Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.110 n.8 Pretoria Aug. 2020
http://dx.doi.org/10.7196/SAMJ.2020.v110i8.14512
RESEARCH
Compliance with hygiene practices among healthcare workers in the intensive care unit
A E LaherI, II; L-R van RooyenIII; L GerberIV; G A RichardsV
IMB BCh, MMed, FCEM, Cert Crit Care, EDIC, Dip PEC, DCH, Dip Allerg, Dip HIV Man; Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, MMed, FCEM, Cert Crit Care, EDIC, Dip PEC, DCH, Dip Allerg, Dip HIV Man; Department of Critical Care, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIBTech EMC;Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVBTech EMC; Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VMB BCh, PhD, FCP, FRCP, FCCP; Department of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Intensive care unit (ICU)-related healthcare-associated infections (HCAIs) are two to three times higher in lower-income countries than in higher-income ones. Hand cleansing and other hygiene measures have been documented as one of the most effective measures in combating the transmission of HCAIs. There is a paucity of data pertaining to hygiene practices in the ICU in developing countries.
OBJECTIVES. To determine compliance with hygiene practices among healthcare workers in a tertiary hospital ICU.
METHODS. Hygiene practices of healthcare workers in a tertiary academic hospital ICU in Johannesburg, South Africa, were discreetly observed over an 8-week period. Compliance with hand cleansing and other hygiene practices was documented and analysed. Retrospective consent was obtained, and subject confidentiality was maintained.
RESULTS. A total of 745 hygiene opportunities were observed. Of the 156 opportunities where handwashing with soap and water was indicated (20.9%), compliance was noted in 89 cases (57.1%), while an alcohol-based hand rub was inappropriately used in 34 cases (21.8%) and no hand hygiene was performed in the remaining 33 cases (21.1%). Of the 589 opportunities where an alcohol-based hand-rub was indicated, it was used in 312 cases (53.0%). Compliance with the donning of disposable surgical gloves, disposable plastic aprons and being 'bare below the elbows' was noted in 114 (90.6%), 108 (71.1%) and 355 (47.7%) opportunities, respectively, where these were indicated.
CONCLUSIONS. Overall compliance with hygiene measures among healthcare workers in the ICU was suboptimal in this study, but in keeping with general international trends. Regular retraining of staff, frequent reminders, peer oversight and regular audits may improve compliance.
Patients in intensive care units (ICUs) are at higher risk of acquiring healthcare-associated infections (HCAIs) than patients in the general ward. HCAIs have been associated with an increase in morbidity, mortality, length of ICU stay and costs[1] Rates of HCAIs in the ICU may be as high as 37%[2] According to the World Health Organization (WHO), ICU-related HCAIs are two to three times higher in lower-income countries than in higher-income ones.[3]
The frequent movement of healthcare workers between patients in the ICU is a likely reason for the increased rates of cross-infection among critically ill patientsJ4! Hand cleansing and other hygiene measures have been documented as one of the most effective measures in combating the transmission of HCAIs[5] However, despite implementation of multiple interventions over the years, compliance with hygiene practices among healthcare workers remains suboptimaL.[6,7]
Standard hygiene practices have been well described in various international guidelines[8--10]! In recent years, the use of an alcohol-based hand rub has superseded the use of soap and water in most instances where hand hygiene is required.[11] Other measures, including the appropriate use of personal protective equipment (PPE) such as disposable surgical gloves and plastic aprons and keeping the hands, wrists and forearms free ('bare below the elbows') during contact with patients or their surroundings, have also been proven to limit the spread of micro-organisms in the healthcare setting.[9,10]
Objectives
Compliance with hygiene practices has historically been poor in both high- and low-income countries.[12] Additionally, there is a paucity of data pertaining to hygiene practices in the ICU in resourceconstrained settings. The objective of this study was therefore to determine compliance with hygiene practices among healthcare workers in a South African (SA) ICU setting.
Methods
This cross-sectional, observational study was conducted in the multidisciplinary ICU of a tertiary-level academic hospital in Johannesburg, SA. The ICU has 19 beds and 16 handwashing basins, with each basin being equipped with liquid soap and a paper towel dispenser. In addition, there are 12 fixed as well as 4 - 6 non-fixed alcohol rub dispensers randomly placed in the department. Permission to conduct the study was obtained from the head of the ICU and the chief executive officer of the hospital. Ethics approval was granted by the University of the Witwatersrand Human Research Ethics Committee (ref. no. M170458).
