Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.111 n.6 Pretoria Jun. 2021
http://dx.doi.org/10.7196/SAMJ.2021.v111i6.15580
RESEARCH
The initial impact of the COVID-19 pandemic on the diagnosis of new cancers at a large pathology laboratory in the public health sector, Western Cape Province, South Africa
A C van WykI; L J de JagerII; R RazackIII; S S van WykIV; W KleinhansV; H M SimondsVI; P T SchubertVII
IMB ChB, MMed (Anat Path); National Health Laboratory Service, Division of Anatomical Pathology, Tygerberg Hospital and Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIMB ChB, MMed (Anat Path), FC Path (SA) Anat; National Health Laboratory Service, Division of Anatomical Pathology, Tygerberg Hospital and Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIMB ChB, MMed (Anat Path), FC Path (SA) Anat, MSc (Med Sc) Cytopathology; National Health Laboratory Service, Division of Anatomical Pathology, Tygerberg Hospital and Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IVMB ChB, MSc (Clin Epi); Centre for Evidence-Based Health Care, Division of Epidemiology and Biostatistics, Department of Global Health, Stellenbosch University, Cape Town, South Africa
VBTech; National Health Laboratory Service, Division of Haematological Pathology, Tygerberg Hospital and Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIMB ChB, MRCP, FRCR, PG Dip HE, PhD; Division of Clinical and Radiation Oncology, Department of Medical Imaging and Clinical Oncology, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
VIIMB ChB, MMed (Anat Path), FC Path (SA) (Anat), MSc (Med Sc) Cytopathology, MPhil (Paed Path) National Health Laboratory Service, Division of Anatomical Pathology, Tygerberg Hospital and Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND. The COVID-19 pandemic has disrupted cancer diagnostic services. A decline in the number of new cancers being diagnosed over a relatively short term implies a delay in diagnosis and subsequent treatment. This delay is expected to have a negative effect on cancer-related morbidity and mortality. The impact of the pandemic on the number of new cancer diagnoses in our setting is unknown.
OBJECTIVES. To assess the impact of COVID-19 on the number of new cancers diagnosed at our institution in the first 3 months following the implementation of lockdown restrictions, by focusing on common non-cutaneous cancers.
METHODS. A retrospective laboratory-based audit was performed at a large anatomical pathology laboratory in Western Cape Province, South Africa. The numbers of new diagnoses for six common cancers (breast, prostate, cervix, large bowel, oesophagus and stomach) from 1 April 2020 to 30 June 2020 were compared with the corresponding period in 2019.
RESULTS. Histopathological diagnoses for the six cancers combined decreased by 192 (-36.2%), from 531 new cases in the 2019 study period to 339 in the corresponding period in 2020. Substantial declines were seen for prostate (-58.2%), oesophageal (-44.1%), breast (-32.9%), gastric (-32.6%) and colorectal cancer (-29.2%). The smallest decline was seen in cervical cancer (-7%). New breast cancers diagnosed by cytopathology declined by 61.1%.
CONCLUSIONS. The first wave of the COVID-19 pandemic and the associated response resulted in a substantial decline in the number of new cancer diagnoses, implying a delay in diagnosis. Cancer-related morbidity and mortality is expected to rise as a result, with the greatest increase in mortality expected from breast and colorectal cancer.
The COVID-19 pandemic and its associated response have disrupted essential health services across the globe.[1] In South Africa (SA), as in many other countries affected by the pandemic, healthcare resources have been shifted away from non-COVID-19 patients to deal with the surge in COVID-19 patientsJ2] Concern has been raised over the impact on morbidity and mortality from diseases that have been sidelined in favour of COVID-19.[3]
Cancer diagnosis is one of the essential health services that have been negatively affected. Several studies from around the world have reported a decline in the number of new cancers diagnosed since the start of the pandemic[4-14] Since the incidence of cancer is expected to remain relatively stable over a period of months, this decline can be attributed to a delay in cancer diagnosis due to the pandemic. A delay in diagnosis is likely to lead to patients presenting at a more advanced stage and poorer clinical outcomes.
The anatomical pathology laboratory at our institution is one of only two anatomical pathology laboratories that serve the adult public healthcare sector in Western Cape Province, SA. We observed a substantial decrease in our total pathology caseload during the months following the implementation of national lockdown restrictions on 26 March 2020, but the exact effect on the number of new cancer diagnoses is unknown.
