enable it to address ethical considerations of importance in SA. Some but not all of these domains appear in other, related HTA frameworks.[12]
5. Equity is about fairness, about how health is distributed across the population, and about addressing unfair inequalities in health and wellbeing more broadly. The idea is to ensure that everyone has a fair chance to benefit from the health system and to address disadvantages related to health. This domain requires assessment of whether and how an intervention may promote equity or exacerbate inequities, including by age, race, gender, class and geographical location.
6. Respect and Dignity. Human dignity and equal moral status are basic principles underlying human rights and are important in health priority-setting. Some health interventions help preserve or promote people's sense of dignity and respect by, for example, giving people more independence or choice, while others may undermine respect for deeply valued cultural traditions or individual privacy. This domain requires an assessment of whether and in what ways an intervention may either positively or negatively affect people's experience of self-respect, dignity and personal identity and/or their opportunities to make meaningful decisions about their wellbeing in line with their personal values, beliefs and life plans. The domain also addresses social stigma. Discrimination is included in this discussion, and whether implementing the intervention would infringe on people's religious, spiritual or cultural beliefs.
7. Impacts on Personal Financial Situation. A core principle of UHC is that every person in the country should be able to access quality healthcare without having to suffer financially for it. Because health coverage decisions may have significant financial impacts on individuals and families, it is important to analyse how much people may have to pay out of pocket to receive care, and ways in which health interventions may reduce financial hardship by enabling people to work and earn income.
8. Forming and Maintaining Important Personal Relationships. People's ability to form and maintain personal bonds is a core element of human wellbeing. A person's health status can dramatically affect their personal relationships and the ways in which they interact with others. This domain encourages decision-makers to consider how a health intervention may impact on important personal relationships, for better or worse. This includes family members, caregivers and friends, and the ability to participate in social and community activities.
9. Ease of Suffering. There are circumstances in which people will not be able to improve functioning, return to their 'best possible' health, or extend time before death. Even when people cannot be cured, there may still be interventions to reduce the pain or suffering they experience. However, common approaches to assess health benefits or cost-effectiveness, particularly those that focus on life-years gained, do not adequately account for the benefits of relieving pain or discomfort. This domain prompts decision-makers to consider any benefits, beyond what is counted in the health benefits section, that relate to easing pain and suffering. This domain commonly arises for palliative and end-of-life care, as well as symptom management of certain illnesses or disabilities.
10. Impact on Safety and Security. Feeling safe and being protected from harm while seeking health services, getting care or providing care is important for the wellbeing of patients and providers alike. This domain encourages decision-makers to assess whether covering a given health intervention has any considerations that relate to people's exposure to unsafe environments or dangerous encounters.
11. Solidarity and Social Cohesion. Social cohesion is the commitment of all members of society to co-operate with each other to survive, prosper and have a sense of belonging and trust. This domain addresses questions about whether an intervention has the potential to unify people within a society or drive them apart. Unlike the Personal Relationships domain, social cohesion looks at society at large; for example, how broad coverage of a vaccine might bring people together in a common cause against an infectious disease threat by building population protection, or conversely, how a targeted health intervention may drive further divisions or tensions between groups, for example if a marginalised or stigmatised group would benefit most from the intervention.
12. System Factors and Constraints operates as a cross-cutting domain, highlighting context-specific features of the health system and broader infrastructure that can have implications for how the delivery of the health intervention may play out and affect considerations under other domains. The framework lays out a range of systems factors and constraints up front, and then weaves specific considerations into each domain. These include relevant health facilities, healthcare worker capacity and availability, medical equipment and supplies, and other broader systems factors, such as access to electricity, oxygen, inadequate or unreliable internet connectivity, clean water, transportation and road infrastructure.
Participants felt that the framework assisted them in thinking differently in the appraisal and in fact, along with the discussions, changed their minds about possible recommendations.
