Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.111 n.12 Pretoria Dec. 2021
http://dx.doi.org/10.7196/samj.2021.v111i12.15761
RESEARCH
Secondary health conditions in people with spinal cord injury in South Africa: Prevalence and associated factors
S PilusaI; H MyezwaII; J PottertonIII
IBSc (Physiotherapy), MPH; Physiotherapy Department, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg South Africa
IIBSc (Physiotherapy), MSc (Physiotherapy), PhD; School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIBSc (Physiotherapy), MSc (Physiotherapy), PhD; Physiotherapy Department, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg South Africa
ABSTRACT
BACKGROUND: People with spinal cord injury (SCI) experience preventable secondary health conditions (SHCs) that worsen the disability, reduce the quality of life and affect health and wellbeing. There is limited information on the prevalence of SHCs and the associated factors to inform planning and practice in South Africa (SA
OBJECTIVES: To identify the prevalence of SHCs and the associated factors in people with SCI
METHODS: We conducted a retrospective review of patients' medical records at a tertiary academic hospital and a rehabilitation hospital in Gauteng Province, SA. Data collected included demographic data, injury profile, SHCs and associated factors. Data were summarised using descriptive statistics of frequency and percentages. Fisher's exact test was used to determine the association between SHCs and sociodemographic and clinical variables. The Mann-Whitney U-test was used to determine the associated risk factors for SHCs. Multinomial regression was used to determine the predictors of the frequency of SHCs
RESULTS: A total of 425 records were reviewed, 68.0% of patients were male, and the median (interquartile range) age was 45 (35 - 56) years. The majority (93.7%) of the patients had SHCs, and 78% had >2 SHCs. Significant predictors of having >3 SHCs were the duration of SCI (p=0.01), site of injury in the upper (p=0.03) and lower (p=0.01) thoracic spine, being unemployed (p=0.04), and public hospital income classification (HO = social grant/unemployed, H1 = earning ZARO - 70 000 per annum single income/ZARO - 100 000 per annum household income, and Road Accident Fund; p=0.03, p=0.03 and p=0.01, respectively
CONCLUSIONS: Secondary health conditions were prevalent among patients with SCI. People with SCI experience multimorbidity that requires multiple management strategies. These findings point to the need for prevention strategies to minimise the occurrence of SHCs
Spinal cord injury (SCI) is a devastating condition, causing severe disability and contributing to the global health burden.[1] There is no national data base for SCI in South Africa (SA). However, the Global Burden of Disease Study 2016 estimated the prevalence of SCI at 206/100 000.[1] This figure could be an underestimate, given that apart from traumatic injuries, several other conditions such as HIV and tuberculosis contribute to the burden of disease.[2] SCI has long-term consequences affecting the individual's health, their family, and the health system.[3,4]
Several studies have reported a high prevalence of secondary health conditions (SHCs) in people with SCI. The spectrum of SHCs includes pain, respiratory problems, oedema, autonomic dysreflexia pressure sores, spasms, depression, contractures, and sexual, bowel and bladder problems.[5,6] The prevalence of SHCs increases with the length of time individuals have lived with SCI.[7] In the early stages of SCI, the prevalence of SHCs ranges from 50% to 78%,[8] increasing to 89 - 98.5% 4 - 10 years after SCI.[5,9]
Several modifiable and non-modifiable risk factors influence the development of SHCs.[10] Non-modifiable risk factors associated with their development include gender, age and SCI profile (type, level, completeness, and time since injury).[7,11] Females are more at risk for bladder dysfunction and depression[11] and tend to report greater pain severity than males.[7] Males with SCI are more at risk for sexual problems and pressure sores.[11] Older age is associated with pain, sexual problems and sleep problems.[11] People with complete lesions and tetraplegia have a high risk for multiple SHCs.[9,11-13] Modifiable risk factors include high body mass index (BMI),[7,10] smoking,[14] lack of knowledge about SHCs,[15] unemployment[10] and healthcare system inefficiencies.[16,17] Data on SHCs and associated risk factors in SA are needed to inform patient care and develop targeted context-specific prevention interventions.
