Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.111 n.10 Pretoria Oct. 2021
http://dx.doi.org/10.7196/samj.2021.v111i10.15915
CORRESPONDENCE
Children have been left behind during the HIV 90-90-90 strategy implementation in South Africa
To the Editor: Worldwide, children still lag in accessing HIV services,[1] despite the Sustainable Development Goals and the UNAIDS 95-95-95 strategy highlighting the critical need for focus on children and adolescents.[2] By 2020, only half (53%) of HIV-infected children globally were on antiretroviral therapy (ART), compared with two-thirds (68%) of adults.[1] This discrepancy also exists in South Africa (SA). In 2019, among adults, 93% had known HIV status, and 71% of those who were positive were recipients of ART, with 61% virally suppressed. Children had much lower rates: 77%, 63% and 63%, respectively.[3,4]
Recent City of Johannesburg data indicate that children on ART had constantly lower viral load suppression rates compared with adults throughout the 90-90-90 strategy implementation period.[5]
Case-finding has received priority attention from SA health services and international funders.[6] However, poor retention in care and inadequate viral suppression threaten programme success. Left unattended, this situation leads not only to high morbidity and mortality in children but also to the development of a cohort of young adults with high levels of drug resistance, placing control of the epidemic at risk.
Challenges to retention and adherence to ART in children include child-unfriendly ART formulations (such as unpalatable or large-volume syrups), non-availability of fixed-dose combinations, and formulations requiring refrigeration.[7] Inadequate supervision and poor health literacy of caregivers, poor caregiver-child relationships and support systems, and non-disclosure to the child and other family members of his/ her HIV-positive status further hinder adherence.[8,9]
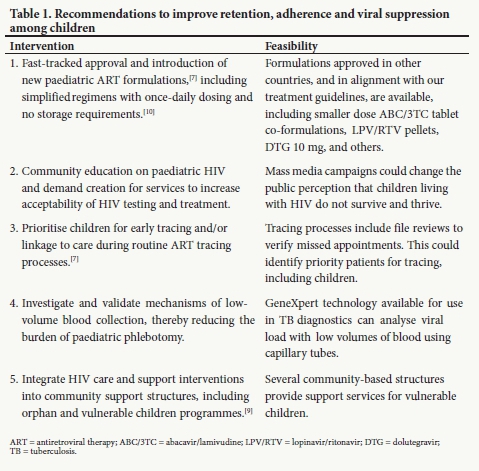
We have to do more to ensure that children are initiated on ART, remain in care, and achieve virological suppression. We suggest five key interventions that can change the trajectory of HIV care for SA children (Table 1).
J C Y Nyasulu
Division of Health Systems and Public Health, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa; Division of Community Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; AFRIQUIP Health Systems, Johannesburg, South Africa julietnyasulu@gmail.com
J Dunlop
Division of Community Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; Anova Health Institute, Johannesburg, South Africa
H Pandya, W Slemming
Division of Community Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
C Fick
Division of Community Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; Wits Reproductive Health and HIV Institute, University of the Witwatersrand, Johannesburg, South Africa
H Saloojee
Division of Community Paediatrics, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
References
1. Joint United Nations Programme on HIV and AIDS (UNAIDS). 2020 global AIDS update - Seizing the moment - Tackling entrenched inequalities to end epidemics. 6 July 2020. https://www.unaids.org/en/resources/documents/2020/global-aids-report (accessed 13 September 2021). [ Links ]
2. Joint United Nations Programme on HIV and AIDS (UNAIDS). How AIDS changed everything: MDG 6: 15 years, 15 lessons of hope from the AIDS response. 14 July 2015. https://www.unaids.org/en/resources/documents/2015/MDG6_15years-15lessonsfromtheAIDSresponse (accessed 13 September 2021). [ Links ]
3. Joint United Nations Programme on HIV and AIDS (UNAIDS). UNAIDS data 2020. 6 July 2020. https://www.unaids.org/en/resources/documents/2020/unaids-data (accessed 13 September 2021). [ Links ]
4. Pillay Y. Setting the scene: Some data on the HIV epidemic. Presented at the 9th SA AIDS Conference, Durban, South Africa, 11 -14 June 2019. [ Links ]
5. Nyasulu JCY, Maposa I, Sikhakhane BP, Pandya H. Access to HIV services and viral load suppression among children during the 90-90-90 strategy implementation in South Africa: A time series analysis. South Afr J HIV Med 202132(1):1187. https://doi.org/10.4102/sajhivmed.v22i1.1187 [ Links ]
6. Simon KR, Flick RJ, Kim MH, et al. Family testing: An index case finding strategy to close the gaps in pediatric HIV diagnosis. J Acquir Immune Defic Syndr 2018;78(Suppl 2):S88-S97. https://doi.org/10.1097/QAI.0000000000001731 [ Links ]
7. Schlatter AF, Deathe AR, Vreeman RC. The need for pediatric formulations to treat children with HIV. AIDS Res Treat 2016;2016:1654938. https://doi.org/10.1155/2016/1654938 [ Links ]
8. Ardura-Garcia C, Feldacker C, Tweya H, et al. Early tracing of children lost to follow-up from antiretroviral treatment. J Acquir Immune Defic Syndr 2015;70(5):e160-e167. https://doi.org/10.1097/QAI.0000000000000772 [ Links ]
9. Kim MH, Ahmed S, Buck WC, et al. The Tingathe programme: A pilot intervention using community health workers to create a continuum of care in the prevention of mother to child transmission of HIV (PMTCT) cascade of services in Malawi. J Int AIDS Soc 2012;15(Suppl 2):17389. https://doi.org/10.7448/IAS.15.4.17389 [ Links ]
10. Hien H, Meda N, Diagbouga S, et al. 24-month adherence, tolerance and efficacy of once-a-day antiretroviral therapy with didanosine, lamivudine, and efavirenz inAfrican HIV-1 infected children: ANRS 12103/12167. Afr Health Sci 2013;13(2):287-294. https://doi.org/10.4314/ahs.v13i2.13 [ Links ]














