Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.111 n.11 Pretoria Nov. 2021
http://dx.doi.org/10.7196/samj.2021.v111i11.15897
RESEARCH
Assessing South African medical interns' experience and confidence in managing obstetric emergencies
A C MillerI, II; F J L B MayanjaIII; J D PorterIV, V
IMB ChB, Dip HIV Man (SA); Department of Family Medicine and Rural Health, Faculty of Health Sciences, Walter Sisulu University, Mthatha, South Africa
IIMB ChB, Dip HIV Man (SA); Madwaleni District Hospital, Mbhashe sub-district, Eastern Cape Province, South Africa
IIIMB ChB, DTM&H, DPH, DHSM, MFamMed, BB&A, MBA; Department of Family Medicine and Rural Health, Faculty of Health Sciences, Walter Sisulu University, Mthatha, South Africa
IVMB ChB, MMed (Fam Med), FCFP; Department of Family Medicine and Rural Health, Faculty of Health Sciences, Walter Sisulu University, Mthatha, South Africa
VMB ChB, MMed (Fam Med), FCFP; Symphony Way Community Day Centre, Cape Town, South Africa
ABSTRACT
BACKGROUND: Medical doctors in South Africa (SA) are required to complete a 2-year internship at training hospitals, including a 4-month rotation in obstetrics and gynaecology. Following this, doctors are allocated to community service posts, many of which are at district- and primary-level facilities where supervision is limited. Recent triennial Saving Mothers reports identify district hospitals (DHs) as the second leading site for maternal deaths of all causes, the leading site for maternal deaths secondary to obstetric haemorrhage, and the most likely site for the lack of a skilled doctor to be identified as a factor in deaths associated with caesarean delivery
OBJECTIVES: To describe the self-perceived readiness of medical interns completing their training to manage obstetric emergencies, based on the Essential Steps in the Management of Obstetric Emergencies modules in the Health Professions Council of South Africa's internship logbook
METHODS: This cross-sectional descriptive study assessed medical interns in the last 3 months of their training, using a self-administered online questionnaire. Data collection took place between October and December 2019
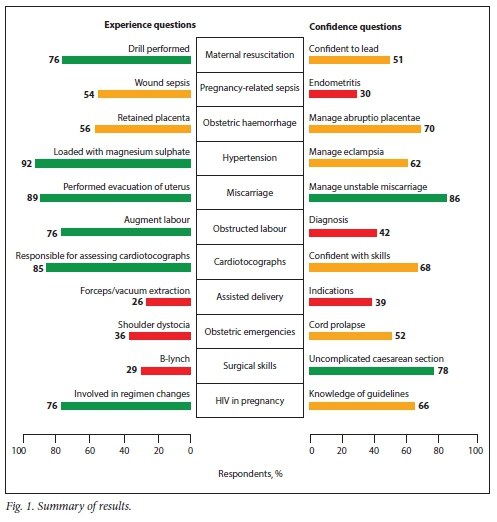
RESULTS: Cluster sampling of interns at training facilities throughout SA resulted in a total of 182 respondents from 17 hospitals in seven provinces in the country, with an overall response rate of 34.1%. Most interns had experience with and confidence in the management of miscarriage and hypertension in pregnancy. However, gaps in labour ward management, pregnancy-related sepsis and surgical skills were identified. Only 42.3% of respondents were confident in their ability to diagnose obstructed labour, 26.3% had performed an assisted delivery, 39.0% were confident in their knowledge of the indications for and contraindications to assisted deliveries, and 35.7% had been involved in the delivery of a baby with shoulder dystocia. Regarding pregnancy-related sepsis, 54.4% had experience with managing a wound abscess and 29.7% were confident managing puerperal endometritis. While 78.0% felt confident to perform a caesarean section (CS), only 28.6% had performed uterine compression suture for uterine atony at CS. Additionally, there was a statistically significant variation in scores between training hospitals
CONCLUSIONS: An incongruity exists between the shortcomings in DH obstetric services, the prioritisation of placement of community service doctors at primary healthcare facilities and DHs, and the self-perceived readiness of medical interns completing their training to manage obstetric emergencies safely. This situation highlights the importance of clinical support for junior doctors at DHs and standardisation of intern training at accredited facilities across SA
Medical doctors in South Africa (SA) are required to complete a 2-year internship at a training hospital as part of the qualification for independent practice, including a 4-month rotation in obstetrics and gynaecology. This rotation includes mandatory obstetric emergency training in the form of Essential Steps in the Management of Obstetric Emergencies (ESMOE) fire drills or prescribed ESMOE modules.[1] Following completion of medical internship, junior doctors are then allocated to community service posts. In contrast to the facilities where internship training is performed, the National Department of Health states in its guidelines for community service placement[2] that prioritisation should be given to filling community service medical officer posts at district hospitals (DHs) and primary healthcare (PHC) facilities.