'I fully agree with P that was what we said, but now as we sat here and we heard everyone's view I just changed my mind, because the reality is that if you choose a poor area, because you want to improve equity.' (Western Cape)
'The approach impacted positively on the deliberation because it guided our thinking and critical engagement on the topic both ethically and realistically.' (Gauteng)
Discussion
It has never been clearer, particularly during the COVID pandemic, that health and healthcare are significant for people's wellbeing, beyond their health status. Moreover, attention to health equity in priority-setting nationally and internationally is paramount to ensure that people can fairly benefit from investments in health interventions. As SA moves toward NHI implementation and the introduction of an HTA body, the SAVE-UHC Ethics Framework provides a resource to explicitly assess the wider range of ethics considerations relevant to a health coverage decision. In fact, some would suggest that priority-setting is usually focused on cost-effectiveness and budget impact without systematically taking into consideration important, locally relevant, social, organisational and ethical impacts in the health service context that are particularly important in LMICs.[3,13] Assasi et al[12]found in their systematic review that there are numerous frameworks available to include ethics in HTA, each with their own limitations and benefits. The National Institute for Health Care Excellence (NICE) in the UK does not have a specific ethics framework, but includes 'social value judgements' in their principles and methodology guidelines.[14] In 2019, a review of criteria used in decision-making in LMICs found that issues such as ethics and fairness were seldom reported.[15] A review of some Health Intervention and Technology Programme of Thailand decisions concluded that the existing conceptual framework was inadequate to capture all the elements that influence decisions, and, in particular, how they engage with social values.[16] SA can learn from other LMICs with regard to the development or implementation of HTA, including Thailand and Tanzania,[17,18] as hopefully other countries can learn from this pioneering SA experience. However, it is important for an ethics framework to be responsive to relevant features of the national context and national values in which it is intended to be used. Nationally developed, nationally specified ethics frameworks are more likely to be substantively appropriate to the task of national priority-setting and more likely to be viewed favourably by policymakers and the public alike.[3,19,20] The present study, a first in a middle-income country, demonstrates that the development of such an ethics framework for health priority-setting can be achieved using local experts and involving a wide range of interdisciplinary stakeholders.
One challenge when expanding the set of considerations used in HTA beyond the more easily quantifiable domains such as cost-effectiveness and budget impact is that it requires more information and more effort to balance considerations when they are at odds. While other approaches may be simpler, this framework was developed in recognition that health priority-setting is complex and should be informed by a comprehensive set of ethically important considerations so that decision-makers can appropriately assess, deliberate on, and justify resulting positions. In discussions with the Working Group around the number of domains, members ultimately felt that each one was needed in the Framework, though not every domain will feature prominently for every health intervention under review.
The context in which a health service operates determines whether and how the technology will function and which domains may be relevant and important.[10] In SA, system factors are critical to understanding all other domains. This includes not only the health system but other factors that could impact on a technology, for example the presence of regular electricity or clean water. In the final Framework, therefore, not only are system factors underlying all the domains, but the impact of system factors needs to be explicitly considered in each domain. Additionally, many domains relate to each other, for example an intervention improving an individual's financial situation is likely to also have positive impacts on poverty and in turn on Respect and Dignity. These are cross-referenced in the Framework.
Participants in both the Working Group and the SACs discussed whether the domains should be weighted, given that some may be seen as more important than others. For example, several of the participants indicated that equity should take priority over all other domains, given the historical and ongoing importance of equity in the SA national context. However, although an argument could be made for equity as a 'first among equals' domain in SA, the final decision endorsed by the Working Group was to leave the SAVE-UHC Ethics Framework as an unweighted, unranked set of 12 domains, primarily because the relative importance of each domain may vary depending on the type of intervention, its benefits and burdens, and who is affected. For example, the domains of Respect and Dignity, Personal Relationships and Safety and Security may be of greater importance in assessing a new type of contraceptive or other family planning interventions. In contrast, other types of health interventions may engage less significantly with these domains. Rather than assign specific weights or scores to each domain, the SAVE-UHC Ethics Framework is meant to guide deliberative decision-making so that the relevance and significance of particular domains and their considerations can be discussed in the context of a specific HTA coverage decision, and the trade-offs debated by the multidisciplinary appraisal group in order to reach consensus. In the SA context, particularly given the history of deliberative processes to end apartheid, this approach was viewed as especially useful in attempting to align or adjudicate trade-offs between the various social values.[21]
Like all good HTA and ethics analysis, applying this Framework will rely on quality evidence to feed into the process. Because many of the considerations included in the Framework domains may not be routinely captured in data collected in clinical trials and other studies, a commitment will be needed on the part of the HTA body to ensure that the evidence for the domains is available, which may involve primary research to ensure context specificity.[22] In the long term, the need for this evidence for use in national decision-making may prompt research and other mechanisms of evidence generation on topics that are relevant locally.[23]
Conclusions
The SA values and ethics framework for UHC is intended for use in health priority-setting within an HTA process in SA. The framework was well accepted by a diverse group of stakeholders. The final version will be a useful tool, not only for HTA and other priority-setting processes in SA but also for future efforts to create HTA methods in SA, and may be useful to other countries in developing their own frameworks. The COVID-19 pandemic demonstrates that having such a framework would have been helpful in making a number of critical decisions, for example in the pricing, procurement and allocation of vaccines, treatments, oxygen and critical care beds for COVID-19, as well as for procurement and allocation of personal protective equipment.[24-26] In the context of a constrained budget and severe hardship caused by the pandemic, going forward, careful priority-setting using local ethics and values is essential. This Framework will assist this process.