Objectives
To assess the impact of the COVID-19 pandemic and its associated response on the number of new cancers diagnosed at our institution during the months following the implementation of lockdown restrictions.
Methods
We conducted a retrospective laboratory-based audit of common, newly diagnosed, non-cutaneous cancers in adults (>18 years of age) in specimens registered during the 3-month period of the second quarter of the year, from 1 April 2020 to 30 June 2020 (2020 Q2), and compared this with the corresponding period in 2019 (2019 Q2).
The non-cutaneous cancers in SA with the highest projected incidence were selected for the audit: cancer of the breast, prostate, uterine cervix, lung and colorectum.[15] In addition, cancer of the oesophagus was included because it is currently ranked fifth in terms of mortality. Stomach cancer was included because the Western Cape is a known hotspot for this cancer in SA.
Cancers of these anatomical sites diagnosed by histopathology were identified by searching for Systematized Nomenclature of Medicine codes on the laboratory information system. These codes had been assigned at the time of diagnosis by the pathologist responsible for the case. The electronic pathology reports were accessed and reviewed to confirm that the code corresponded to the diagnosis on the report. The following cases were excluded: (!) referred cases from outside the usual drainage area of the laboratory; (!!) in situ carcinoma where no invasion could be demonstrated; (!!!) cases where the diagnosis of cancer was uncertain; (!v) recurrent cancer that had already been previously diagnosed; and (v) duplicate diagnoses from the same anatomical site (only first specimen included).
For breast cancer, in addition to the above cancers diagnosed by histopathology, cancers diagnosed on fine-needle aspiration biopsy by cytopathology were identified by searching for the malignant breast cytology category code. Similar exclusion criteria were applied, but breast cancers diagnosed by cytopathology were reported separately from breast cancers diagnosed by histopathology (some patients may have been diagnosed by both modalities).
We determined the total number of histopathology specimens with unique episode numbers registered on the laboratory information system during 2020 Q2 and the corresponding periods during the preceding 3 years (2017 - 2019) to assess the overall histopathology caseload trend over a 4-year period. The number of new cancers for the selected anatomical sites were then determined for 2020 Q2 and 2019 Q2. We compared age at diagnosis, sex (for oesophageal, gastric and colorectal cancer) and the level of healthcare facility (central, regional and district level and lower) where the diagnostic procedure was performed between these two time periods.
Analysis was completed using Stata Statistical Software, release 10 (StataCorp, USA). Frequency distributions, means and 95% confidence intervals (CIs) were calculated where applicable. The time period during which diagnoses were made was assessed for bivariate association with age at diagnosis, sex (where applicable) and the level of the health facility where the diagnostic procedure was performed. The t-test for means and χ2 test for proportions were used at a significance level of 0.05 (2-sided).
The study received ethical approval from the Stellenbosch University Health Research Ethics Committee on 4 November 2020 (ref. no. N20/10/065_COVID-19).
Results
The laboratory received histopathology and cytopathology specimens from public healthcare facilities distributed over a large geographical area that included parts of the City of Cape Town metropolitan area and the Cape Winelands, Central Karoo, Garden Route, Overberg and West Coast districts. This drainage area is inhabited by an estimated 4.5 million people,[16] of whom fewer than 25% are covered by medical insurance[17] Tissue specimens with a diagnosis of cancer were received from one central hospital, three regional hospitals, 24 district hospitals and 8 different community health centres/clinics. The laboratory drainage area remained the same for 2019 Q2 and 2020 Q2.
The number of working days for both periods was the same (60 days). The 2020 Q2 period extended over three different COVID-19 alert levels: level 5 from 1 to 30 April, level 4 from 1 to 31 May and level 3 from 1 to 30 June.
The overall histopathology caseload for the second quarter of the year remained relatively stable for the 3 preceding years, with 7 503, 8 118 and 8 157 cases in 2017, 2018 and 2019, respectively, but decreased dramatically by 3 825 (-46.9%) to 4 332 cases in 2020.