Data were collected by two study investigators who discreetly observed the hygiene practices of all clinical staff, including doctors, nurses and other healthcare professionals who were either part of the permanent ICU staff establishment or were attending the ICU for patient consultation. The study was conducted between 13 May and 7 July 2019. Data were collected daily (on weekdays as well as over weekends) for ~4 hours per day at random times between 08h00 and 20h00. The researchers observed 5 - 10 hygiene opportunities per subject on different days.
During a single patient contact-related encounter, data were collected on whether subjects: (i) adhered to the correct method of hand cleansing (soap and water v. alcohol-based hand rub); (ii) adhered to the correct steps of hand cleansing for the indicated method; (Hi) adhered to the donning of disposable surgical gloves when indicated; (z'v) adhered to the donning of a disposable plastic apron when indicated; and (v) adhered to being bare below the elbows when indicated.
For the purpose of the study, the WHO's '5 moments of hand hygiene' (before touching a patient, before performing an aseptic procedure, after patient body fluid exposure, after touching a patient and after touching a patient's surroundings) were regarded as hygiene opportunities and were assessed for compliance by the study investigators. Subjects were assessed with regard to whether they had correctly adhered to the nine steps of handwashing with soap and running water if their hands were visibly dirty, if their hands were visibly soiled with blood or other body fluids, after using the toilet, or after exposure to patients who were potentially infected or known to be infected with spore-forming pathogens such as Clostridium difficile. For all other patient contact-related encounters (moving from a contaminated to another site during care of the same patient, handling an invasive device for patient care, and after removing sterile or non-sterile gloves), subjects were assessed with regard to whether they had correctly adhered to the six steps of hand cleansing with an alcohol-based hand rub. Subjects were assessed for adherence with the following steps of handwashing when soap and water was indicated: (i) rubbing of hands palm to palm; (ii) rubbing of each palm over the dorsum of the other hand; (,Hi) interlacing of the fingers; (iv) rubbing the back of the fingers to the opposing palm; (v) rotational rubbing of the thumbs; (v) rotational rubbing of fingertips on the palms; (vii) rinsing of the hands under running water; (viii) drying the hands with disposable paper towel; and (ix) turning off the water without contaminating the hands. When an alcohol-based hand rub was indicated, adherence with only the first six steps were assessed. In addition, data were collected on whether study subjects had donned disposable surgical gloves when in contact with blood, mucous membranes, non-intact skin or other potentially infectious material, as well as whether they donned a disposable plastic apron and were bare below the elbows during any episode of direct patient care. [813,14] Data on all of the above items were collected on a specifically designed data collection sheet in a tick-box format.
To maintain subject confidentiality, each potential subject was assigned a code with no linkable identifying data. To eliminate study bias, the investigators did not identify themselves as researchers to potential study subjects or disclose the design, aim and objectives of the study until the period of data collection was completed. Consent was therefore obtained retrospectively upon completion of data collection. All subjects consented to their data being included in the study.
Data were captured into a 2010 Excel spreadsheet (Microsoft, USA) and reported as frequencies and percentages. Fisher's exact and Pearson's χ2 tests were used to assess for differences in hygiene compliance between the various categories of staff. Post-hoc analysis was performed where there were significant differences. Study reporting conformed to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.[15]
Results
A total of 745 hygiene opportunities were observed. Handwashing with soap and water was indicated in 156 (20.9%) of these opportunities, while hand cleansing with an alcohol-based hand rub was indicated in the remaining 589 (79.1%). Of the 156 opportunities where the use of soap and water was indicated, this was only used on 89 occasions (57.1%), while an alcohol-based hand rub was inappropriately used on 34 occasions (21.8%) and no hand hygiene was observed on 33 occasions (21.1%). In contrast, an alcohol-based hand rub was used in 312 (53.0%) of the 589 opportunities where it was indicated. Donning of disposable surgical gloves, donning of disposable plastic aprons and adherence with 'bare below the elbows' were observed in 144 (90.6%), 108 (71.1%) and 355 (47.7%) opportunities respectively, where these were indicated. Overall compliance with the above hygiene practices is described in Fig. 1.