The triennial Saving Mothers reports provide a valuable context to the challenges faced by these DHs and primary-level facilities. The 2014 - 2016 Saving Mothers report[3] published in 2017 identified DHs as the second leading site for maternal deaths of all causes after regional hospitals. DHs were the leading site for maternal deaths secondary to obstetric haemorrhage (OH), and lack of an appropriately trained doctor was identified as a factor in 31% of OH deaths occurring at DHs. Most importantly, the report states that 26% of maternal deaths associated with caesarean delivery occurred at DHs, where half of the cases identified the lack of a skilled doctor as an avoidable cause. This figure was higher than any other level of care.
Community service doctors may be placed at facilities that lack clinical supervision[4] or at facilities that may not offer a complete package of obstetric emergency services.[5] Subsequent to the medical internship programme being increased to 2 years, there have been two studies looking at the competency of post-internship practitioners. A 2008 cross-sectional study by Peters et al.[6] found that 73% of medical interns assessed themselves as competent in performing caesarean sections (CSs), and a 2012 cross-sectional study by Nkabinde et al.[7] found that community service doctors felt well prepared in all disciplines, but identified critical gaps in obstetrics, including labour ward emergencies and CS complications.
Given the challenges identified at DHs and PHC facilities in the Saving Mothers reports,'3,81 it is important to investigate in more detail and quantify the readiness of community service doctors to provide safe obstetric care at DHs and PHC facilities. Research into the readiness of medical interns completing their training to independently manage obstetric emergencies is lacking, despite policy that prioritises community service doctor placement in district- and primary-level facilities.
Objectives
To describe the experience level medical interns completing their internship have had in managing obstetric emergencies during their internship, and their confidence in managing these emergencies. We also compared the experience level and confidence of medical interns with the university where they studied, the current hospital at which they were completing internship, and the hospital level for internship training.
Methods
The study took the form of a cross-sectional descriptive study, using a self-administered online questionnaire. Data collection took place from October to December 2019. The study took place in SA, among medical interns in accredited training hospitals throughout the country where participants were completing their 2-year internship training programme.[2]
Participants
Approximately 1 800 medical doctors complete their internship each year,[9] the group doing so in 2019 forming the study population for this research. The majority of these medical interns subsequently enter community service posts for 1-year mandatory contracts as medical officers before registration for independent practice.[2] For the purposes of the research, the population was second-year internship candidates only, who were in the final 3 months of their internship training.
A cluster sampling technique was used, randomly selecting internship accredited training sites, alternating the levels of the hospitals to ensure a fair representation of interns from the variety of levels of care where interns are trained. Using the results of the study by Peters et al.,[6] where 73% of medical interns assessed themselves as competent in performing a CS, a target sample size of 260 participants was calculated. A response rate of 51% was expected, based on the results of previous research with similar data collection methods in community service doctors.[4] Sampling of facilities continued until a sample frame of a total number of >510 potential participants was obtained. With an expected response rate of 51%, a total of 260 participants was anticipated.
Procedure
The participants were recruited via an intern representative for each facility, who distributed the link to the online questionnaire and assisted with follow-up messages to ensure an adequate response rate. For each facility, response rates were monitored according to the number of reported second-year interns employed at the hospital.
The data collection consisted of an online questionnaire conducted using Google Forms.[10] The questionnaire could be completed within 5 minutes and was accessible on a standard smartphone, as well as on a tablet or computer. Informed consent for the questionnaire was obtained electronically at the start of the questionnaire.
No appropriate and validated data collection tool was available for this research. To ensure standardisation, topics for the questions were based on the list of ESMOE modules to be completed during internship, according to the Health Professions Council of South Africa (HPCSA)'s internship logbook. There are 12 modules in the logbook, one of which is neonatal resuscitation. The latter was excluded to keep the questionnaire focused on maternal factors. The remaining 11 modules were: (i) maternal resuscitation; (ii) sepsis; (iii) obstetric haemorrhage; (iv) pre-eclampsia/ eclampsia; (v) miscarriage; (vi) partograms and obstructed labour; (vii) cardiotocographs (CTGs); (viii) assisted deliveries; (ix) obstetric emergencies; (x) surgical skills; and (xi) HIV in pregnancy.