New histopathological diagnoses for six selected cancers combined (breast, prostate, uterine cervix, colorectum, oesophagus and stomach) decreased by 192 (-36.2%) from 531 in 2019 Q2 to 339 in 2020 Q2.
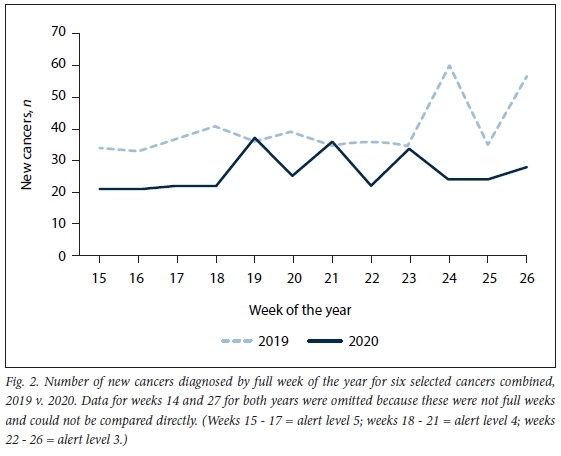
Lung cancer had to be excluded from the analysis owing to inability to distinguish accurately between primary and secondary tumours based on the limited clinical data available in the pathology reports. A summary of the results is presented in Table 1. The largest decline was seen in prostate cancer (-58.2%) and the smallest in cervical cancer (-7%) (Fig. 1). Breast cancers diagnosed by cytopathology declined by 61.1%. Gastrointestinal cancers (cancer of the oesophagus, stomach and colorectum combined) declined by 35.5%. The number of new cancers diagnosed per full week is graphically represented in Fig. 2. The number of new histopathology diagnoses for the six cancers combined, as a percentage of the total histopathology caseload, increased from 6.5% in 2019 Q2 to 7.8% in 2020 Q2.

The mean age at diagnosis for the six cancers in 2020 was 2 years younger than in 2019 (p=0.018). The age difference was most pronounced for colorectal cancer, with a mean age of 64 years in 2019 Q2 and 58 years in 2020 Q2 (p=0.012). The age at diagnosis for the other specific cancers did not show any statistically significant differences between the study periods.
There was no statistically significant difference between the study periods in sex or in the level of healthcare facility where the diagnostic procedures were performed.
Forty-four of 66 patients with cervical cancer (66.7%) diagnosed in 2020 Q2 had an abnormal cervical smear cytology result during the preceding year.
Sub-analysis of prostate cancers showed a decrease of 63.6% in high-risk cancers (Grade Groups 4 and 5), in line with the decrease of 53.7% in low- and intermediate-risk cancers (Grade Groups 1 - 3).
Colorectal cancer tended to be diagnosed more frequently on resection specimens than on biopsy specimens in 2020 Q2 compared with 2019 Q2, but this result was not statistically significant (odds ratio 1.9; 95% Cl 0.92 - 3.96; p=0.079). The pathological stage of colorectal cancers first diagnosed on resection specimens did not show a statistically significant difference between these periods p=0.101).
Discussion
We demonstrated a substantial decline in newly diagnosed cancers (-36.2%) for six common cancers combined in 2020 Q2 compared with 2019 Q2. Our results echo the findings of several studies (using a variety of data sources) from around the world (Table 2).
There are many possible reasons for this decline. In a pulse survey conducted by the World Health Organization, the reasons provided for the interruption of essential health services were a mix of demand and supply factors.!11 On the demand side, the causes most often mentioned were patients not presenting to outpatient care, public transport restrictions hindering access, and financial difficulties preventing attendance. Fear of contracting COVID-19 and mistrust were mentioned as additional reasons. On the supply side, the most commonly mentioned factor was the cancellation of elective services. Other factors included staff redeployment to provide COVID-19 relief, insufficient personal protective equipment available for healthcare providers, unavailability of services due to closure of services or health facilities, and interruptions in the supply of medical equipment and health products.