Declaration. None.
Acknowledgements. The time and insights of the attendees of the three SACs, and the support in materials development by Karen Hurt, Dr Debbie L Marais, Dr Taryn Young and Cynthia Ngwalo, are acknowledged.
Author contributions (in alphabetical order). NB, KC, RF, KH and CBK
conceptualised the study. All authors engaged with the Working Group. SG, CBK and AM wrote the protocol for testing the Framework using SACs. NB, SG, CBK, AM, SP and AT did the fieldwork. NB, MD, SG, CBK, AM, MWM and SP analysed the data. DC facilitated the SACs and analysed data. NB, RF, CBK and MWM led on revisions to the Framework document. SG created the initial draft of this manuscript. All authors and the Working Group edited and reviewed the manuscript and gave final approval for submission.
Funding. This research was funded by the Wellcome Trust (grant no. 208045/Z/17/Z) and partly supported by the South African Medical Research Council (grant no. 23108).
Conflicts of interest. None.
References
1. Hollingworth S, Gyansa-Lutterodt M, Dsane-Selby L, et al. Implementing health technology assessment in Ghana to support universal health coverage: Building relationships that focus on people, policy, and process. Int J Technol Assess Health Care 2020;36(1):8-11. https://doi.org/10.1017/s0266462319000795 [ Links ]
2. Kapiriri L, Baltussen R, Oortwijn W. Implementing evidence-informed deliberative processes in health technology assessment: A low income country perspective. Int J Technol Assess Health Care 2020;36(1):29-33. https://doi.org/10.1017/s0266462319003398 [ Links ]
3. Chalkidou K, Li R, Culyer AJ, Glassman A, Hofman KJ, Teerawattananon Y. Health technology assessment: Global advocacy and local realities; comment on 'Priority setting for universal health coverage: We need evidence-informed deliberative processes, not just more evidence on cost-effectiveness. Int J Health Policy Manag 2017;6(4):233-236. https://doi.org/10.15171/ijhpm.2016.118 [ Links ]
4. Republic of South Africa. National Health Insurance Bill (B11-2019). https://www.gov.za/documents/national-health-insurance-bill-b-11-2019-6-aug-2019-0000 (accessed 10 September 2021). [ Links ]
5. O'Rourke B, Oortwijn W, Schuller T. The new definition of health technology assessment: A milestone in international collaboration. Int J Technol Assess Health Care 2020;36(3):187-190. https://doi.org/10.1017/s0266462320000215 [ Links ]
6. Ten Have H. Ethical perspectives on health technology assessment. Int J Technol Assess Health Care 2004;20(1):71-76. https://doi.org/10.1017/s0266462304000819 [ Links ]
7. Saarni SI, Hofmann B, Lampe K, et al. Ethical analysis to improve decision-making on health technologies. Bull World Health Organ 2008;86(8):617-623. https://doi.org/10.2471/BLT.08.051078 [ Links ]
8. Byskov J, Bloch P, Blystad A, et al. Accountable priority setting for trust in health systems - the need for research into a new approach for strengthening sustainable health action in developing countries. Health Res Policy Syst 2009;7(1):23. https://doi.org/10.1186/1478-4505-7-23 [ Links ]
9. National Department of Health, South Africa. White Paper on National Health Insurance. Government Gazette No. 39506:1230, 11 December 2015. https://www.gov.za/sites/default/files/gcis_document/201512/39506gon1230.pdf (accessed 9 September 2021). [ Links ]
10. Heintz E, Lintamo L, Hultcrantz M, et al. Framework for systematic identification of ethical aspects of healthcare technologies: The SBU approach. Int J Technol Assess Health Care 2015;31(3):124-130. https://doi.org/10.1017/S0266462315000264 [ Links ]
11. Edoka IP, Stacey NK. Estimating a cost-effectiveness threshold for health care decision-making in South Africa. Health Policy Plan 2020;35(5):546-555. https://doi.org/10.1093/heapol/czz152 [ Links ]