Two questions were formulated per the ESMOE module, based on a core skill or knowledge component in the drill and accompanying lecture material associated with each module. Each question focused on assessing either the participants' confidence or their experience relating to a particular core skill or knowledge component in each module. The questions were not aimed at testing the participants' knowledge of that topic or skill.
A conventional level of significance of alpha = 0.05 (5%) was used, and confidence intervals were therefore set at 95%. The level of significance was p<0.05. All data were analysed using Excel 2019 (Microsoft, USA) and Stata 15 (StataCorp, USA). Ethics approval was obtained from the Walter Sisulu University Faculty of Health Sciences Post Graduate Education, Training, Research and Ethics Unit on 16 September 2019 (ref. no. 063/2019).
Results
A total of 17 hospitals in 7 provinces were randomly selected in the sample, with the hospitals reporting a total of 534 second-year interns employed and therefore potential respondents. Of these, 212 interns answered the online questionnaire. After applying exclusion criteria to remove respondents who had completed the questionnaire despite being in their first year of training, 182 respondents remained for analysis. The final overall response rate was 34.1%. Reponse rates varied between facilities, ranging from 11.4% to 83.3% (Table 1).
Data on the university at which undergraduate training had been completed were collected to assist with analysis. Candidates from all eight SA medical schools were represented.
Respondents were asked 11 questions regarding their experience with or exposure to certain obstetric conditions or procedures, as related to the ESMOE modules to be completed according to the HPCSA internship logbook. These questions and responses are detailed in Table 2.
Respondents were asked 11 questions regarding their confidence to manage certain obstetric conditions or procedures, as related to the ESMOE modules to be completed according to the HPCSA internship logbook. They were asked to rate their confidence on a Likert scale (strongly agree, agree, neutral, disagree and strongly disagree) in response to a statement regarding their confidence to manage a certain scenario. These questions are detailed in Table 3. In describing these data, Likert scales were binarised to be represented as either confident or not confident. Confidence was interpreted when the respondent agreed or strongly agreed with the statement.
A summary of the results arranged by ESMOE topic is presented in Fig. 1, including scores for both experience and confidence questions.
In keeping with the objectives of the study, the experience level and the confidence of respondents were compared with the current hospital for internship training, the level of the hospital, and the university at which they had studied. In these comparisons, Likert scales for confidence scores were kept at the original scale of 1 - 5 (strongly disagree to strongly agree). This was done to avoid loss of detail in the data, with the Likert scale converted to numerical values (1 - 5) when analysing. For each comparison, a one-way analysis of variance test was performed to look for significance in the variation of the means between groups. If a significant difference was found, further analysis using a Bonferroni test was done to compare facilities individually.
The hospital level did not significantly affect results, with scores similar between hospital levels for both experience questions (p=0.36) and confidence questions (p=0.71). Similarly, there was no significant difference in the scores between different universities for both experience questions (p=0.32) and confidence questions (p=0.11).
When comparing the current hospital for internship training with those hospitals' scores in the experience and confidence questions, greater variation was seen. Statistically significant variation was seen between hospitals for both experience scores (p=0.00) and confidence scores (p=0.001). While there was variation in the scores for both experience and confidence between hospitals, the total numbers of respondents for most hospitals were too low for those differences to be statistically significant. However, one hospital scored significantly lower than six other hospitals for experience scores and significantly lower than three others for confidence scores.
Discussion
Strengths were noted in the management of hypertension in pregnancy, miscarriages and HIV in pregnancy. Areas with lower scores included OH, surgical skills and pregnancy-related sepsis. Regarding OH, 56.0% of respondents had experience with manually removing a retained placenta and 69.8% were confident with managing a patient presenting with abruptio placentae. The 2014 - 2016 Saving Mothers report[3] identified OH as the third leading cause of maternal mortality, with DHs the most likely site of deaths due to OH.
Further investigating surgical skills, 78.0% of respondents felt confident to perform a CS, but only 28.6% had performed a uterine compression suture for uterine atony at CS. It is encouraging to see that interns felt comfortable to perform a CS, probably as a result of this procedure being prioritised in the HPCSA internship logbook. However, considerably fewer had performed a uterine compression suture, suggesting that interns are probably preferentially exposed to low-risk CSs in their training. With the possibility of even low-risk CSs becoming complicated, the importance of experience in managing these complications is apparent.
This discrepancy between the confidence of interns to perform an uncomplicated CS and their potential lack of exposure to complicated CSs illuminates a concerning shortcoming in the current training programme.