In our setting, the suspension or de-escalation of routine outpatient health services appeared to play a major role in the decline and may explain some of the differences in the decline between specific cancers. The large decline in new breast cancers diagnosed on cytopathology can in part be ascribed to the temporary closure of a dedicated fine-needle aspiration clinic. Similarly, the decline in prostate cancer and gastrointestinal cancers can largely be attributed to the substantial de-escalation of routine prostate biopsy and endoscopic services, respectively. The small decline in the number of newly diagnosed cervical cancers can be explained by the uninterrupted, albeit scaled-down, service of the colposcopy clinic at our institution throughout the study period. However, outreach colposcopy clinics were cancelled. Cervical cancer also had the benefit of being part of a formal screening programme, which was not the case with the other cancers in this study. Approximately two-thirds of patients diagnosed with cervical cancer in 2020 Q2 had an abnormal cervical smear result in the preceding year, and were therefore likely to already have had a referral letter to a colposcopy clinic or a date for an appointment at the start of the pandemic. Disruption of the cervical screening programme during 2020 Q2 is likely to have a negative effect on cervical cancer diagnosis after the study period.
The reason for the statistically significant lower age at cancer diagnosis in 2020 Q2 compared with 2019 Q2 for the six cancers combined and for colorectal cancer individually is not clear. A possible explanation is that older patients tended to avoid healthcare facilities more than younger patients during the initial phase of the pandemic.
Predicting the impact of diagnostic delay on patient outcome is complex and dependent on cancer type and stage. In general, a delay in diagnosis is likely to result in a delay in treatment, which carries the risk of a tumour progressing from being curable to incurable. Apart from resulting in avoidable death, an increase in tumour stage may also lead to more extensive and complex treatment, potentially increasing morbidity and healthcare costs.
Unpublished data from our radiotherapy unit for the third quarter of 2020 show a remarkable correlation between the decline in new cancer diagnoses in the second quarter and the reduction in radiotherapy for three cancers for which patients were likely to receive radiotherapy as part of their treatment plan: prostate (-47.9%), breast (-23.5%) and cervical cancer (-3%) (Prof. Hannah Simonds, personal communication). The correlation between diagnostic decline and reduction in administered radiotherapy treatment for these cancers is observed despite the influence of other factors, apart from diagnostic delays, that may have influenced the administration of radiotherapy.
Several studies have attempted to quantify the effect of diagnostic and treatment delays on cancer outcomeJ18-23] While it has been shown that a delay in surgical treatment for prostate cancer of up to 1 year was not associated with adverse oncological outcomes[22] there is concern over the effect of delay on more aggressive cancer types. A pre-pandemic cancer registry study from Taiwan on 39 000 colorectal cancers found that a longer interval (>30 days) from diagnosis to the start of treatment was associated with a significantly higher risk of death.[23] In the USA, a model considering the effect of COVID-19 on cancer screening and treatment for breast and colorectal cancer predicted almost 10 000 excess deaths associated with these cancers over the next 10 years. A population-based modelling study in England estimated >3 000 avoidable deaths and an additional ~60 000 total years of life lost from breast, colorectal, lung and oesophageal cancer due to diagnostic delays resulting from disruption caused by the COVID-19 pandemic.[20]
In SA, for cancers that showed a substantial decline from pre-pandemic levels, the effect of diagnostic delay on mortality will probably be most significant for breast and colorectal cancer. Unfortunately, even before the pandemic, most oesophageal and gastric cancers were diagnosed at an advanced stage,[24,25] and further diagnostic delays will probably not have a significant impact on mortality. Nonetheless, it will take longer for these patients to access palliative care, which will result in unnecessary morbidity.
The negative impact of COVID-19 on cancer care goes beyond cancer diagnosis and includes the disruption of cancer screening, treatment and research.[21] Apart from these immediate and direct effects on cancer care, economic recessions per se have been shown to have a negative impact on cancer care in pre-pandemic studies,[26,27] presumably as a consequence of decreased utilisation of preventive healthcare.
To minimise the impact of future lockdowns on cancer diagnosis, it is essential that outpatient clinics, endoscopy services, mammography services and cancer screening programmes continue to function uninterrupted at full capacity as far as possible. Increased resources and staff will be required, in particular to improve capacity for endoscopy and mammography services. Public cancer awareness campaigns should be considered to provide information about the importance of early detection and diagnosis of cancer. Ultimately, the urgent and wide-scale roll-out of an effective SARS-CoV-2 vaccine is required to prevent further waves and lockdowns, protect the healthcare system, and reassure patients that it is safe to visit healthcare facilities.