12. Assasi N, Schwartz L, Tarride JE, Campbell K, Goeree R. Methodological guidance documents for evaluation of ethical considerations in health technology assessment: A systematic review. Expert Rev Pharmacoecon Outcomes Res 2014;14(2):203-220. https://doi.org/10.1586/14737167.2014.894464 [ Links ]
13. Hipgrave DB, Alderman KB, Anderson I, Soto EJ. Health sector priority setting at meso-level in lower and middle income countries: Lessons learned, available options and suggested steps. Soc Sci Med 2014;102:190-200. https://doi.org/10.1016/j.socscimed.2013.11.056 [ Links ]
14. National Institute for Health and Care Excellence (NICE). Our charter. 2021. https://www.nice.org.uk/about/who-we-are/our-charter (accessed 6 December 2021). [ Links ]
15. Kaur G, Prinja S, Lakshmi PVM, Downey L, Sharma D, Teerawattananon Y. Criteria used for priority-setting for public health resource allocation in low- and middle-income countries: A systematic review. Int J Technol Assess Health Care 2019;35(6):474-483. https://doi.org/10.1017/s0266462319000473 [ Links ]
16. Tanttivess S, Pérez Velasco R, Yothasamut J, Mohara A, Limprayoonyong H, Teerawatttananon Y. Efficiency or equity: Value judgments in coverage decisions in Thailand. J Health Organ Manag 2012;26(3):331-342. https://doi.org/10.1108/14777261211238972 [ Links ]
17. Leelahavarong P, Doungthipsirikul S, Kumluang S, et al Health technology assessment in Thailand: Institutionalisation and contribution to healthcare decision making: Review of literature. Int J Technol Assess Health Care 2019;35(6):467-473. https://doi.org/10.1017/s0266462319000321 [ Links ]
18. Surgey G, Chalkidou K, Reuben W, Suleman F, Miot J, Hofman K. Introducing health technology assessment in Tanzania. Int J Technol Assess Health Care 2020;36(2):80-86. https://doi.org/10.1017/s0266462319000588 [ Links ]
19. Western Cape Department of Health, South Africa. An ethical framework for decision-making. 2007. https://www.dailymaverick.co.za/wp-content/uploads/Oped-Benatar-CovResourcesTW-Priority-setting-tool-for-the-Western-Cape.pdf (accessed 9 September 2021). [ Links ]
20. Reuzel R, Oortwijn W, Decker M, et al. Ethics and HTA: Some lessons and challenges for the future. Poiesis Prax 2004;2(2):247-256. https://doi.org/10.1007/s10202-003-0054-1 [ Links ]
21. Tugendhaft A, Hofman K, Danis M, et al Deliberative engagement methods on health care priority-setting in a rural South African community. Health Policy Plan 2021;36(8):1279-1291. https://doi.org/10.1093/heapol/czab005 [ Links ]
22. Wilkinson M, Hofman KJ, Young T, Schmidt B-M, Kredo T. Health economic evidence in clinical guidelines in South Africa: A mixed-methods study. BMC Health Serv Res 2021;21(1):738. https://doi.org/10.1186/s12913-021-06747-z [ Links ]
23. Barsdorf N, Millum J. The social value of health research and the worst off. Bioethics 2017;31(2):105-115. https://doi.org/10.1111/bioe.12320 [ Links ]
24. Moodley K, Blockman M, Pienaar D, et al. Hard choices: Ethical challenges in phase 1 of COVID-19 vaccine roll-out in South Africa. S Afr Med J 2021;111(6):554-558. https://doi.org/10.7196/SAMJ.2021.v111i6.15593 [ Links ]
25. Moodley K, Rossouw T. What could fair allocation of an efficacious COVID-19 vaccine look like in South Africa? Lancet Glob Health 2021;9(2):e106-e107. https://doi.org/10.1016/S2214-109X(20)30474-5 [ Links ]
26. Erasmus N. Age discrimination in critical care triage in South Africa: The law and the allocation of scarce health resources in the COVID-19 pandemic. S Afr Med J 2020;110(12):1172-1175. https://doi.org/10.7196/SAMJ.2020.v110i12.15344 [ Links ]
 Correspondence:
Correspondence:
S Goldstein
susan.goldstein@wits.ac.za
Accepted 17 December 2021
* Served as Chair for at least one Working Group meeting.














