Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.111 no.9 Pretoria Set. 2021
http://dx.doi.org/10.7196/SAMJ.2021.v111i9.15331
RESEARCH
The reliability of physical examination in diagnosing arterial injury in penetrating trauma to extremities: A first look at different anatomical regions and injury mechanisms
J le RouxI; M BurgerII; G du PreezIII; N FerreiraIV
IMB ChB, DA (SA), MMed (Orth), FC Orth (SA); Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
IIPhD; Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
IIIMB ChB, FC Orth (SA); Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
IVMB ChB, MMed (Orth), FC Orth (SA), PhD Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND. The accuracy of physical examination to exclude arterial injury in penetrating trauma to extremities has been well established. Objectives. To determine whether the accuracy of physical examination to exclude arterial injury is similar to that of a computed tomography arteriogram (CTA) for different anatomical regions and mechanisms of injury, and in patients with concomitant fractures compared with those without.
METHODS. A retrospective review was conducted on all patients who underwent CTA for penetrating injuries to an extremity between 1 June 2016 and 30 June 2017. The presence of arterial injuries was noted, and these were grouped into anatomical areas. Clinical notes were reviewed for the presence of hard signs of arterial injury at initial examination.
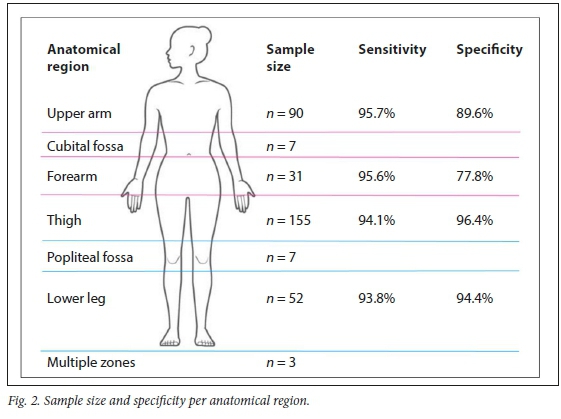
RESULTS. A total of 220 lower limb and 133 upper limb CTAs were included. The mean patient age was 28.9 years (range 11 - 68). The overall sensitivity of physical examination in detecting a CTA-confirmed arterial injury was 95.3% (95% confidence interval (CI) 88.4 - 98.7), with a specificity of 93.9% (95% CI 90.2 - 96.4). Physical examination of the thigh had the highest specificity of 96.4% (95% CI 91.8 - 98.8), followed by the lower leg at 94.4% (95% CI 81.3 - 99.3), the upper arm at 89.6% (95% CI 79.7 - 95.7) and the forearm at 77.8% (95% CI 40.0 - 97.2).
For gunshot wounds the specificity was 96.1% (95% CI 92.4 - 98.3), while for stab wounds it was 86.8% (95% CI 74.7 - 94.5).
CONCLUSIONS. This study agrees with current literature indicating that physical examination has high specificity in detecting arterial injury in the setting of penetrating trauma to an extremity. However, it shows that the specificity is not equal for all anatomical regions or mechanisms of injury.
Penetrating trauma to an extremity (PTE) is a common cause for emergency department presentations and can cause arterial injury, which can lead to loss of life or limb.[1,2] The protocol on how to investigate these patients for arterial injuries has been the topic of much deliberation over the past three decades.[1,3-7] After the Korean War, increased awareness of the hazards of missed arterial injuries after PTE led to decades of liberal use of conventional arteriography (CA) to exclude arterial injuries.[6] This practice only changed in the 1990s, when prospective trials confirmed the high accuracy of physical examination alone in excluding arterial injury in cases of PTE.[1,6-8] Patients without 'hard' signs of arterial injury (pulse deficit, distal ischaemia, bruit, thrill, large or expanding haematoma, and active haemorrhage[7] were no longer subjected to unnecessary arteriograms.
These studies, however, did not attempt to ascertain whether physical examination is equally accurate for upper and lower limbs, or separate anatomical regions, and in the rare event where an arterial injury could not be diagnosed by physical examination, the specific mechanism of trauma in these missed injuries was not always specified.
