Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.111 no.11 Pretoria Nov. 2021
http://dx.doi.org/10.7196/samj.2021.v111i11.15913
RESEARCH
Post-laryngectomy simplified dysphagia score (SDS) tool: Potential for screening and comparison with the swallowing outcomes after laryngectomy (SOAL) tool
R A BloklandI; A J Bruce-ChwattII; J W LoockIII
IMB ChB; Division of Otorhinolaryngology, Department of Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIMD, PRCS; Division of Plastic and Reconstructive Surgery, Department of Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIPCS (SA) ORL; Division of Otorhinolaryngology, Department of Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Our understanding of swallowing disorders after laryngectomy remains limited. A literature search found that documentation of swallowing function in the laryngectomee population is lacking. Furthermore, no consensus exists regarding a suitable evaluation tool to assess swallowing function. While conventional questionnaires are time consuming, cost and time constraints make regular objective swallowing investigations impractical
OBJECTIVES: To develop a 2-question simplified dysphagia score (SDS) screening tool for routine documentation of swallowing function at post-laryngectomy follow-up visits, and to test this new tool against an established dysphagia measuring tool for laryngectomees. We also sought to identify risk factors for poor swallowing outcomes
METHODS: Cross-sectional surveys were used to compare results obtained from the validated swallowing outcomes after laryngectomy (SOAL) questionnaire and our novel SDS tool. The components of the SDS were guided by the experience and expertise of surgeons and speech therapists, as well as insights from patients and their families. Sixty laryngectomy patients (females, n=7; males, n=53) were enrolled in the study. All patients were >18 years of age. Each participant was asked to complete the SDS and the SOAL questionnaires. The results of each tool were compared using non-parametric tests, with multiple pairwise comparisons using Bonferroni tests
RESULTS: Both sets of results showed a linear relationship using the Kruskal-Wallis non-parametric analysis of variance (ANOVA) test. The SDS had a specificity of 96% (95% confidence interval (CI) 76 - 100%), a sensitivity of 81% (CI 64 - 91%), a positive predictive value of 97% (CI 81 - 100%) and a negative predictive value of 76% (CI 56 - 89%) against the SOAL scores. The SDS results yielded 7 false-negative and 1 false-positive result for dysphagia compared with the SOAL questionnaire. Outcomes of the secondary objectives did not reach statistical significance
CONCLUSIONS: The SDS is a 2-question, practical grading system that shows a statistically significant correlation with the recognised SOAL questionnaire, making it a useful alternative for everyday use, which provides outcome scores of direct practical value to patient and clinician. Prospective use of the SDS and higher patient numbers may allow a better understanding of dysphagia, its causes and risk factors
Total laryngectomy (TL) is the surgical removal of the entire larynx. The remaining surgical defect in the pharynx is closed primarily or, if necessary, with different types of pedicled or free flaps, depending on the size of the defect. This major disruption of the anatomy and function of the pharynx may affect physiological processes, which impact on the quality of life (QoL), including loss of speech and dysphagia[1]
In patients with laryngeal cancer who undergo TL, the focus is on successful disease removal. While speech rehabilitation also receives adequate attention, swallowing after TL tends to be neglected even though significant dysphagia can result in diminished QoL, compromised nutrition and a decrease in social participation.[1]
Internationally, reports on the prevalence of post-TL dysphagia vary widely, from 10% to 70%, possibly due to disparate definitions of dysphagia and the use of different measurement tools.[1-3] Until now, the prevalence of dysphagia following TL in our institution was unknown, and patients' swallowing status was not routinely documented at follow-up visits. We therefore investigated post-TL dysphagia in our population.
We suggest that a significant obstacle to the study of dysphagia and its many causes and effects in the post-TL setting is the absence of routine documentation of patients' swallowing status and the lack of a universal descriptive language. Although a number of nonspecific swallowing-assessment tools are described in the literature, including imaging studies and patient-reported outcome measures (PROMs) in the form of questionnaires,[4,5]very few relate to post-TL dysphagia.
Some researchers have attempted to develop methods to quantify dysphagia in the form of PROMs, but none is used commonly.[1,6-10] We suggest that this is due to the methods being relatively complex and time consuming. Additionally, while some of these tools have value in assessing known dysphagia patients, where the aim of the evaluation is to determine the cause and severity of the swallowing impairment and to guide the selection of an effective treatment, they are less practical for use as quick screening tools.