SHCs affect overall health. Their presence limits self-care, restricts participation in social activities and affects mental wellbeing. [3,4,18,19]Over time, SHCs worsen the disability resulting from the SCI.[20] Other consequences of SHCs include high readmission rates[21] and an increased mortality rate resulting from the higher risk of infection from pressure sores and urinary tract infections.[22] Good health for people with disabilities is a fundamental right[23] promoted by Sustainable Development Goal 3.[23,24]
Objectives
To improve understanding of the prevalence of SHCs in patients with SCI and the associated risk factors in SA to help develop tailored prevention strategies.
Methods
A retrospective study design was used to collect data from medical records of patients with SCI at two tertiary hospitals (an academic hospital and a rehabilitation hospital) in Gauteng Province, SA. The two hospitals serve 2.92 million people and referral hospitals from neighbouring provinces that do not have specialised care and rehabilitation facilities. The rehabilitation hospital admits patients with various physical disabilities, offering medical care, physiotherapy, occupational therapy, social work, and speech and hearing therapy. Outpatient care is provided to discharged patients once a month, including medical care, wound care management, and repeat medicine and medical consumables.
Only medical records for discharged patients with SCI at the academic hospital who had been admitted between January 2014 and September 2018 were reviewed. At the rehabilitation hospital, only the medical records of patients with SCI who used the facility between January 2016 and September 2017 and who gave consent during their outpatient department visit were reviewed. Medical records of patients with other neurological impairments or pathology such as stroke and amputations were excluded.
The sample size was calculated based on data from a previous study that looked at the prevalence of SHCs in people with SCI.[12] Using a power of 95%, a level of significance of 5% and a prevalence of SHCs of 50.3%, a minimum sample size of 385 records was calculated for the sample population.[25]
Data collection tool
The researchers developed a questionnaire data collection form based on previous studies on SHCs.[7] The form had four sections. Section A included sociodemographic data items (age, marital status, race, income source and education level). Hospital income categories are used to categorise patients' income status at public health hospitals to determine healthcare cost subsidy, as follows: HO = social grant, pensioners and unemployed - full subsidy; HI = ZAR0 - 70 000 per annum single income/ZARO - 100 000 per annum household income - partial subsidy; H2 = ZAR 70 000 - 250 000 single income/ ZAR100 000 - 350 000 per annum household income - partial subsidy; H3 = >ZAR250 000 per annum single income/ZAR350 000 household income - partial subsidy; Road Accident Fund (RAF) = patient who was involved in a pedestrian or motor vehicle accident and is eligible for RAF cover.
Section B included items on the SCI profile (date of injury, type of lesion, cause of injury, level of injury, American Spinal Injury Association (ASIA) Scale score). Section C captured information on risk factors such as smoking, alcohol consumption, metabolic problems and chronic diseases. Section D recorded SHCs. The data collection tool was checked for content validity by rehabilitation therapists. Feedback from the therapists resulted in the addition of risk factors (drugs), chronic conditions (HIV/AIDS), and further details on SHCs including deep-vein thrombosis, types of bowel problems, grading of pressure sores, spasticity, types of injury, postural deformities (scoliosis, kyphosis) and post-traumatic syringomyelia.
Data analysis
The data were extracted to Excel, 2016 version (Microsoft, USA) from the REDCap (Research Electronic Data Capture) online database manager at the University of the Witwatersrand and imported into SPSS 25 (IBM, USA) for analysis. The data were summarised using descriptive statistics of frequency and percentages for the categorical variables. Medians and interquartile ranges (IQRs) were used to summarise the continuous variable of age. Fishers exact test was used to determine the association between SHCs and sociodemographic and clinical variables, and the Mann-Whitney U-test to evaluate the difference between the age of the participants with and without SHCs. Binary logistic regression analysis was used to determine the predictors of the frequency of SHCs. The level of significance was set atp<0.05.
Ethical considerations
The SA National Health Research Database (ref. no. GP201712036) and the two study sites gave permission before data were collected. The study was approved by the human research ethics committees of the University of the Witwatersrand (ref. no. M170938) and the University of Pretoria (ref. no. 36/2018). Informed consent was obtained from patients with SCI before reviewing their medical records at the rehabilitation hospital. All the medical patient records were given a unique data reference number on the data extraction sheet.