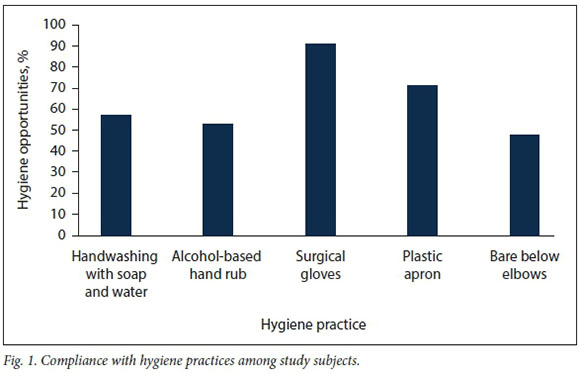
Table 1 describes compliance with each of the steps of hand hygiene in the 435 opportunities where it was attempted. All 9 steps were assessed for handwashing with soap and water, while only the first 6 steps were assessed when an alcohol-based hand rub was used. For handwashing with soap and water, overall compliance was >90% for each of the steps except for turning off the water without contamination of the hands (n=13; 14.6%). All 9 steps were correctly performed in only 12 observations (13.5%), while 8 of the 9 steps were performed in 64 observations (71.9%). When an alcohol-based hand rub was used, overall compliance was <90% in 4 of the 6 steps. All 6 steps were correctly performed in 205 observations (59.2%), while at least 5 steps were completed in only 66 observations (19.1%).
Table 2 describes and compares the percentage compliance with hygiene practices among the various categories of doctors, nurses and other staff. There were statistically significant differences between groups for: (z) step 3 (interlacing of the fingers) of the hand cleansing procedure (p=0.002); (ii) donning of disposable surgical gloves (p=0.004); (z'z'z) the donning of a disposable plastic apron (pcO.OOl); and (z'v) being bare below the elbows (p=0.000). In general, specialist and other categories of healthcare staff (dieticians, physiotherapists and radiographers) were poorly compliant with the donning of disposable surgical gloves and the donning of a disposable plastic apron. Medical officers were also poorly compliant with the donning of a disposable plastic apron. Compliance with being bare below the elbows was generally poor among doctors.
Post-hoc analysis for step 3 (interlacing of the fingers) of the hand cleansing procedure indicated that specialists were significantly more compliant than registrars (p=0.002), registered nurses (p=0.001) and enrolled nurses (p=0.004), while medical officers were significantly more compliant than registratrs (p=0.000), registered nurses (p=0.000) and enrolled nurses (p=0.013), and other categories of healthcare staff (dieticians, physiotherapist and radiographers) were significantly more compliant than registrars (p=0.002) and enrolled nurses (p=0.003).
For the donning of disposable surgical gloves, post-hoc analysis indicated that medical officers were significantly more compliant than specialists (p=0.010) and other categories of healthcare staff (dieticians, physiotherapist and radiographers) (p=0.039), while registered nurses were significantly more compliant than specialists (p<0.001) and medical officers (p=0.026) and enrolled nurses were significantly more compliant than specialists (p=0.003).
Post-hoc analysis for the donning of a disposable plastic apron indicated that medical officers were significantly more compliant than registrars (p=0.031), while registered nurses were significantly more compliant than specialists (p<0.001), registrars (p<0.001) and medical officers (p<0.001). Furthermore, enrolled nurses were significantly more compliant than specialists (p=0.002), registrars (p<0.001) and medical officers (p<0.001), and other categories of healthcare staff (dieticians, physiotherapist and radiographers) were more compliant than registrars (p<0.001) and medical officers (p<0.001).
With regard to being bare below the elbows, post-hoc analysis indicated that registered nurses were significantly more compliant than specialists (p=0.000), registrars (p=0.000) and medical officers (p=0.000), while enrolled nurses were signiificantly more compliant than specialists (p=0.000), registrars (p=0.000), medical officers (p=0.000) and registered nurses (p=0.038), and other categories of healthcare staff (dieticians, physiotherapist and radiographers) were significantly more compliant than specialists (p=0.000), registrars (p=0.000), medical officers (p=0.000) and registered nurses (p=0.015).