The initial description of computed tomography angiography (CTA) was in 1992,[9] and subsequent advances in multi-row detectors and gantry speed made angiography of entire limbs possible during the first pass of a contrast medium.[10] Studies soon followed that proved the accuracy of CTA in diagnosing arterial injuries in penetrating trauma to be comparable to that of CA.[11-15] Despite previous evidence and because CT scanners became ubiquitous in trauma departments, and owing to the convenience of a minimally invasive and rapid test, CTAs have again become part of the standard work-up for PTE in some institutions, in patients without any hard or soft signs of arterial injury[16,17] The widespread use of CTAs unnecessarily exposes a patient to a costly examination, as well as potential harmful effects of radiation and intravenous contrast.
Objectives
To re-evaluate the clinical efficacy of physical examination in excluding arterial injuries in PTE, as well as to establish this accuracy for different anatomical regions and mechanisms of injury.
Methods
A retrospective review was conducted on all patients who underwent CTA in the regional trauma centre at Tygerberg Hospital, Cape Town, South Africa. Ethical approval from the Health Research Ethical Council (ref. no. #S16/07/119) and institutional approval from the hospital review board was obtained.
The hospital's electronic picture archiving and communication system (iSite; Phillips, Netherlands) was used to review all upper and lower extremity CTAs done from 1 June 2016 to 30 June 2017. Patients who had CTAs done for penetrating trauma, from all age groups, were included. Exclusion criteria were if the CTA was done for reasons other than penetrating trauma, if the injury fell outside the proximal defined border for the limb, if there was a delay of >48 hours to presentation, if the CTA was inconclusive (mostly owing to movement or scatter artefacts), if clinical notes concerning the penetrating injury were unavailable, previous significant penetrating trauma or arterial injury to the specific limb, and shotgun injuries.
The presence of arterial injuries was recorded, with the specific artery and type of injury noted. The proximal border of the upper extremity was defined as the deltopectoral groove, and for the lower extremity as the inguinal ligament anteriorly, and the horizontal gluteal crease posteriorly. The CTAs and radiographs were also used to record the presence of fractures associated with the penetrating injury.
All clinical notes were reviewed to obtain the mechanism of penetrating injury, anatomical location of penetrating injury and presence of hard signs of arterial injury. The anatomical location of the penetrating injury was classified as upper arm, cubital fossa, forearm, thigh, popliteal fossa or lower leg. If an injury such as a gunshot wound (GSW) traversed more than one anatomical zone it was recorded as multiple zones. Doppler ultrasound was not used as a routine adjunct to measure the ankle brachial index or brachial-brachial index, and was therefore not included.
Data were analysed using Statistica v.13 (TIBCO, USA) and GraphPad Prism v.6 (GraphPad Software Inc., USA). General characteristics such as age and gender are reported as means (standard deviation (SD)) with ranges indicated in parentheses, or counts with frequencies indicated in parentheses. Sensitivities and specificities of 'hard signs' v. the gold standard of CTA were calculated using the abovementioned software packages.
Results
Participant demographics
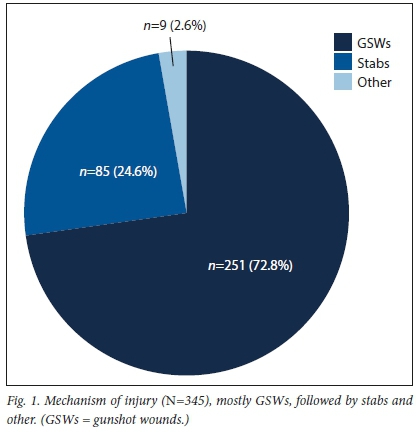
A total of 656 extremity CTAs were done at our institution from 1 June 2016 to 30 June 2017. After exclusions, a total of 345 patients were included in the study, with a male predominance of 318 patients (92.2%) and 27 female patients (7.8%). The mean (SD) age of participants was 29 (8.9) years (range 11 68 "). The most frequent cause of penetrating injury was GSWs, followed by stab wounds, and the remainder were mostly caused by glass fragments (Fig. 1).