Results
We reviewed 425 medical records.
Sociodemographic characteristics
The sociodemographic characteristics of the participants are presented in Table 1.
The patients' median (IQR) age was 45 (35 - 56) years, and most of the patients were males (68.0%).
SCI profile and SHCs
Table 2 outlines the cause of the patients' SCIs, neurological level, and time since injury. The majority of the patients had traumatic SCI (64.7%) and had paraplegia (68.5%), and the median (IQR) time since injury was 4.2 (2.3 - 6.1) years. The range of time since injury was 0.5 - 44.2 years.
Prevalence of SHCs
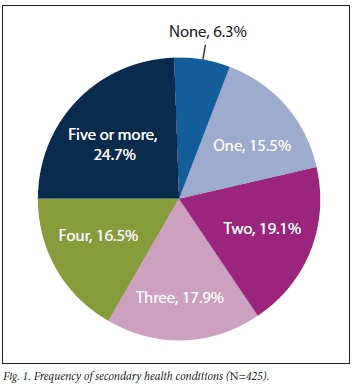
SHCs were present in 93.7% of the patients, and 24.7% had >5 SHCs (Fig. 1).
SHCs identified
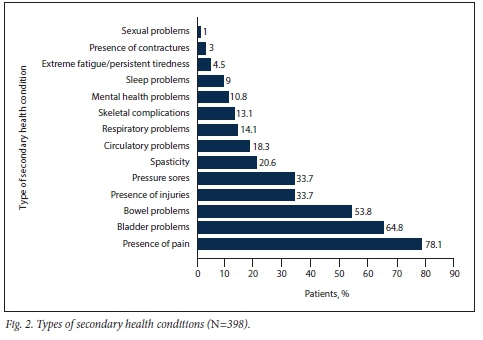
The most common SHCs identified in this population were the presence of pain (78.1%), bladder problems (64.8%), bowel problems (53.8%) and pressure sores (33.7%) (Fig. 2).
Predictors of SHCs
Univariate binary logistic regression analysis showed that employment status was a significant predictor of the presence of SHCs, with unemployment increasing the risk of SHCs (odds ratio (OR) 2.95 (95% confidence interval (CI) 1.33 - 6.53); p=0.01). This result is not statistically significant, as the CI crosses 1. Time since injury was a predictor of SHC after adjusting for gender and age. As the time since injury increased by 1, the adjusted OR of presenting with SHC increased by 1.43 (95% CI 1.09 - 1.88), and the result was statistically significant (Table 3). The median (IQR) time since injury was significantly longer in patients with SHCs (4.3 (2.3 - 6.3) years) than in patients with no SHCs (2.5 (1.8 - 3.8) years) (Table 2). Multivariate stepwise (forward likelihood ratio (LR)) binary logistic regression analysis was performed, adjusting for gender and age with the following variables: employment status, smoking, time since the injury, income classification, cause of injury, level of injury and site of injury. Smoking, type of injury and site of injury were excluded because they did not meet the binary logistic regression assumption. Some cells had zero and were therefore not included in the regression model.[26]
Predictors of the frequency of SHCs
To determine the predictors of the frequency of SHCs, the frequency was categorised into two categories, low (<3) and high (>3), using the median (3) as the cut-off as described by DeCoster et al.[27]Participants with no SHCs were excluded from this analysis. Fisher's exact test showed that the following were significantly associated with the frequency of SHCs: employment status (p=0.00), income classification (p=0.00), type of injury (p=0.02), level of injury (p=0.00) and level of completeness (p=0.00). The Mann-Whitney U-test showed a significant difference in the time since injury between low (<3) and high (>3) SHCs. All the variables with ap-value <0.05 were included in the regression model.
Multivariate stepwise (forward LR) binary logistic regression analysis was performed, adjusting for gender and age with the following variables: employment status, smoking, time since the injury, income classification, cause of injury, level of injury and site of injury. The excluded variables were age, gender, level of lesion, smoking and type of injury. The results showed that level of injury income classification, time since injury and employment status were predictors of >3 SHCs (Table 4). Patients with upper thoracic and lower thoracic injury, those on a social grant, RAF recipients, those in the HI income category and those who were unemployed were more likely to present with >3 SHCs (Table 4).