Regarding pregnancy-related sepsis, while 54.4% of respondents had experience with managing a wound abscess post CS, only 29.7% were confident regarding the management of puerperal endometritis. The 2014 - 2016 Saving Mothers report[3] noted with concern the high proportion of avoidable deaths that occurred due to pregnancy-related sepsis.
Responses to questions related to ESMOE modules pertaining to labour ward management and CSs were important to note. The 2014 - 2016 Saving Mothers report[3] states that 26% of maternal deaths associated with caesarean delivery occurred at DHs, with an institutional maternal mortality ratio three times higher for caesarean delivery than vaginal birth in these facilities. Reducing unnecessary CSs, and specifically avoiding unnecessary high-risk CSs, is essential. The experience and confidence of interns to manage labour and make decisions around delivery is therefore of interest.
Of note here, only 42.3% of respondents were confident in their ability to diagnose obstructed labour, 26.3% had performed an assisted delivery, 39.0% were confident in their knowledge of the indications for and contraindications to assisted deliveries, and 35.7% had been involved in delivery of a baby with shoulder dystocia. Marginally better, 51.7% were confident in their ability to manage cord prolapse and 67.6% were confident in their ability to interpret CTGs. Furthermore, 85.2% had been responsible for assessing CTGs during their internship, and 76.4% had augmented patients in labour with oxytocin during their internship.
When comparing responses to the questions with the university trained at, the level of hospitals trained at and the specific hospital trained at, low numbers of total respondents over many different universities or hospitals make it difficult to draw statistically sound conclusions. However, there was statistically significant variation in how respondents from different training hospitals answered both experience and confidence questions, with one facility scoring significantly lower than several others. This finding highlights the importance of increased efforts to standardise the training at internship-accredited facilities across the country.
Starting from 2021, the 2-year internship training programme includes increased time spent in PHC facilities, with 6 of the 24 months spent at DHs, community health centres and PHC clinics as part of a prolonged family medicine rotation.[11] This increased exposure to PHC comes at the expense of 1 month of obstetrics and gynaecology exposure, with the rotation reduced from 4 to 3 months to accommodate the change. The new 6-month rotation may include some obstetrics exposure, but that is not mandatory. However, the Saving Mothers reports[3,8] note with concern the lack of appropriately trained doctors and the health worker-related avoidable factors identified in maternal deaths in these PHC facilities and DHs.
Nevertheless, most internship obstetric training will continue to be at the same accredited training facilities as occurs at present. As these internship training facilities are required to provide specialist services, many facilities are also a training site for registrars. However, medical interns are not just junior registrars in waiting, but rather represent an important group of doctors who are being trained for an altogether different environment to that in which many of the registrars will work. Unlike the registrars, these junior doctors may soon be required to work without the immediate availability of specialist support, and often with more severe resource constraints than at their internship facilities. They may not be able to refer patients easily or have access to support that will allow them to make experienced decisions that reduce the risk of complications which they may not be equipped to handle.
This research was limited by low response rates, and potential for response bias therefore exists. Nevertheless, the 182 respondents represent a higher number of study participants than have been included in relevant literature prior to this. Additionally, this research relied on participants' self-reported experience and confidence, rather than assessing actual competence. Regarding the provincial distribution of participants, the nature of cluster sampling meant that certain provinces were under- or over-represented. Specifically, there were no respondents who were completing their internship in Limpopo and North West provinces.
Further research into the readiness of junior doctors to practise safe obstetrics is needed, especially considering the current changes to the internship training programme. Together with the research presented here, future research can better describe the outcomes of current internship training, and thus ensure greater congruency between the training of medical interns and the expectations placed on community service and junior doctors. Additionally, research into the role of DH family physicians in ensuring ongoing training of junior doctors and addressing the avoidable factors identified in the Saving Mothers reports would complement this research.
With the increased prioritisation of community service doctor placement at DHs and PHC facilities, this research strengthens the findings of previous literature in showing the relative lack of skills available in these settings. Clinical support in the form of senior medical officers, family physicians and district clinical specialist teams is therefore essential.
Conclusions
This research aimed to describe the self-perceived readiness of medical interns completing their training to independently manage obstetric emergencies, based on the ESMOE modules in the HPCSA internship logbook. A significant variation between internship-accredited hospitals in the self-perceived readiness of medical interns to practise safe obstetrics was found. Specific experience and confidence gaps in labour ward management, pregnancy-related sepsis and compression sutures for uterine atony were identified. Strengths were identified in the management of miscarriage, performing an uncomplicated CS and the management of hypertension in pregnancy.