Of the 345 injuries, 128 (37.1%) were in the upper limbs: 90 (26.1%) in the upper arm, 7 (2.0%) in the cubital fossa and 31 (9.0%) in the forearm (Fig. 2). There were 217 (62.9%) penetrating injuries to the lower limbs: 155 (44.9%) in the thigh, 7 (2.0%) in the popliteal fossa and 52 (15.1%) in the lower leg; 3 injuries (0.9%) spanned across more than one distinct anatomical zone and were classified as multiple zones. There were 127 patients (36.8%) who sustained concomitant fractures, while 218 (63.2%) did not have any skeletal injuries.
Physical examination v. CTA
A total of 86 patients (24.9%) had arterial injuries as confirmed by CTA, of whom 81 (94.2%) were reported to have abnormalities on clinical examination (hard signs of arterial injury or diminished pulse compared with the contralateral side). Five patients (5.8%) with arterial injuries, as confirmed by CTA, had no record of hard signs of arterial bleeding or diminished pulses.
Compared with the gold standard of CTA, physical examination had a global sensitivity of 95.3% (95% Cl 88.39 98.70 ") and a specificity of 93.85% (95% Cl 90.20 96.44 ") (Table 1). Physical examination of lower limb injuries had on average a higher specificity compared with upper limb injuries. In patients who sustained a concomitant fracture, physical examination had a specificity of 98.0% (95% Cl 93.03 98.97 ") to identify a vascular injury, compared with a specificity of 91.2% (95% Cl 95.67 95.10 ") if no fracture was present.
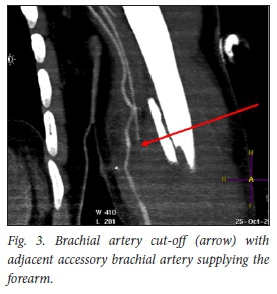
In the current study, a total of 5 patients' arterial injuries were missed by physical examination (Table 2). Of these 5 patients, 3 did not undergo arterial repair (1 patient absconded), 1 patient had an accessory brachial artery that could have accounted for distal pulses still being present (Fig. 3), and 1 patient sustained a GSW to the thigh with resultant superficial femoral artery stenosis and femur fracture (Fig. 4). The admission notes stated that the patient had a palpable dorsalis pedis artery, but this was not compared with the contralateral side and could account for a diminished pulse not being detected. The patient was surgically treated with an interposition vein graft and an intramedullary femoral nail.

Discussion
The objective of the study was to determine whether physical examination in PTE is equally accurate for all anatomical regions and mechanisms of injury, and in patients with and without concomitant fractures.
The first main finding of this study was that different anatomical regions did not share the same specificity of physical examination to exclude arterial injury in penetrating trauma to the extremity, with physical examination having a higher specificity in the lower limbs than in the upper limbs (96.1 v. 88.3%, respectively). When subdividing the limbs into anatomical regions, the specificity in the thigh was higher than in the lower leg (96.5% v. 94.4%, respectively), while the specificity of physical examination to exclude arterial injury in the upper arm was higher than in the forearm (89.4% v. 77.8%). A previous study reported only two missed arterial injuries in their series of 318 patients, both of which were axillary arteries.[7]
An explanation for this finding could be that there are two critical arteries in the forearm, the radial and ulnar arteries, and three critical arteries in the lower leg distal to the trifurcation, the anterior tibial, posterior tibial and peroneal arteries. It is therefore possible to evaluate a normal pulse in an artery different from the injured one, and neglect to examine the pulse in the injured vessel.
The second main finding of the study was that the specificity of physical examination to exclude an arterial injury was higher in the case of GSWs (96.1%) compared with stab wounds (86.5%). An explanation for this finding could be that the energy transfer in GSWs is higher than in stabs, and so GSWs cause more significant arterial injuries that are more easily identified with clinical examination. However, it could also be that more significantly injured patients are more meticulously examined, and a pulse deficit or hard sign of arterial injury is therefore less likely to be missed in a GSW than in a stab wound. In a review by Gurien et al [17]a stab wound was also the mechanism of injury in the only patient who had normal pulses on examination and was discharged, but later became symptomatic and was found to have a pseudoaneurysm of the profunda femoris artery. The findings of the current study therefore differ from those of Erykberg et al. [1] in 1991, who reported 'no difference that is attributable to the mechanism in either the incidence of vascular injuries or in outcome when physical examination is used to examine proximity penetrating trauma to an extremity'.