In many settings, communication barriers make the routine application of questionnaires difficult and impractical. These barriers include speech difficulty after laryngectomy, multilingualism and absence of translation services, compounded by illiteracy and socioeconomic hindrances to mutual understanding.[11] Within this context, the objective of our study was to develop and investigate a simple and practical dysphagia screening tool, i.e. the simplified dysphagia score (SDS), for documenting dysphagia after TL, including its prevalence and severity and the causative factors.
To test the appropriateness of the SDS, we compared its outcomes with those of the swallowing outcome after laryngectomy (SOAL) questionnaire, an established measurement tool developed and preliminarily validated in 2012,[10] followed by full psychometric validation in 2015.[12] The SOAL was identified from the literature as being methodologically robust and the only questionnaire specifically developed to assess swallowing after TL. While impractical as a routine screening tool in our busy clinics, it did present a good exemplar against which to measure the validity of the developed SDS.
Secondarily, we collected data to identify the associations, causes and contributing factors in the development of dysphagia Potential risk factors for poor postoperative swallowing function were investigated by correlating the results obtained with each tool (SDS and SOAL) with variables that possibly affect swallowing function, including pathological T-stage of disease, pharyngeal closure technique and time since surgery.
T-stage refers to the extent of the primary tumour according to the TNM (tumour, nodes, metastasis) classification of malignant tumours and is specifically defined for each cancer subsite, depending on characteristics such as size, extent and specific structure involvement.[13] This assessment can be clinical (before surgery) or pathological (after surgery). The pathological T-stage refers specifically to the final assessment of these characteristics after surgery and histological examination of the excised specimens.
During a TL procedure, the choice of pharyngeal closure technique depends on the size of the pharyngeal defect after removal of the tumour. The surgeon assesses whether sufficient pharyngeal tissue remains to create an adequate neopharynx by primary closure or whether tissue will have to be imported by using a free or pedicled flap. Options for primary closure also partly depend on the surgeon's preference, which includes suturing the defect horizontally, vertically or in a T-closure (a combination of horizontal and vertical suturing). Theoretically, this may affect the internal diameter of the neopharynx which would influence swallowing function.
It is well known that radiotherapy may cause mucositis and fibrosis over time.[14] It can, therefore, be expected to impact on swallowing function when used to treat laryngeal disease. However, because most of our patients received adjuvant radiotherapy as part of their treatment, the number of patients who did not receive such therapy was too small to allow us to study this variable and its impact on swallowing function.
Methods
Patient surveys
We conducted a cross-sectional survey comparing two patient-reported outcome tools, i.e. SOAL (established and validated) and SDS (novel). Therefore, the survey represented a validation study for the newly developed dysphagia-screening instrument.
Every patient who attended a TL follow-up clinic and/or support group meeting at our institution over a period of 1 year was asked to participate in our study. All agreed, and a total of 60 patients (females, n=7; males, n=53) received counselling as stipulated in our consent form. All respondents gave permission for their questionnaire responses and data from their files to be used for research purposes.
All study participants were > 18 years of age, had previously had a TL for laryngeal squamous cell carcinoma (SCC) and were disease free at the time of participation. Each participant was asked to complete both the SDS and SOAL questionnaires in English, Afrikaans or Xhosa, depending on the language he/she was most comfortable with. Translations were supplied by an official translating service. Informal verbal interpreters, including family members and staff, were used if participants were illiterate or preferred a language other than those mentioned above. No patients were excluded based on language, as we were able to communicate adequately with all participants.
Data for the secondary objectives, i.e. pathological tumour stage, pharyngeal closure technique and time since surgery, were collected from patients' files and recorded on their respective questionnaire forms. All data sheets were stored securely and were only accessible to the involved researchers.
Dysphagia scores were quantified separately by each tool (SOAL and SDS) and results were compared using non-parametric tests, with multiple pairwise comparisons using Bonferroni tests. Furthermore, secondary objective variables were analysed according to the dysphagia scores of both tools.
SOAL questionnaire
The SOAL questionnaire consists of 17 statements, each describing an aspect of dysphagia. Respondents were required to indicate whether the statement applied to him/her with 'no', 'a little' or a lot' and scores were then allocated as 0, 1 and 2, respectively. Thus, respondents obtained a total score between 0 and 34, with 0 representing normal swallowing function and 34 reflecting the most severe form of dysphagia. For the purpose of our study and for comparison with the developed SDS, we identified a threshold score that separated patients with normal swallowing function from those with clinically significant dysphagia.