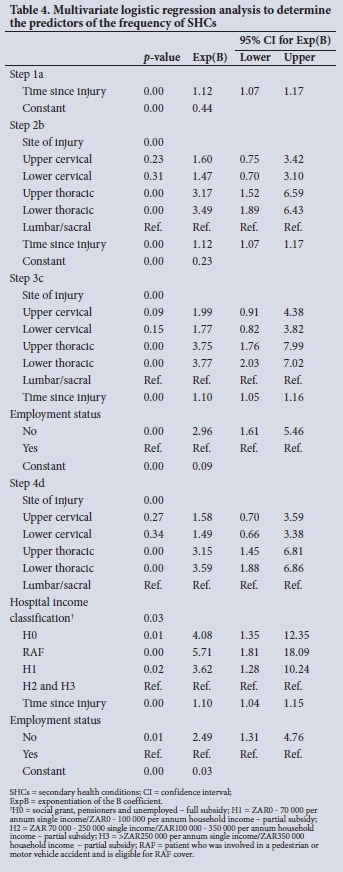
Site of injury. The adjusted OR of presenting with >3 SHCs increased by 3.15 (95% CI 1.45 - 6.81) and 3.59 (95% CI 1.88 - 6.86) in the participants with upper thoracic and lower thoracic injuries, respectively, and the result was statistically significant.
Income classification and employment status. The adjusted OR of presenting with >3 SHCs increased by 4.08 (95% CI 1.35 - 12.35), 5.71 (95% CI 1.81 - 18.09) and 3.62 (95% CI 1.28 - 10.24) in the social grant, RAF and HI categories, respectively, and the result was statistically significant. The OR of presenting with >3 SHCs in the unemployed category increased by 2.49 (95% CI 1.31 - 4.76), and the result was statistically significant.
Time since injury. For every year of living with SCI, the odds of presenting with >3 SHCs increased by 1.10 (95% CI 1.04 - 1.15).
Discussion
This study aimed to identify the prevalence of SHCs and associated factors in people with SCI. As previously reported in other studies,[5,7] the prevalence of SHCs was high (96.7%). This figure is higher than reported prevalences in other SA-based studies.[8,9] Madasa et al[9] reported a prevalence of SHCs of 89% up to 4 years after SCI. Joseph and Nilsson Wikmar[8] reported a 50.3% prevalence among patients with SCI during the acute hospitalisation phase. The difference in the findings could be due to the inclusion of patients with both non-traumatic and traumatic lesions in our study, while Madasa et al[9] and Joseph and Nilsson Wikmar[8] focused only on traumatic SCI. These results confirm the need for preventive care services for people with SCI to minimise the occurrence of SHCs. Continuous surveillance of these patients is needed to track health outcomes, identify needs and inform the development of prevention strategies.
We found multimorbidity of SHCs, 24.7% of our patients having >5 SHCs. Multimorbidity is common in people with SCI, with 2-15 SHCs being reported in other studies.[9-11] The occurrence of multiple SHCs is indicative of the extent and severity of the problem. Having multiple SHCs has been shown to affect quality of life, functioning[20,28] and life satisfaction.[10] Managing more than two SHCs concurrently can lead to polypharmacy[29] and high demand for healthcare.[28] These findings must be considered when developing a preventive care model to target multiple SHCs and their associated risk factors.