Discussion
The practice of hand hygiene has been proven to considerably decrease the prevalence of multidrug-resistant infection in the ICUJ16] The 'five moments' of hand hygiene along with direct observation have been shown to be the 'gold standard' when measuring hand hygiene compliance.^ In the present study, handwashing with either soap and water or an alcohol-based hand rub was only performed in just over half the number of opportunities where they were indicated (57.1% and 53.0%, respectively). Historically, best-practice hand hygiene compliance rates have ranged from <40% to as high as 80%.[7-19] According to the WHO, hand hygiene practices below 60% are considered poor, while those exceeding 90% are considered excellent[16]
Except for rotational rubbing of the fingers (80,7%) and turning off the water without contaminating the hands (14.6%), overall compliance was >85% for most of the steps of hand cleansing in this study. Comparatively, Park et al[20] assessed five items of handwashing and reported compliance with the various steps of hand hygiene that ranged between 8.5% and 99.9%, with a marked incremental decline noted from step 1 to step 5. Drying of the hands with a paper towel should not be regarded as an insignificant step in the procedure of hand cleansing, as this step is of value in removing persistent bacteria beneath layers of dead skin[21] Of note, subjects in the current study used paper towel to dry their hands in almost all handwashing opportunities (97.6%).
The primary role of disposable surgical gloves, disposable plastic aprons and other PPE is to diminish the risk of pathogen transmission between patients, healthcare workers and the environment.[22]Compared with previous studies where compliance rates ranged between 12% and 94%,[23,241] in this study disposable surgical gloves were used in 90.6% of opportunities in which they were indicated. It is important to note that the need for hand cleansing is not eliminated when disposable surgical gloves are used, and it should still be performed prior to donning as well as after removal of gloves. [25] Although our study did not report on this, other studies have indicated that healthcare workers are unlikely to cleanse their hands after removal of disposable surgical gloves.[26,27]
The use of a disposable plastic apron is recommended when there is a risk of clothing being exposed to blood, body fluids, secretions or excretions during direct patient care. In this study, a disposable plastic apron was only used in 71.1% of opportunities where it was indicated. Surprisingly, compliance with the use of disposable plastic aprons has not been reported previously.
In the present study, compliance with being bare below the elbows was <50%. Although the practice of being bare below the elbows is generally encouraged, its benefits are debatable. A study in the UK did not report a difference in clinically significant organisms or the number of colony-forming units between healthcare workers who either observed or did not observe being bare below the elbows[28] Additionally, a randomised controlled trial in the USA did not report any significant differences in bacterial contamination of the wrists and clothing between doctors wearing white coats and doctors wearing newly laundered short-sleeved uniforms.[29] However, bacteria have been shown to be present in higher quantities underneath jewellery compared with other areas of the skin.[9] In fact, one study reported that Gram-negative bacilli persisted for several months under the jewellery of 40% of nursing staff.[30]
Senior staff members have been shown to be less compliant than more junior ones with hygiene practices in the healthcare environment.[31,32] Although in the present study there were no significant differences between doctors and nurses with regard to complying with the various steps of hand hygiene (except for interlacing of the fingers), doctors were generally less compliant with the appropriate use of disposable surgical gloves, disposable plastic aprons and being bare below the elbows. The low rates among allied healthcare staff in this study are also of concern.
Study limitations
A limitation of this study is that it was a single-centre study. Hygiene practices are influenced by various factors, such as the presence and proactiveness of an infection control team, the quantity and location of washbasins and alcohol-rub dispensers, and frequency of healthcare worker education and reminders, which may differ from facility to facility.[33,34] Other limitations are that data were not collected after 20h00, when peer oversight and monitoring are generally lacking and hygiene practices may therefore differ from those during daytime hours. Also, the relationship of handwashing frequency to the incidence of HCAIs was not studied. Despite these limitations, it is hoped that the findings of this study will improve hygiene compliance across ICUs in SA and other regions by encouraging the implementation of various strategies such as regular internal audits, increasing the availability and accessibility of washbasins and alcohol-based hand rub, regular training and retraining of staff, and frequent reminders.[35]
Conclusions
Compliance with the correct method of hand hygiene (soap and water v. alcohol-based hand rub), correctly performing the recommended steps of hand hygiene, donning of disposable surgical gloves, donning of a plastic apron and being bare below the elbows was suboptimal in this study, but in keeping with general international trends. Strategies such as regular internal audits, increasing availability and accessibility of washbasins and alcohol-based hand rub, regular training and retraining of staff and frequent reminders are recommended to improve compliance with hygiene practices.
Declaration. None.
Acknowledgements. None.