One of the problems associated with the SOAL questionnaire is that it does not provide a cut-off value for the diagnosis of dysphagia. Govender et al.[10] comment on the development of the SOAL questionnaire by stating that 'a patient with no adverse features on modified barium swallow would have a predicted SOAL score of (approximately) 5, whereas a patient with all adverse features on all boluses would have a predicted score of (approximately) 34'. Based on this, we interpreted the SOAL results as follows: <5 - normal swallowing; >5 - dysphagia.
SDS
The SDS was designed in consultation with 2 speech pathologists, 6 otorhinolaryngology consultants and 1 plastic and reconstructive surgeon, all with experience in dysphagia and the post-TL patient population. Content was also adjusted according to information gained from a pilot study and interactions with patients and their close relatives.
The developed SDS is based on identifying the consistency of food closest to normal' that the patient can eat, as well as whether the patient can manage the diet with ease or difficulty. The questionnaire comprises 5 levels for types of food tolerated, with sub-levels A or B for ease of eating each food type. Types of food tolerated:
• normal diet with no restrictions
• mostly normal diet with some restrictions
• soft/mashed food only, e.g. porridge or mashed potatoes
• thick liquid diet, e.g. soup, milkshakes or supplement drinks
• thin fluids only, e.g. juice, water
• saliva only
Sub-levels:
• no difficulty - no second swallow/no water required
• with difficulty - second swallow required/needs water/takes a long time.
Together, the levels offer a categorical score that inherently contains valuable practical information for the clinician. The scores progress from 1A, IB, 2A, 2B, 3A ... and so on. Again, for comparison with the SOAL tool, we required a threshold score to identify clinically significant dysphagia. Considering that a completely normal diet with no restrictions would allow for the least nutritional disturbance, we used any score of > 1 as representative of dysphagia.
Statistical analyses
Data were analysed using SPSS version 26 (IBM Corp., USA), with p<0.05, indicating statistical significance. Furthermore, Kruskal-Wallis non-parametric analysis of variance (ANOVA) tests were used to compare median SOAL scores across SDS grades, with multiple pairwise comparisons using the Bonferroni correction for multiple tests. Results of SDS-assessed dysphagia were cross-tabulated against those of SOAL-assessed dysphagia. Sensitivity, specificity, as well as negative and positive predictive values, were calculated along with their 95% confidence intervals (CIs).
Risk factors were plotted against the presence or absence of dysphagia according to both methods, and Fischer's exact test was performed. Time since surgery was compared in the dysphagia groups using the non-parametric Mann-Whitney test.
Ethical approval
Ethical approval for the research was obtained from the Stellenbosch University Health Research Ethics Committee 2 (ref. no. S19/01/015).
Results
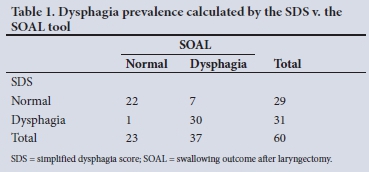
We assessed 60 patients at post-TL follow-up clinics in a single institution between January and July 2019. The overall prevalence of dysphagia among these patients using the SOAL questionnaire was 61.7% (n=37) and using the SDS it was 51.7% (n=31).
Accepting the SOAL questionnaire as the gold standard, the SDS results yielded 1 false-positive and 7 false-negative results for dysphagia. Furthermore, our results showed the SDS to have a sensitivity of 81% (CI 64 - 91%), a specificity of 96% (CI 76 - 100%), a positive predictive value of 97% (CI 81 - 100%) and a negative predictive value of 76% (CI 56 - 89%) against the SOAL questionnaire (Table 1).
The median SOAL score was statistically significantly different between the SDS grade categories (p<0.001). Although our results showed a linear trend in the median increase across SDS grades (Fig. 1), the Bonferroni correction after multiple comparison testing showed that the differences were only found in the extreme categories, i.e. category 1A differed from 2B and 3B, and IB differed from 3B. The remaining pairwise comparisons were not statistically significant.