In order to develop tailored prevention interventions for SHCs, knowledge of the associated factors is essential. Multimorbidity has been reported to be associated with older age, unemployment, higher BMI,[10] complete paraplegia, tetraplegia and non-traumatic SCI.[11] However, in our study, we only found injury site, income classification, time since injury and employment status to be significant predictors for multiple SHCs. Concerning the site of injury, participants with upper and lower thoracic spine injury had significantly higher odds (3.15 and 3.59, respectively) of having multiple SHCs. This finding was similar to that reported by Brinkhof et al.,[11]although in their study, patients with complete paraplegia or tetraplegia were more likely to have multimorbidity than those with incomplete paraplegia. Our findings show the high risk of readmission among individuals with SCI lesions in the upper thoracic region (Tl - T6) and those with paraplegia (OR 2.6 and 2.3, respectively).[21] Individuals with upper and lower thoracic lesions have upper limb strength and should be independent in daily life activities, but it seems that there are still challenges in terms of preventing SHCs.[30] Furthermore, considering that people with thoracic SCI lesions use their upper limbs for all activities of daily living, they will be prone to overuse injuries resulting in pain. Upper thoracic lesions may also result in autonomic dysreflexia and respiratory problems due to paralysis of the respiratory muscles.
The duration of injury was another predictor for multiple SHCs. With each year lived with SCI, the risk of developing multiple SHCs increased. The presence of SHCs worsens the disability,[20] which can increase the risk of SHCs.[11] Other possible factors not explored in this study include 'forgetting' to practise prevention care,[15] mental health problems[31] and systemic environmental barriers.[32] These findings could imply the need to extend support for people with SCI as they live longer
Poor socioeconomic status is associated with adverse health outcomes.[33,34]The unemployed, individuals in the social grant income category, and those in the H1 category had significantly higher odds of presenting with >3 SHCs. The impact of unemployment on a person with a disability is devastating because it can lead to loss of lifes meaning[3] and economic vulnerability.[35] Living with a disability can be costly owing to disability-related costs such as hiring transport, paying a caregiver and buying medication. A social grant may not be enough to cover all the costs.[36] It was surprising that the RAF recipients were at risk of multimorbidity. The RAF is an insurance cover for all road users, and people who incur injury or disability can claim for loss of income and medication expenses. The fund ensures access to the resources needed to self-manage and to prevent the occurrence of SHCs. Possible reasons for the relationship between being an RAF recipient and multimorbidity could be payment delays or that the funds paid had run out, leaving the individual with no cover for long-term disability-related costs. Another perspective could be related to the severity of the injury, so that even if there are RAF funds, the severity of the SCI increases vulnerability to SHCs. Future research is needed to clarify whether the RAF improves health outcomes and access to health resources. Economic vulnerability and the impact on disability and health outcomes must be considered when developing prevention interventions.[37,38]
The most prevalent SHCs were pain (78.1%), bladder problems (64.8%) and bowel problems (53.8%). Pain and bladder and bowel problems are the most commonly reported and significant SHCs experienced by people with SCI.[39] Similar to findings in previous studies, pain was the most prevalent SHC.[5,9] Pain limits self-care,[40] restricts participation in working life,[4] and is associated with depression[41] and disability.[20] Pain is usually managed with medication, but overuse, misuse, dependence and non-effectiveness must be addressed.[42] Bladder and bowel problems are significant issues that negatively affect health[13] and are a source of fear and shame.[19] They require extra time to manage, disrupting daily routines.[18] Bowel and bladder problems are associated with poor health status[13] and depression[40] and restrict participation in home and social activities.[18]
Study limitations
Incomplete and illegible medical records posed a challenge. Important information on the severity of the injury and the patients' education level was often missing.
Conclusions
SHCs are prevalent among people with SCI. A high proportion of patients had multimorbidity, indicating challenges related to preventing SHCs. The predictors of multimorbidity were SCI duration, a thoracic lesion, unemployment, and income classification (no income, social grant, RAF). These findings underscore the need to strengthen preventive care for people with SCI. Models of care for people with SCI must address multimorbidity and the predictors thereof
Implications of the study findings
• Practice. Health professionals can use the findings to inform preventive interventions. For example, patients with SCI should be educated on SHCs throughout the continuum of care. During clinic visits, screening for SHCs can be conducted to identify risk factors and minimise the occurrence and progress of SHCs. Patients with risk factors for SHCs can be flagged for targeted intervention for follow-up care after discharge and tailored patient-centred intervention.
• Research. There is a need for prospective longitudinal studies to track health outcomes related to SCI and identify unmet care needs.
Declaration. The research for this study was done in partial fulfilment of the requirements for SP's PhD degree at the University of the Witwatersrand.