The third main finding of the present study was that the specificity of physical examination alone to exclude an arterial injury was higher in the group with concomitant fractures than in the group without (98.0% v. 91.1%). The reason for this could again be that patients with fractures are potentially examined more carefully, and that arterial injuries are therefore more likely to be detected; however, this remains to be confirmed.
Based on these findings, we can recommend that a penetrating GSW to an extremity is not in itself an indication to perform CTA to exclude arterial injury. This also holds true for a concomitant long-bone fracture in the presence of PTE. These injuries should not be seen as a 'soft sign of an arterial injury.
We cannot, however, recommend a single strategy appropriate for all patients with PTE. In the study by Erykberg et2 patients had missed arterial injuries.[11]
One patient was admitted to hospital and signs of ischaemia were recognised after 12 hours, and the second patient was discharged, but returned 30 hours later when arterial bleeding reoccurred. If a patient is not capable of returning to hospital, or is not likely to (e.g. high remoteness index, poor socioeconomic status, different cultural beliefs), or will not recognise the onset of hard signs of arterial injury (poor mental capacity, substance abuser, etc.), it may therefore be an indication to do a CTA in a patient with a high suspicion of an arterial injury, but without hard signs of arterial bleeding. Cases such as these should be individualised and managed accordingly.
Study limitations
There are several limitations to this study, the first being its retrospective nature. Patients with PTE were investigated according to the protocol of the emergency unit, but in some instances the comparison of the pulse on the injured side with the contralateral side was not documented. Had this been done, the specificity to exclude an arterial injury could possibly have been higher. The hospital is, however, a level I trauma centre with experienced clinicians who have daily exposure to penetrating trauma. The second limitation of the study is the sample size. Although the overall sample size is large compared with similar studies in the literature, once the patients were subdivided into different anatomical regions, the sizes were smaller, and a statistically relevant sample was not achieved for the cubital or popliteal fossas.
Conclusions
The present study illustrates that physical examination remains highly accurate to exclude arterial injuries in PTE. Meticulous examination and comparison of the pulse on the injured limb with that on the contralateral limb can save unnecessary CTAs and the associated costs and radiation exposure. The specificity of physical examination to exclude an arterial injury is not equal for all anatomical regions, and this should be kept in mind when evaluating patients with PTE, with the upper limb and specifically the forearm having the lowest specificity for clinically diagnosing an arterial injury. Finally, although fractures or GSWs have previously been seen by some as a soft sign of or intermediate risk for an arterial injury in PTE, we report the specificity of physical examination compared with CTA in patients with fractures or GSWs to be higher compared with those without fractures or GSWs. A concomitant fracture, or a GSW as the mechanism of injury, is not in itself an indication for a CTA. A prospective trial is needed to confirm the findings of different specificity for all anatomical regions, mechanisms of injuries and patients with or without fractures.
Declaration. The research for this study was done in partial fulfilment of the requirements for JlR's MMed (Orthopaedics) degree at Stellenbosch University.
Acknowledgements. The authors thank Drs Katherine Nel and Michael Cooke for assistance with data collection.
Author contributions. JlR: conceptualisation, methodology, data collection and verification, validation, review and editing, original draft preparation. GdP: methodology, original draft preparation, review and editing, supervision. MB: methodology, review and editing, formal analysis, supervision. NF: methodology, original draft preparation, review and editing, supervision.
Funding. None.
Conflicts of interest. None.