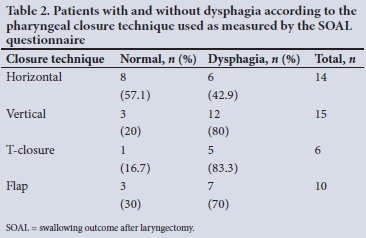
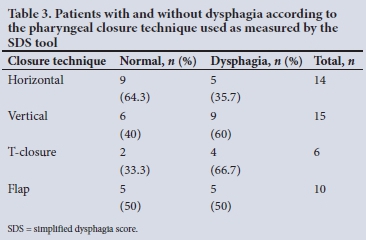
An examination of the variables believed to have an impact on post-TL dysphagia was undertaken and included the pathological T-stage, pharyngeal closure technique used and time since surgery. However, none of these reached statistical significance in their associations with dysphagia by either method. According to both tools, the pharyngeal closure technique plotted against dysphagia showed a slight trend towards better outcomes with horizontal closure, but statistical significance was not attained (Tables 2 and 3). Neither pathological T-stage nor time since surgery showed an impact on the presence of dysphagia.
Discussion
Primary objectives
The prevalence of dysphagia was 61.7% using the SOAL questionnaire, and 51.7% using the SDS tool. However, these results were obtained by accepting the cut-off scores (>5 for SOAL and >1B for SDS) that separated patients with problematic dysphagia from those with acceptable swallowing function. This division is, at best, an educated estimate based on clinical experience. More accurate cut-offs are impossible to deduce before the clinical entity of dysphagia is better understood and precise definitions are established.
The trend towards a linear relationship between the results obtained from the two measurement tools and the good sensitivity and specificity of the SDS against the SOAL, suggest that the SDS is a reasonable substitute for the SOAL questionnaire. Although the trend does not directly indicate the accuracy of the SDS for dysphagia screening, it does imply that the SDSs correlate with the scores obtained from the SOAL, which has been rigorously developed and validated. We suggest that the SDS can be presumed to be as adequate as the SOAL for the detection and grading of dysphagia in the laryngectomee population.
Secondary objectives
We investigated a number of variables believed to impact on dysphagia after TL, including the pathological T-stage, pharyngeal closure technique and time since surgery.
However, none of these variables reached statistical significance, and we conclude that higher patient numbers are needed to confidently assess the effect of these variables on dysphagia.
Our results do not indicate a clear trend towards higher levels of dysphagia among any particular tumour stage, and statistical significance was not reached. Similarly, when dysphagia was assessed across pathological tumour stages using the SDS, no trends could be identified among the patients in our study, and statistical significance was not reached. According to both tools, the pharyngeal closure technique plotted against dysphagia showed a slight trend towards better outcomes with horizontal closure, but statistical significance was not attained. Time since surgery did not seem to have an impact on the presence of dysphagia, but higher patient numbers are needed to confirm this with statistical significance.
Conclusions
Results from the developed SDS showed high sensitivity and specificity when compared with the SOAL questionnaire, and we believe that this makes it acceptable to use for routine documentation of swallowing function after laryngopharyngectomies. The intention of this comparison was to establish whether the SDS is at least as useful as the most appropriate existing tool to assess swallowing in post-TL patients.
As the SDS is easy to use and can be completed in <1 minute, it can be implemented at every patient visit and provides the clinician with a clear image of the patient's swallowing status. It is amenable to wider adoption as a universal post-TL dysphagia screening tool and may be a suitable method for the routine recording of dysphagia.
The questions in the SDS inherently provide information regarding the effect of dysphagia on patients' lives. For example, a patient with a level 2A score or higher, can eat with minor modifications and participate socially, while a level 4B patient has to spend most waking hours sipping at food to maintain an adequate nutritional status. By routinely documenting patients' swallowing status at follow-up visits, we hope to establish a significant database from which to conduct further retrospective research into risk factors, associations and causes of dysphagia after TL.
We acknowledge the need for a more detailed analysis that comes with the SOAL questionnaire when treating patients with dysphagia. We suggest that the SDS be used for routine screening at follow-up visits of laryngectomees to identify patients who require further management. SOAL can then be used in the management of these patients to further explore the details of the individual patient's problem.
Further validation studies comparing the SDS to imaging studies, such as videofluoroscopy, will be useful. Additionally, we hope that with the wider use of the SDS and retrospective analyses, it will be possible to obtain statistically significant answers to our questions regarding the causative factors of dysphagia after TL.