Acknowledgements: None.
Author contributions. SP: conceptualised the study collected data, analysed data and wrote the manuscript. HM and JP: supervision during the conceptualisation phase, assisted during data analysis, read several versions of the article and did the final editing.
Funding. SP was supported by:
1. The Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (grant no. G-19-57145), Sida (grant no. 54100113), Uppsala Monitoring Centre and the DELTAS Africa Initiative (grant no. 107768/Z/15/Z). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)'s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa's Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (UK) and the UK government. The statements made and views expressed are solely the responsibility of the Fellow.
2. National Research Foundation grant (Thuthuka).
The statements made and views expressed are solely the responsibility of the authors. Neither funder played any role in the study design, in collection, analysis and interpretation of data, or in writing the manuscript.
Conflicts of interest. None.
References
1. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990 - 2016 . A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18(1):56-87. https://doi.org/10.1016/S1474-4422(18)30415-0 [ Links ]
2. Mayosi BM, Benatar SR. Health and health care in South Africa - 20 years after Mandela. N Engl J Med 2014;371(14):1344-1353. https://doi.org/10.1056/nejmsrl405012 [ Links ]
3. Fuseini A, Aniteye P, Alhassan A. Beyond the diagnosis. Lived experiences of persons with spinal cord injury in a selected town in Ghana. Neurol Res Int 2019;2019:9695740. https://doi.org/10.1155/2019/9695740 [ Links ]
4. Callaway L, Barclay L, Mcdonald R, Farnworth L, Casey J. Secondary health conditions experienced by people with spinal cord injury within community living. Implications for a National Disability Insurance Scheme. AustOccup Ther J 2015;62(4):246-254. https://doi.org/10.1111/1440-1630.12206 [ Links ]
5. Adriaansen J, Ruijs L, Koppenhagen C, et al Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med 2016;48(10):853-860. https://doi.org/10.2340/16501977-2166 [ Links ]
6. Stillman MD, Barber J, Burns S, Wilhams S, Hoffman JM. Complications of spinal cord injury over the first year after discharge from inpatient rehabilitation. Arch Phys Med Rehabil 2017;98(9):1800-1805. https://doi.org/10.1016/j.apmr.2016.12.011 [ Links ]
7. Adriaansen JJE, Post MWM, de Groot S, et al. Secondary health conditions in persons with spinal cord injury. A longitudinal study from one to five years post-discharge. J Rehabil Med 2013;45(10):1016-1022. https://doi.org/10.2340/16501977-1207 [ Links ]
8. Joseph C, Nilsson Wikmar N. Prevalence of secondary medical complications and risk factors for pressure ulcers after traumatic spinal cord injury during acute care in South Africa. Spinal Cord 2016;54(7):535-539. https://doi.org/10.1038/sc2015.189 [ Links ]
9. Madasa V, Boggenpoel B, Phillips J, Joseph C. Mortality and secondary complications four years after traumatic spinal cord injury in Cape Town, South Africa. Spinal Cord Ser Cases 2020,6.84. https://doi.org/10.1038/s41394-020-00334-w [ Links ]
10. Rivers CS, Fallah N, Noonan VK, et al. Health conditions. Effect on function, health-related quality of life, and life satisfaction after traumatic spinal cord injury. A prospective observational registry cohort study. Arch Phys Med Rehabil 2018;99(3):443-451. https://doi.org/10.1016/j.apmr.2017.06.012 [ Links ]
11. Brinkhof M, Al-Khodairy A, Eriks-Hoogland I, et al. Health conditions in people with spinal cord injury. Contemporary evidence from a population-based community survey in Switzerland. J Rehabil Med 2016;48(2):197-209. https://doi.org/10.2340/16501977-2039 [ Links ]
