Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.110 no.6 Pretoria Jun. 2020
http://dx.doi.org/10.7196/SAMJ.2020.v110i6.14355
RESEARCH
Thirty-day readmission rate: A predictor of initial surgical severity or quality of surgical care? A regional hospital analysis
PCS SnydersI; O SwartII, III; R C DuvenageIV, V
IMB ChB; Department of General Surgery, Worcester Hospital, South Africa
IIMB ChB, FCS (SA), MSc Clin Epi; Department of General Surgery, Worcester Hospital, South Africa
IIIMB ChB, FCS (SA), MSc Clin Epi; Ukwanda Centre for Rural Health, Stellenbosch University, Worcester, South Africa
IVMB ChB, MMed (Surgery); Department of General Surgery, Worcester Hospital, South Africa
VMB ChB, MMed (Surgery); Ukwanda Centre for Rural Health, Stellenbosch University, Worcester, South Africa
ABSTRACT
BACKGROUND. Unplanned readmission within 30 days is currently being used in high-income countries (HICs) for measuring the quality of surgical care. Surgical site infection (SSI), abdominal complaints and pain are the most common causes for such readmission. The correlation between readmission rates and mortality, increased patient volumes and complexity of surgery remains controversial.
OBJECTIVES. To explore the risk factors for unplanned readmission in the surgical population in a low- and middle-income country setting.
METHODS. This is a retrospective review of prospectively collected data of unplanned 30-day readmissions from January 2014 to December 2017 in the Department of General Surgery, Worcester Hospital, South Africa (SA). Basic patient demographics, reasons for readmission, operative urgency and severity, wound class, length of stay and final outcomes were used to compare the inpatient cohort and identify predictors for unplanned readmission.
RESULTS. A total of 9 649 patients were admitted to the general surgery department at Worcester Hospital - 2.87% (n=270) were unplanned readmissions within 30 days. The mean age of this cohort was 42 (standard deviation (SD) 22) years, with 61% male patients. SSI (60.37%; n=163), gastrointestinal complications (24.44%; n=66) and blood transfusion (7.03%; n=19) were the most common causes for readmission. Median initial length of stay (LOS) was 4 days; after readmission it was 5 days. Readmissions were responsible for 1914 additional patient days. Operative Portsmouth-POSSUM (P-POSSUM) (Physiological and Operative Severity Score for the enumeration of Mortality and morbidity) score (p<0.001), increase in operative wound classification (p=0.001) and emergency surgical procedures (p=0.001) were significant risk factors for readmission within 30 days.
CONCLUSIONS. The Department of General Surgery, Worcester Hospital, had a readmission rate comparable with that in HICs. Readmission rate is an indicator of advanced surgical pathology requiring an operative intervention of greater magnitude, often presenting as an emergency. Our results can be used to improve postoperative surveillance and ultimately improve outcomes in high-risk surgical populations. This study provides a benchmark for other regional hospitals in SA and has implications for quality-improvement programmes.
The 30-day hospital readmission rate following surgery is used in certain countries as an indicator of the quality of surgical patient care.[1-6] This readmission rate may be used to review patient care, identify areas of potential improvement, reduce risk of adverse outcomes and also penalise poor-performing institutions.[2,4,7] Most of the published literature originates from the USA owing to the implementation of a national readmission reduction programme in that country, which was passed as part of the Patient Protection and Affordable Care Act of 2010. The cost of readmissions in the USA was estimated at USD17 billion annually[4,8] South Africa (SA) does not have similar legislation.
Studies from the USA and other high-income countries (HICs) identified surgical site infection (SSI), intestinal obstruction, abdominal complaints including nausea and vomiting, respiratory complications including pneumonia, blood transfusion, failure to thrive and pain management as the most common factors associated with readmission within 30 days from discharge after surgery[1,9] No such data exist for SA or other sub-Saharan low- and middle-income countries (LMICs).
The aim of the study is an analysis of the 30-day readmission rate and underlying risk factors responsible for 30-day readmission of surgical patients treated at Worcester Hospital, a regional hospital in Western Cape Province, SA. The information will be used to identify surgical patients at risk for readmission, potentially to increase post-discharge surveillance. The data could form the basis for a quality-improvement programme in a LMIC setting and could lead to decreased hospital costs and improved patient outcomes.
Methods
A retrospective review was performed of prospectively collected data of unplanned 30-day readmissions over 4 years, from January 2014 to December 2017, in the Department of General Surgery at Worcester Hospital. The hospital functions as the primary referral centre for 8 district hospitals and services a rural population of 660 000, according to the 2011 national census. More than 80% of this population are dependent on public health services.