Study limitations
The SDS was not directly compared with imaging investigations. Greater patient numbers would be required to determine the possible roles of variables that might contribute to dysphagia. The comparison between the two PROMs only indicates that the SDS as a measurement tool is as sound as the SOAL questionnaire. Although we acknowledge that the correlation between the tools is not exact, we suggest that it is sufficient to accept the SDS as a valuable tool to screen for swallowing problems. Higher patient numbers would be needed to establish a better correlation between the SOAL and SDS.
Declaration. The research for this study was done in partial fulfilment of the requirements for RAB's MMed (ORL) degree at Stellenbosch University.
Acknowledgements. We acknowledge the help of Candice Randall, Leanie Engelbrecht and Dr Gary Kroukamp.
Author contributions. RAB: concept development, literature review, pilot study execution, data collection, statistical analyses and write-up; AJB-C: concept development, statistical analyses and write-up; and JWL: concept development and write-up.
Funding. None.
Conflicts of interest. None.
References
1. Maclean J, Cotton S, Perry A. Post-laryngectomy. Its hard to swallow. Dysphagia 2008;24(2):172-179. https://doi.org/10.1007/S00455-008-9189-5 [ Links ]
2. Frowen J, Perry A. Speech and swallowing functions in head and neck cancer patients. What do we know? Cancer Forum 2006;30(3):178-183. [ Links ]
3. Ward EC, Bishop B, Frisby J, Stevens M. Swallowing outcomes following laryngectomy and pharyngolaryngectomy Arch Otolaryngol Head Neck Surg 2002;128(2):181-186. https://doi.org/10.1001/archotol.l28.2.181 [ Links ]
4. Coffey M, Tolley N. Swallowing after laryngectomy Curr Opin Otolaryngol Head Neck Surg 2015;23(3):202-208. https://doi.org/10.1097/MOO.0000000000000162 [ Links ]
5. Patel DA, Sharda R, Hovis KL, et al Patient-reported outcome measures in dysphagia. A systematic review of instrument development and validation. Dis Esophagus 2017;30(5):1-23. https://doi.org/10.1093/dote/dow028 [ Links ]
6. Armstrong E, Isman K, Dooley P, et al. An investigation into the quality of life of individuals after laryngectomy Head Neck 2001;23:16-24. https://doi.org/10.1159/000103870 [ Links ]
7. Nguyen NP, Vos P, Karlsson U, et al. Quality of life following chemoradiation and postoperative radiation for locally advanced head and neck cancer. ORL J Otorhinolaryngol Relat Spec2007;69(5):271-276. https://doi.org/10.1159/000103870 [ Links ]
8. Oozeer N, Owen S, Perez B, Jones G, Welch A, Paled V Functional status after total laryngectomy. Cross-sectional survey of 79 laryngectomees using the performance status scale for head andneck cancer. J Laryngol Otol 2009;124(04):412-416. https://doi.org/10.1017/s0022215109992192 [ Links ]
9. Chen A, Frankowski R, Bishop-Leone J, et al Lhe development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer. Lhe M D Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg 2001;127(7):870-876. [ Links ]
10. Govender R, Lee ML, Davies LC, et al. Development and preliminary validation of a patient-reported outcome measure for swallowing after total laryngectomy (SOAL questionnaire). Clin Otolaryngol 2012;37(6):452-459. https://doi.org/10.llll/coa.12036 [ Links ]
11. Edwards BL, Greeff LE. Exploring grassroots feedback about cancer challenges in South Africa. A discussion of themes derived from content thematic analysis of 316 photo-narratives. Pan Afr Med J 2017;28:173. https://doi.org/10.11604%2Fpamj.2017.28.173.11894 [ Links ]
12. Govender R, Lee ML, Davies LC, et al Psychometric evaluation of the swallowing outcomes after laryngectomy (SOAL) patient-reported outcome measure. Head Neck 2015;38:E1639-E1645. https://doi.org/10.1002/hed.24291 [ Links ]
13. Laryngeal cancer stages. https://www.cancer.org/cancer/laryngeal-and-hypopharyngeal-cancer/detection-diagnosis-staging/staging.html (accessed 15 October 2021). [ Links ]
14. Rancati L, Schwarz M, Allen A, et al. Radiation dose volume effects in the larynx and pharynx. Int J Radiat Oncol Biol Phys 2010;76(3):64-69. https://doi.org/10.1016/j.ijrobp.2009.03.079 [ Links ]
 Correspondence:
Correspondence:
RA Blokland
rachelblokland@gmail.com
Accepted 10 August 2021