12. Joseph C, Nilsson Wikmar L. Prevalence of secondary medical complications and risk factors for pressure ulcers after traumatic spinal cord injury during acute care in South Africa. Spinal Cord 2016;54(7):535-539. https://doi.org/10.1038/sc2015.189 [ Links ]
13. Park SE, Elliott S, Noonan VK, et al. Impact of bladder, bowel and sexual dysfunction on health status of people with thoracolumbar spinal cord injuries living in the community. J Spinal Cord Med 2017;40(5):548-559. https://doi.org/10.1080/10790268.2016.1213554 [ Links ]
14. January A, Zebracki K, Chlan K, Vogel L. Mental health and risk of secondary medical complications in adults with pediatric-onset spinal cord injury. Top Spinal Cord Inj Rehabil 2014,20(1).1-12. https://doi.org/10.1310/sci2001-l [ Links ]
15. Visser AM, Surona V. Pressure ulcer knowledge, beliefs and practices in a group of South Africans with spinal cord injury. Spinal Cord Ser Cases 2019;5:83. https://doi.org/10.1038/s41394-019-0226-4 [ Links ]
16. Fuseini A-G, Aniteye P, Kofi-Helegbe G. Barriers and facilitators related to the health care system in spinal cord injury. Nurs Pract Today 2018;5(3):335-346. http://41.66.217.101/bitstream/123456789/2437/l/BARRIERS%20AND%20FACILITATORS%20RELATED%20TO%20THE%20HEALTH%20CARE%20SYSTEM%20IN%20SPINAL%20CORD%20INJURY.pdf (accessed 28 October 2021). [ Links ]
17. Guilcher SJT, Craven BC, Lemieux-Charles L, Casciaro T, McColl MA, Jaglal SB. Secondary health conditions and spinal cord injury. An uphill battle in the journey of care. Disabil Rehabil 2013;35(11):894-906. https://doi.org/10.3109/09638288.2012.721048 [ Links ]
18. Van der Meer P, Post MWM, van Leeuwen CMC, van Kuppeveit HJM, Smit CAJ, van Asbeck FWA. Impact of health problems secondary to SCI one and five years after first inpatient rehabilitation. Spinal Cord 2017;55(1):98-104. https://doi.org/10.1038/sc.2016.103 [ Links ]
19. Pilusa SI, Myezwa H, Potterton J. Experiences of secondary health conditions amongst people with spinal cord injury in South Africa. A qualitative study. S Afr J Physiother 2021;77(1):1-8. https://doi.org/10.4102/sajp.v77il.l530 [ Links ]
20. Richardson A, Samaranayaka A, Sullivan M, Derrett S. Secondary health conditions and disability among people with spinal cord injury. A prospective cohort study. J Spinal Cord Med 2021;44(1):19-28. https://doi.org/10.1080/10790268.2019.1581392 [ Links ]
21. Mashola MK, Olorunju SAS, Mothabeng J. Factors related to hospital readmissions in people with spinal cord injury in South Africa. S Afr Med J 2019;109(2):107-111. https://doi.org/10.7196/SAMJ.2019.v109i2.13344 [ Links ]
22. Oderud T. Surviving spinal cord injury in low income countries. Afr J Disabil 2014;3(2):a80. https://doi.org/10.4102/ajod.v312.80 [ Links ]
23. United Nations. Convention on the Rights of Persons with Disabilities and Optional Protocol 2006,19. https://www.un.org/disabilities/documents/convention/convoptprot-e.pdf (accessed 25 May 2019). [ Links ]
24. World Health Organization. SDG 3. Ensure healthy lives and promote welibeing for all at all ages. 2017. http://www.who.int/sdg/targets/en/ (accessed 3 December 2018). [ Links ]
25. Naing L, Winn T, Rush BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci 2006;1.:9-14. https://www.scribd.com/doc/63105077/How-to-Caiculate-Sample-Size (accessed 28 October 2021). [ Links ]
26. Mansournia MA, Geroldinger A, Greenland S, Heinze G. Separation in logistic regression. Causes; consequences, and control Am J Epidemiol 2018;187(4):864-870. https://doLorg/10.1093/aje/kwx299 [ Links ]
27. DeCoster J, Galiucci M, Iselin A-MR. Best practices for using median splits, artificial categorisation, and their continuous alternatives. J Exp Psychopathol 2011;2(2):197-209. https://doi.org/10.5127/jep.008310 [ Links ]