One of the limitations of this study is that it was conducted at a single institution. From our interaction with pathologists at other laboratories, we suspect that our experience parallels that of most anatomical pathology practices in SA. Another limitation is that we could not provide accurate data for lung cancer, as we did not consistently have adequate clinical information on the pathology report to classify tumours as primary lung cancers or metastases from other organs.
Further studies are necessary to assess changes in the incidence of cancer over a longer period of time, including investigating a possible rebound effect caused by 'catching up' on cancers that had a delayed presentation, the effects of further COVID-19 surges, and the effects of disruption of cervical cancer screening programmes on the subsequent diagnosis of cervical cancer beyond the study period. The true impact on stage migration and cancer-specific mortality will only be revealed in the next 5 - 10 years.
Conclusions
The first wave of the COVID-19 pandemic and the associated response resulted in a substantial decline in the number of new cancer diagnoses at our institution, implying a delay in cancer diagnosis and treatment. Cancer-related morbidity and mortality in the next 5 -10 years is expected to rise as a result of this, with the greatest increase in mortality expected from breast and colorectal cancer. The effect of COVID-19 restrictions on the morbidity and mortality of non-COVID-19 diseases such as cancer should be carefully considered to minimise the total burden of disease over the long term.
Declaration. None.
Acknowledgements. None.
Author contributions. ACvW and PTS conceived the study idea; WK, ACvW and PTS collected the data; LJdJ and RR validated the data; SSvW analysed the data; and ACvW drafted the first version of the manuscript with contributions from LJdJ, RR and HMS. All authors revised and approved the final manuscript.
Funding. None.
Conflicts of interest None.
References
1. World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: Interim report, 27 August 2020. Geneva: WHO, 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 (accessed 8 December 2020). [ Links ]
2. Taylor A, Taylor B, Parkes J, Fagan J. How should health resource allocation be applied during the COVID-19 pandemic in South Africa? S Afr Med J 2020;110(7):561. https://doi.org/10.7196/SAMJ.2020.v110i7.14916 [ Links ]
3. Hofman K, Madhi S. The unanticipated costs of COVID-19 to South Africa's quadruple disease burden. S Afr Med J 2020;110(8):698-699. https://doi.org/10.7196/SAMJ.2020.v110i8.15125 [ Links ]
4. Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 2020;21(6):750-751. https://doi.org/10.1016/s1470-2045(20)30265-5 [ Links ]
5. De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 'lockdown, due to COVID-19 pandemic, compared with the 2018 - 2019: An audit study from cellular pathology. J Clin Pathol 2020;74:187-189. https://doi.org/10.1136/jclinpath-2020-206833 [ Links ]
6. Ferrara G, de Vincentiis L, Ambrosini-Spaltro A, et al. Cancer diagnostic delay in Northern and Central Italy during the 2020 lockdown due to the coronavirus disease 2019 pandemic. Am J Clin Pathol 2021;155(1):64-68. https://doi.org/10.1093/ajcp/aqaa177 [ Links ]
7. London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Informatics 2020;4:657-665. https://doi.org/10.1200/CCI.20.00068 [ Links ]
8. Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: A National Endoscopy Database Analysis. Gut 2021;70:537-543. https://doi.org/10.1136/gutjnl-2020-322179 [ Links ]
9. Zadnik V, Mihor A, Tomsic S, et al Impact of COVID-19 on cancer diagnosis and management in Slovenia - preliminary results. Radiol Oncol 2020;54(3):329-334. https://doi.org/10.2478/raon-2020-0048 [ Links ]
10. Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open 2020;3(8):e2017267. https://doi.org/10.1001/jamanetworkopen.2020.17267 [ Links ]
