Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.110 n.8 Pretoria Aug. 2020
http://dx.doi.org/10.7196/SAMJ.2020.v110i8.14957
CORRESPONDENCE
Evolution of the SAMPLAR box: A multipurpose tool to facilitate limited re-use of personal protective equipment in low- and middle-income countries
To the Editor: The SARS-CoV-2 pandemic has created unprecedented challenges for low- and middle-income countries (LMICs) in which health systems are profoundly under-resourced.[1] In sub-Saharan Africa, the doctor-to-patient ratio is 0.22 per 1 000 compared with 3.57 in Europe and 2.59 in North America.[2] In the context of limited supplies and staff along with a predicted increase in SARS-CoV-2 cases, innovation is required.
Effective measures to sterilise personal protective equipment (PPE) have been demonstrated, but data are sparse on decreasing contact with infectious droplets in LMICs.[3,4] In an attempt to address the shortfall of PPE and allow limited re-use, the SAMPLAR (safe, affordable, multipurpose, light, aerosol-reducing) box was developed for use in paediatric settings to protect personnel through a cost-effective, partially negative pressure environment.
It is hypothesised that SARS-CoV-2 infectivity extends beyond transmission via respiratory droplets, with the virus displaying stability and persistence in aerosol form.[5] SARS-CoV-2 has demonstrated a half-life suspended in air of 1.1 - 1.2 hours, giving credibility to aerosol and fomite transmission.[6]
The SAMPLAR box comprises access ports for an assistant to stabilise the patient's head and introduce testing swabs, an oxygen inflow point, and an antimicrobial particulate filter that connects to in-wall suction to create negative pressure. This device can be implemented easily in general wards where multiple patients are managed and access to isolation cubicles is limited. The SAMPLAR box allows rapid testing of patients and may mitigate contact with aerosolised viral particles during procedures such as nebulisation, high-flow oxygen provision, and invasive and non-invasive ventilation.
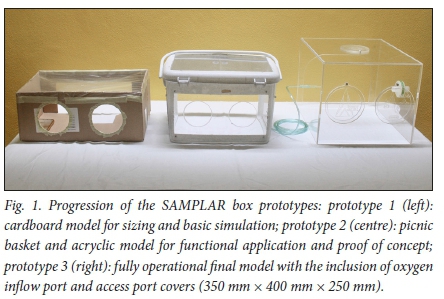
Fig. 1 illustrates the evolution of the SAMPLAR box. Prototype 1 was built from a cardboard box, allowing the desired dimensions to be assessed for suitability and functionality; sterility and reuse were not possible. Prototype 2 was developed using a plastic picnic basket, clear acrylic sheets and a functional antimicrobial filter. Initial testing showed it to be effective and simple to clean. Additions to prototype 3 included a transparent clear acrylic construction, an oxygen inflow point, and covers for all access ports. Practical application of the device includes the addition of a plastic sheet draped over the patient and secured to the box, allowing further containment of aerosolised droplets within this partially negative pressure setting. This prototype is being further modified to allow easier cleaning and sterilisation of the inner surfaces of the box and calculations of time required to clear contained aerosol.
This device was developed in response to the need to protect staff in the global context of a PPE shortage. The low-cost, patent-free design allows clinicians in LMICs to implement and further develop this tool in their own hospitals, both during and beyond the current pandemic. Increased protection for healthcare workers is vital in settings where understaffing is severe, and this problem could be addressed through scaleable implementation of the SAMPLAR box.
Shaegan Irusen
Division of Paediatric Nephrology, Department of Paediatrics and Child Health, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa shaegan.irusen@wits.ac.za
Rossella M Bandini
Department of Paediatrics and Child Health, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Khumo H Myezo, Jennifer A Geel
Division of Paediatric Oncology and Haematology, Department of Paediatrics and Child Health, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
References
1. Sengupta S, Barman P, Lo J. Opportunities to overcome implementation challenges of infection prevention and control in low-middle income countries. Curr Treat Options Infect Dis 2019;11(3):267-280. https://doi.org/10.1007/s40506-019-00200-w [ Links ]
2. World Bank. Physicians (per 1,000 people). Data.worldbank.org. 2020. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS (accessed 17 May 2020). [ Links ]
3. Jinadatha C, Simmons S, Dale C, et al. Disinfecting personal protective equipment with pulsed xenon ultraviolet as a risk mitigation strategy for health care workers. Am J Infect Control 2015;43(4):412-414. https://doi.org/10.1016/j.ajic.2015.01.013 [ Links ]
4. Caeiro J, Garzón M. Controlling infectious disease outbreaks in low-income and middle-income countries. Curr Treat Options Infect Dis 2018;10(1):55-64. https://doi.org/10.1007/s40506-018-0154-z [ Links ]
5. Setti L, Passarini F, de Gennaro G, et al. Airborne transmission route of COVID-19: Why 2 meters/6 feet of inter-personal distance could not be enough. Int J Environ Res Public Health 2020;17(8):2932.https://doi.org/10.3390/ijerph17082932 [ Links ]
6. Von Doremalen N, Bushmaker T, Morris D, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:1564-1567. https://doi.org/10.1056/NEJMc2004973 [ Links ]