Author contributions. AEL: primary and corresponding author, conceptualisation of the study, data analysis and preparation and approval of the final manuscript; L-RvR: data collection, literature review, data analysis and preparation and approval of the final manuscript; LG: data collection and preparation and approval of the final manuscript; GR: study design and preparation and approval of the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Trubiano JA, Padiglione AA. Nosocomial infections in the intensive care unit. Anaesth Intensive Care Med 2015;16(12):598-602. https://doi.org/10.1016/j.mpaic.2015.09.010 [ Links ]
2. Vincent J-L. Nosocomial infections in adult intensive-care units. Lancet 2003;361(9374):2068-2077. https://doi.org/10.1016/S0140-6736(03)13644-6 [ Links ]
3. World Health Organization. Health care-associated infections fact sheet. https://www.who.int/gpsc/country_work/gpsc_ccisc_fact_sheet_en.pdf (accessed 7 September 2019). [ Links ]
4. Kretzer EK, Larson EL. Behavioral interventions to improve infection control practices. Am J Infect Control 1998;26(3):245-253. https://doi.org/10.1016/s0196-6553(98)80008-4 [ Links ]
5. Blot S. Limiting the attributable mortality ofnosocomial infection and multidrug resistance in intensive care units. Clin Microbiol Infect 2008;14(1):5-13. https://doi.org/10.1111/j.1469-0691.2007.01835.x [ Links ]
6. Tschudin-Sutter S, Sepulcri D, Dangel M, Schuhmacher H, Widmer AF. Compliance with the World Health Organization hand hygiene technique: A prospective observational study. Infect Control Hosp Epidemiol 2015;36(4):482-483. https://doi.org/10.1017/ice.2014.82 [ Links ]
7. Luangasanatip N, Hongsuwan M, Limmathurotsakul D, et al Comparative efficacy of interventions to promote hand hygiene in hospital: Systematic review and network meta-analysis. BMJ 2015;351:h3728. https://doi.org/10.1136/bmj.h3728 [ Links ]
8. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First global patient safety challenge: Clean care is safer care. 2009. https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_ eng.pdfjsessionid=F80AA90D81CC2611FE45552A17AF27F0?sequence=1 (accessed 12 September 2019). [ Links ]
9. Loveday HP, Wilson JA, Pratt RJ, et al epic3: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014;86(Suppl 1):S1-S70. https://doi.org/10.1016/S0195-6701(13)60012-2 [ Links ]
10. World Health Organization. Practical guidelines for infection control in health care facilities. https://apps.who.int/iris/handle/10665/206946 (accessed 18 September 2019). [ Links ]
11. Canham L. The first step in infection control is hand hygiene. Dent Assist 2011;80(1):42-46. [ Links ]
12. Lambe KA, Lydon S, Madden C, et al Hand hygiene compliance in the ICU. Crit Care Med 2019;47(9):1251-1257. https://doi.org/10.1097/CCM.0000000000003868 [ Links ]
13. Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. MMWR Morb Mortal Wkly Rep 2002;51:RR-16. https://www.cdc.gov/mmwr/PDF/rr/rr5116.pdf (accessed 17 September 2019). [ Links ]
14. Candlin J, Stark S. Plastic apron wear during direct patient care. Nurs Stand 2005;20(2):41-46. https://doi.org/10.7748/ns2005.09.20.2.41.c3957 [ Links ]
15. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007;335(7624):806-808. https://doi.org/10.1136/bmj.39335.541782.AD [ Links ]
16. World Health Organization. Evidence of hand hygiene to reduce transmission and infections by multi-drug resistant organisms in health-care settings. https://www.who.int/gpsc/5may/MDRO_literature-review.pdf (accessed 8 September 2019). [ Links ]
17. Fitzpatrick KR Pantle AC, McLaws M-L, Hughes CF. Culture change for hand hygiene: Clean hands save lives, part II. Med J Aust 2009;191(S8):S13-S17. https://doi.org/10.5694/j.1326-5377.2009.tb02900.x [ Links ]
18. Allegranzi B, Sax H, Pittet D. Hand hygiene and healthcare system change within multi-modal promotion: A narrative review. J Hosp Infect 2013;83(Suppl 1):S3-S10. https://doi.org/10.1016/S0195-6701(13)60003-1 [ Links ]