References
1. Frykberg ER, Dennis JW, Bishop K, Laneve L, Alexander RH. The reliability of physical examination in the evaluation of penetrating extremity trauma for vascular injury: Results at one year. J Trauma 1991;31(4):502-511. https://doi.org/10.1097/00005373-199104000-00009 [ Links ]
2. Franz RW, Shah KJ, Halaharvi D, Franz ET, Hartman JF, Wright ML. A 5-year review of management of lower extremity arterial injuries at an urban level I trauma center. J Vasc Surg 2011;53(6):1604-1610. https://doi.org/10.1016/j.jvs.2011.01.052 [ Links ]
3. Snyder WH, Thal ER, Bridges RA, Gerlock AJ, Perry MO, Fry WJ. The validity of normal arteriography in penetrating trauma. Arch Surg 1978;113(4):424-428. https://doi.org/10.1001/archsurg.1978.01370160082013 [ Links ]
4. Gorman RBO, Feliciano DV, Bitondo CG, Mattox KL, Burch JM, Jordan GL. Emergency centre arteriography in the evaluation of suspected peripheral vascular injuries. Arch Surg 1984;119(5):568-573. https://doi.org/10.1001/archsurg.1984.01390170064013 [ Links ]
5. Menzoian JO, Doyle JE, Logerfo FW, Cantelmo N, Weitzman AF, Sequiera JC. Evaluation and management of vascular injuries of the extremities. Arch Surg 1983;118(1):93-95. https://doi.org/10.1001/archsurg.1983.01390010069016 [ Links ]
6. Weaver FA, Yellin AE, Bauer M, et al. Is arterial proximity a valid indication for arteriography in penetrating extremity trauma? A prospective analysis. Arch Surg 1990;125(10):1256-1260. http://www.ncbi.nlm.nih.gov/pubmed/2222167 [ Links ]
7. Dennis JW, Frykberg ER, Crump JM, Vines FS, Alexander RH. New perspectives on the management of penetrating trauma in proximity to major limb arteries. J Vasc Surg 1990;11(1):84-93. https://doi.org/10.1016/0741-5214(90)90332-5 [ Links ]
8. Schwartz MR, Weaver FA, Bauer M, Siegel A, Yellin AE. Refining the indications for arteriography in penetrating extremity trauma: A prospective analysis. J Vasc Surg 1993;17(1):116-124. https://doi.org/10.1067/mva.1993.42588 [ Links ]
9. Schwartz B, Mukherji K, Jones M, et al. Common carotid artery bifurcation: Evaluation with spiral CT. Radiology 1992;185(2):513-519. https://doi.org/10.1148/radiology.185.2.1410365 [ Links ]
10. Rubin GD, Leipsic J, Schoepf UJ, Fleischmann D, Nap el S. CT angiography after 20 years: A transformation in cardiovascular disease characterization continues to advance. Radiology 2014;271(3):633-652. https://doi.org/10.1148/radiol.14132232 [ Links ]
11. Inaba K, Potzman J, Munera F, et al. Multi-slice CT angiography for arterial evaluation in the injured lower extremity. J Trauma 2006;60(3):502-507. https://doi.org/10.1097/01.ta.0000204150.78156.a9 [ Links ]
12. Jens S, Kerstens MK, Legemate DA, Reekers JA, Bipat S, Koelemay MJW. Diagnostic performance of computed tomography angiography in peripheral arterial injury due to trauma: A systematic review and meta-analysis. Eur J Vasc Endovasc Surg 2013;46(3):329-337. https://doi.org/10.1016/j.ejvs.2013.04.034 [ Links ]
13. Colip CG, Gorantla V, LeBedis CA, Soto JA, Anderson SW. Extremity CTA for penetrating trauma: 10-year experience using a 64-detector row CT scanner. Emerg Radiol 2017;24(3):223-232. https://doi.org/10.1007/s10140-016-1469-z [ Links ]
14. Adibi A, Krishnam MS, Dissanayake S, et al Computed tomography angiography of lower extremities in the emergency room for evaluation of patients with gunshot wounds. Eur Radiol 2014;24(7):1586-1593. https://doi.org/10.1007/s00330-014-3174-1 [ Links ]
15. Fox N, Rajani RR, Bokhari F, et al. Evaluation and management of penetrating lower extremity arterial trauma. J "Trauma Acute Care Surg 2012;73(5 Suppl 4):315-320. https://doi.org/10.1097/ta.0b013e31827018e4 [ Links ]
16. Jordaan P, Roche S, Maqungo S. Computerised tomographic angiography (CTA) in extremity trauma -a level one hospital experience. S Af J Surg 2016;54(4):11-16. [ Links ]
17. Gurien LA, Kerwin AJ, Yorkgitis BK, et al. Reassessing the utility of CT angiograms in penetrating injuries to the extremities. Surgery 2018;163(2):419-422. https://doi.org/10.1016/j.surg.2017.09.019 [ Links ]
 Correspondence:
Correspondence:
J le Roux
johan.abroad@gmail.com
Accepted 25 March 2021