28. Noonan V, Faliah N, Park S, et aL Health care utilisation in persons with traumatic spinal cord injury. The importance of muitimorbidity and the impact on patient outcomes. Top Spinal Cord Inj Rehabil 2014;20(4):289-301. https://doi.org/10.1310/scl2004-289 [ Links ]
29. Patel T, Mi 11 iga n J, Lee J. Medication-relate d problems in individuals with spinal cord injury in a primary care-based clinic. JSpinal Cord Med2017; 40(l):54-61. https://doi.org/10.1179/2045772315Y.0000000055 [ Links ]
30. Sezer N. Chronic complications of spinal cord injury. World J Orthop 2015;6(1):24-33. https://doi.org/10.5312/wjo.v6.il.24 [ Links ]
31. Pilusa S, Myezwa H, Potterton J, Sciences H, Africa S, Pilusa S.' I forget to do pressure relief'. Personal factors influencing the prevention of secondary health conditions in people with spinal cord injury, South Africa. S Afr J Physiother 2020;77(1):1-9. https://doi.org/10.4102/sajp.v7711.1493 [ Links ]
32. Maart S, Jelsma J. Disability and access to health care - a community based descriptive study. Disabil Rehabil 2014;36(18):1489-1493. https://doi.org/10.3109/09638288.2013.807883 [ Links ]
33. Gordon T, Booysen F, Mbonigaba J. Socio-economic inequalities in the multiple dimensions of access to healthcare. The case of South Africa. BMC Public Health 2020;20(1):289. https://doi.org/10.1186/ [ Links ]
34. Von Fintel M. Chronic child poverty and health outcomes in South Africa using a multidimensional poverty measure. Child Indie Res 2021;14:1571-1596. https://doi.org/10.1007/sl2187-021-09817-0 [ Links ]
35. Hanass-Han cock J, McKenzie TC. People with disabilities and in come-relate d social protection measures in South Africa-. Where is the gap? Afr J Disabil 2017;6:a300. https://doi.org/10.4102/ajod.v6i0.300 [ Links ]
36. Hanass-Han cock J, Nene S, Deghaye N, Pillay S. "These are not luxuries, it is essential for access to life". Disability related out-of-pocket costs as a driver of economic vulnerability in South Africa. Afr J Disabil 2017;6:a280. https://doi.org/10.4102/ajod.v6i0.280 [ Links ]
37. Liu H, Hossain MS, Islam MS, et al. Understanding how a community-based intervention for people with spinal cord injury in Bangladesh was delivered as part of a randomised controlled trial. A process evaluation. Spinal Cord 2020;58(11):1166-1175. https://doi.org/10.1038/s41393-020-0495-6 [ Links ]
38. Chishtie J, Chishtie F, Yoshida K, Baiogh R. Spinal cord injury rehabilitation and pressure ulcer prevention after the 2005 South Asian Earthquake. A CBR case study from Pakistan. Disabil Rehabil 2019;41(14):1655-1663. https://doi.org/10.1080/09638288.2018.1445783 [ Links ]
39. Piatt JA, Nagata S, Zahl M, Li J, Rosenbluth JP. Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life. J Spinal Cord Med 2016;39(6)693-698.https://doi.org/10.1080/10790268.2015.1123845 [ Links ]
40. Mashola MK, Mothabeng DJ. Associations between health behaviour, secondary health conditions and quality of life in people with spinal cord injury. Afr J Disabil 2019;8:a463. https://doi.org/10.4102/ajod.v8i0.463 [ Links ]
41. Jorgensen S, Ginis K, Iwarsson S, Lexeli J. Depressive symptoms among older adults with long-term spinal cord injury. Associations with secondary health conditions, sense of coherence, coping strategies and physical activity. J Rehabil Med 2017;49(8):644-651. https://doi.org/10.2340/16501977-2259 [ Links ]
42. Cardenas DD, Jensen MP. Treatments for chronic pain in persons with spinal cord injury. A survey study J Spinal Cord Med 2006;29(2):109-117. https://doi.org/10.1080/10790268.2006.11753864 [ Links ]
 Correspondence:
Correspondence:
S Pilusa
sonti.pilusa@wits.ac.za
Accepted 18 August 2021