19. Qushmaq IA, Heels-Ansdell D, Cook DJ, Loeb MB, Meade MO. Hand hygiene in the intensive care unit: Prospective observations of clinical practice. Pol Arch Med Wewn 2008;118(10):543-547. [ Links ]
20. Park H-Y, Kim S-K, Lim Y-J, et al. Assessment of the appropriateness of hand surface coverage for health care workers according to World Health Organization hand hygiene guidelines. Am J Infect Control 2014;42(5):559-561. https://doi.org/10.1016/j.ajic.2013.12.014 [ Links ]
21. Tibballs J. Teaching hospital medical staff to handwash. Med J Aust 1996;164(7):395-398. https://doi.org/10.5694/j.1326-5377.1996.tb124899.x [ Links ]
22. National Institute for Health and Care Excellence (NICE). Healthcare-associated infections: Prevention and control in primary and community care. 28 March 2012. https://www.nice.org.uk/guidance/cg139/resources/healthcareassociated-infections-prevention-and-control-in-primary-andcommunity-care-35109518767045 (accessed 12 October 2019). [ Links ]
23. Flores A, Pevalin DJ. Healthcare workers' compliance with glove use and the effect of glove use on hand hygiene co^liance. Br J Infect Control 2006;7(6):15-19. https://doi.org/10.1177/14690446060070060501 [ Links ]
24. Girou E, Chai SHT, Oppein F, et al. Misuse of gloves: The foundation for poor compliance with hand hygiene and potential for microbial transmission? J Hosp Infect 2004;57(2) :162-169. https://doi.org/10.1016/j.jhin.2004.03.010 [ Links ]
25. Pittet D. Improving adherence to hand hygiene practice: A multidisciplinary approach. Emerg Infect Dis 2001;7(2):234-240. https://doi.org/10.3201/eid0702.010217 [ Links ]
26. Larson E. Compilance with isolation technique. Am J Infect Control 1983;11(6):221-225. https://doi.org/10.1016/0196-6553(83)90004-4 [ Links ]
27. Thompson BL, Dwyer DM, Ussery XT, Denman S, Vacek P, Schwartz B. Handwashing and glove use in a long-term-care facility. Infect Control Hosp Epidemiol 1997;18(2):97-103. https://doi.org/10.1086/647562 [ Links ]
28. Willis-Owen CA, Subramanian P, Kumari P, Houlihan-Burne D. Effects of 'bare below the elbows' policy on hand contamination of 92 hospital doctors in a district general hospital. J Hosp Infect 2010;75(2):116-119. https://doi.org/10.1016/j.jhin.2009.12.013 [ Links ]
29. Burden M, Cervantes L, Weed D, Keniston A, Price CS, Albert RK. Newly cleaned physician uniforms and infrequently washed white coats have similar rates of bacterial contamination after an 8-hour workday: A randomized controlled trial. J Hosp Med 2011;6(4):177-182. https://doi.org/10.1002/jhm.864 [ Links ]
30. Hartstein AI, Denny MA, Morthland VH, LeMonte AM, Pfaller MA. Control of methicillin-resistant Staphylococcus aureus in a hospital and an intensive care unit. Infect Control Hosp Epidemiol 1995;16(7):405-411. https://doi.org/10.1086/647138 [ Links ]
31. Lankford MG, Zembower TR Trick WE, Hacek DM, Noskin GA, Peterson LR Influence of role models and hospital design on the hand hygiene of health-care workers. Emerg Infect Dis 2003;9(2):217-223. https://doi.org/10.3201/eid0902.020249 [ Links ]
32. Pittet D. Compliance with handwashing in a teaching hospital. Ann Intern Med 1999;130(2):126-130. https://doi.org/10.7326/0003-4819-130-2-199901190-00006 [ Links ]
33. Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. Handwashing compliance by health care workers. Arch Intern Med 2000;160(7):1017-1021. https://doi.org/10.1001/archinte.160.7.1017 [ Links ]
34. Allegranzi B, Gayet-Ageron A, Damani N, et al. Global implementation of WHO's multimodal strategy for improvement of hand hygiene: A quasi-experimental study. Lancet Infect Dis 2013;13(10):843-851. https://doi.org/10.1016/S1473-3099(13)70163-4 [ Links ]
35. Gould DJ, Moralejo D, Drey N, Chudleigh JH, Taljaard M. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev 2017, Issue 9. Art. No.: CD005186. https://doi.org/10.1002/14651858.CD005186.pub4 [ Links ]
 Correspondence:
Correspondence:
A E Laher
abdullahlaher@msn.com
Accepted 3 April 2020