11. Tsibulak I, Reiser E, Bogner G, et al Decrease in gynecological cancer diagnoses during the COVID-19 pandemic: An Austrian perspective. Int J Gynecol Cancer 2020;30(11):1667-1671. https://doi.org/10.1136/ijgc-2020-001975 [ Links ]
12. Suárez J, Mata E, Guerra A, et al Impact of the COVID-19 pandemic during Spain's state of emergency on the diagnosis of colorectal cancer. J Surg Oncol 2021;123(1):32-36. https://doi.org/10.1002/jso.26263 [ Links ]
13. Maluchnik M, Podwójcic K, Wiçckowska B. Decreasing access to cancer diagnosis and treatment during the COVID-19 pandemic in Poland. Acta Oncol 2020;60(1):28-31. https://doi.org/10.1080/0284186x.2020.1837392 [ Links ]
14. Marques NP, Silveira DMM, Marques NCT, Martelli DRB, Oliveira EA, Martelli-Júnior H Cancer diagnosis in Brazil in the COVID-19. Semin Oncol 2021 (epub 7 January 2021). https://doi.org/10.1053/j.seminoncol.2020.12.002 [ Links ]
15. World Health Organization International Agency for Research on Cancer (IARC). GLOBOCAN 2020: South Africa. Geneva: WHO, 2020. https://gco.iarc.fr/today/data/factsheets/populations/710-south-africa-fact-sheets.pdf (accessed 6 March 2021). [ Links ]
16. Western Cape Department of Health: Chief Director: Strategy and Health Support. Population Data. Circular H 102/2020. Cape Town: Western Cape Government, 2020. https://www.westerncape.gov.za/assets/departments/health/h_102_2020_covid-19_population_data.pdf (accessed 6 March 2021). [ Links ]
17. Statistics South Africa. General Household Survey, 2019. Pretoria: Stats SA, 2020. http://www.statssa.gov.za/publications/P0318/P03182019.pdf (accessed 6 March 2021). [ Links ]
18. Sud A, Jones ME, Broggio J, et al Collateral damage: The impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol 2020;31(8):1065-1074. https://doi.org/10.1016/j.annonc.2020.05.009 [ Links ]
19. Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: A modelling study. Lancet Oncol 2020;21(8):1035-1044. https://doi.org/10.1016/S1470-2045(20)30392-2 [ Links ]
20. Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: A national, population-based, modelling study. Lancet Oncol 2020;21(8):1023-1034. https://doi.org/10.1016/S1470-2045(20)30388-0 [ Links ]
21. Sharpless NE. COVID-19 and cancer. Science 2020;368(6497):1290. https://doi.org/10.1126/science.abd3377 [ Links ]
22. Ginsburg KB, Curtis GL, Timar RE, George AK, Cher ML. Delayed radical prostatectomy is not associated with adverse oncologic outcomes: Implications for men experiencing surgical delay due to the COVID-19 pandemic. J Urol 2020;204(4):720-725. https://doi.org/10.1097/ju.0000000000001089 [ Links ]
23. Lee YH, Kung PT, Wang YH, Kuo WY, Kao SL, Tsai WC. Effect of length of time from diagnosis to treatment on colorectal cancer survival: A population-based study. PLoS ONE 2019;14(1):e0210465. https://doi.org/10.1371/journal.pone.0210465 [ Links ]
24. Nel D, Omar M, Chinnery G, Jonas E. Disparity in oesophageal cancer management in South Africa: A comparison between two tertiary centres with special focus on the palliation of dysphagia. S Afr J Surg 2019;57(2):10-15. https://doi.org/10.17159/2078-5151/2019/v57n2a2842 [ Links ]
25. Benamro F, Sartorius B, Clarke DL, Anderson F, Loots E, Olinger L. The spectrum of gastric cancer as seen in a large quaternary hospital in KwaZulu-Natal, South Africa. S Afr Med J 2017;107(2):130-133. https://doi.org/10.7196/SAMJ.2017.v107i2.11383 [ Links ]
26. Gomez SL, Canchola AJ, Nelson DO, et al. Recent declines in cancer incidence: Related to the Great Recession? Cancer Causes Control 2017;28(2):145-154. https://doi.org/10.1007/s10552-016-0846-y [ Links ]
27. Maruthappu M, Watkins J, Noor AM, et al. Economic downturns, universal health coverage, and cancer mortality in high-income and middle-income countries, 1990 - 2010: A longitudinal analysis. Lancet 2016;388(10045):684-695. https://doi.org/10.1016/s0140-6736(16)00577-8 [ Links ]
 Correspondence:
Correspondence:
A C van Wyk
abraham.vanwyk@nhls.ac.za
Accepted 18 March 2021