An incongruity exists between the shortcomings in DH obstetric services as identified in the Saving Mothers reports, the prioritisation of placement of community service doctors at PHC facilities and DHs, and the self-perceived readiness of medical interns completing their training to safely manage obstetrics and reduce preventable maternal mortality. It is therefore important that internship training hospitals and the HPCSA adjust their programmes accordingly. Interns in their obstetrics and gynaecology rotations need prioritisation given to developing life-saving skills while these can be learnt in an environment with specialist support. Additionally, considering the lack of experience and confidence identified in this research, it becomes essential that senior medical doctors and on-site family physicians are attracted to and retained in PHC facilities and DHs where they will be able to support junior doctors, together with district clinical specialist obstetricians.
Declaration. The research for this study was done in partial fulfilment of the requirements for ACM's MMed (Family Medicine) degree at Walter Sisulu University.
Acknowledgements. The authors acknowledge the intern co-ordinators and representatives and their role in recruitment of participants. They also thank the staff of the Department of Family Medicine and Rural Health, Walter Sisulu University, for support and guidance.
Author contributions. ACM is the primary author. JDP and FJLBM supervised the study and contributed to the writing of the manuscript.
Funding. The National Research Foundation contributed funding to this research.
Conflicts of interest. None.
References
1. Health Professions Council of South Africa. Handbook on internship training: Guidelines for interns, accredited facilities and health authorities. Pretoria: HPCSA, 2017. http://www.hpcsa-blogs.co.za/wp-content/uploads/2017/04/2017-IN-Handbook-Part-I-and-II.pdf (accessed 2 May 2019). [ Links ]
2. National Department of Health, South Africa. Internship and community service placement guidelines 2017/2018. Pretoria: NDoH, 2017. https://www.kznhealth.gov.za/internship-and-community-service-placement-guidelines-for-2017-2018.pdf (accessed 3 November 2018). [ Links ]
3. National Committee on Confidential Enquiries into Maternal Deaths. Saving Mothers 2014 - 2016: Seventh triennial report on confidential enquiries into maternal deaths in South Africa. Pretoria: 2018. https://www.westerncape.gov.za/assets/departments/health/saving_mothers_2014-16_-_short_report.pdf (accessed 5 November 2018). [ Links ]
4. Reid SJ, Peacocke J, Kornik S, Wolvaardt G. Compulsory community service for doctors in South Africa: A 15-year review. S Aft Med J 2018;108(9):741-747. https://doi.org/10.7196/SAMJ.2018.v108i9.13070 [ Links ]
5. Pattinson RC, Makin JD, Pillay Y, van den Broek N, Moodley J. Basic and comprehensive emergency obstetric and neonatal care in 12 South African health districts. S Afr Med J 2015;105(4):256-260. https://doi.org/10.7196/SAMJ.9181 [ Links ]
6. Peters F, van Wyk J, van Rooyen M. Intern to independent doctor: Basic surgical skills required for South African practice and interns' reports on their competence. S Afr Fam Pract 2015;57(4):261-266. https://doi.org/10.1080/20786190.2014.976954 [ Links ]
7. Nkabinde TC, Ross A, Reid S, Nkwanyana NM. Internship training adequately prepares South African medical graduates for community service - with exceptions. S Afr Med J 2013;103(12):930-934. https://doi.org/10.7196/SAMJ.6702 [ Links ]
8. National Committee on Confidential Enquiries into Maternal Deaths. Saving Mothers 2011 - 2013: Annual report and detailed analysis of maternal deaths due to non-pregnancy related infections. Pretoria: 2014. https://www.westerncape.gov.za/assets/departments/health/saving_mothers_2011-13_-_comprehensive_report.pdf (accessed 5 November 2018). [ Links ]
9. Masweneng K. Internship placement delay causing headache for medical graduates. Times Live, 29 November 2017. https://www.timeslive.co.za/news/south-africa/2017-11-29-internship-placement-delay-causing-headache-for-medical-graduate (accessed 6 November 2018). [ Links ]
10. Google. Google Forms. 2020. https://docs.google.com/forms/ (accessed 16 January 2020). [ Links ]
11. Luke B. Medical internship training in South Africa: 2020 and beyond: A transformational plan for health service delivery Pretoria: Health Professions Council of South Africa, 2019. https://www.hpcsa.co.za/Uploads/Events/Conference/day%202/19Aug-3E-13h40-13h55_Binu_Luke.pdf (accessed 21 September 2020). [ Links ]
 Correspondence:
Correspondence:
A C Miller
mr.acmiller@gmail.com
Accepted 26 July 2021