Data were analysed to calculate the rate of and reasons for readmission. To determine predictors for unplanned readmission, basic patient demographics (age and gender) were collected and potential risk factors identified. Non-operatively managed patients were excluded from the assessment of operative severity. Operative severity and physiological derangement were classified according to the Portsmouth-POSSUM (P-POSSUM) (Physiological and Operative Severity Score for the eNumeration of Mortality and morbidity) score, and operative wounds according to the Centers for Disease Control and Prevention and National Healthcare Safety Network (CDC/NHSN) grading system (available since October 2015) as an indicator of SSI risk.[10] Operative severity and wound class were transformed to binary categorical variables to assist analysis. The mean P-POSSUM of the operative cohort was used to risk stratify operative severity into two categorical groups: group 1:6- 12, and group 2: 13 - 48. SSI was divided into low-risk (clean and clean-contaminated) and high-risk (contaminated and dirty/infected) wounds. Operative urgency was divided into emergency and elective surgery. These variables were used for direct comparative analysis. Those that were significant formed part of further multivariable regression models to adjust for potential confounding factors. Analysis of the readmission trend over this time period was also done. Statistical analysis was performed using Stata 15 (StataCorp., USA); p<0.05 was considered statistically significant.
Results
A total of 9 649 patients were admitted to the Department of General Surgery, Worcester Hospital, from January 2014 to December 2017. Two hundred and seventy of these patients were unexpectedly readmitted within 30 days of discharge - a readmission rate of 2.87%. The basic demographical details of the study population are shown in Table 1. The 30-day readmission group stayed 2 days longer during their initial admission (p<0.001). The subsequent readmission median length of stay (LOS) of 5 days (interquartile range (IQR) 3-9) was responsible for 1914 additional patient days.
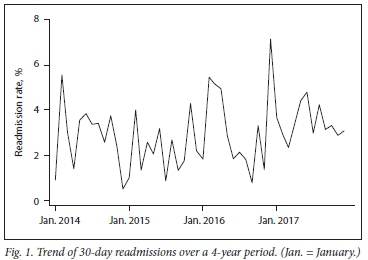
Unadjusted non-parametric trend analysis over the 4 years showed no increase in the 30-day readmission rate (p=0.25) (Fig. 1). This rate remained constant, even though the overall number of admissions increased significantly over the same period against the background of fixed resources.
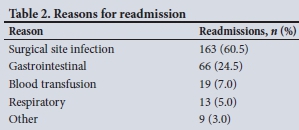
The most common reasons for readmission within 30 days were SSI (60.5%) and gastrointestinal complications (24.5%) consisting of ileus, bowel obstruction, non-infected wound management, nausea, vomiting, constipation and diarrhoea (Table 2).
In the readmission group, 202 patients underwent surgery during initial presentation compared with 7 250 over the 4-year period. The mean P-POSSUM score of the total number of operations performed was 10.9 (standard deviation (SD) 4.7) compared with 13.0 (4.9) for the readmission group. The mean difference in operative P-POSSUM score was 2.1 (95% confidence interval (CI) 1.4 - 2.7; p<0.001). The mean score was used as a guideline to risk stratify into 2 categorical groups: group 1: 6 - 12, and group 2: 13 - 48. The operative cohort comprised 33.3% in group 2 compared with 52.5% of those readmitted within 30 days. Those in the more severe P-POSSUM group (group 2) had more than double (odds ratio (OR) 2.18; 95% CI 1.6 - 2.9;p<0.001) the risk of being readmitted within 30 days after discharge than those in group 1.
Patients with surgical wounds at a higher risk for developing SSI (group B) comprised 39.2% of the total operative cohort compared with 59.4% of the initial operations performed in patients readmitted within 30 days of discharge. The presence of a contaminated or dirty/infected wound (group B) during surgery was twice (OR 2.2; 95% CI 1.7 - 3.1; p<0.001) as likely to result in an unplanned 30-day readmission than in those in group A.
Regression analysis showed that an increase in operative P-POSSUM score (p<0.001), increase in the operative wound grade (p=0.001) and emergency surgical procedures (p=0.001) remained statistically significant risk factors for readmission within 30 days (Table 3) in a multivariable logistical model.
Discussion
The Department of General Surgery at Worcester Hospital had a readmission rate of 2.87% from January 2014 to December 2017, without an increased trend, which is similar to that found in studies done in HICs.[2,5,7,11,12] SSI (60%) and gastrointestinal complications (24.5%) were the most common reasons for readmission. Operative magnitude, emergency surgery and high-risk surgical wounds contributed significantly to the risk of readmission.
Incomplete capturing of patient comorbid disease data over this period, excluding it as a factor in this readmission risk model, is a major weakness of this study. Only readmissions to regional hospitals were analysed. Details of patients with minor complications of surgery performed at a regional level and readmitted to a primary level/district hospital were not recorded. This led to an underestimation of the true readmission rate. All readmitted patients requiring re-operation or more specialised surgical care would have been referred to the regional hospital. The recorded 30-day readmission rate therefore only identifies patients readmitted to the index hospital and not those who died within 30 days of discharge, or those readmitted to emergency centres or other institutions.
The unadjusted non-stratified 30-day readmission rate in general surgery, although easy to measure, is a poor marker for quality of care. As shown in our study, those readmitted mostly represent a subset of the surgical population who are in a poorer physiological state, have more advanced surgical pathology on initial presentation and require operative interventions of greater magnitude. They also represent a small proportion of the total number of patients managed and their quality of life after discharge is not measured. Readmission rates in general surgery cannot be used as a punitive measure against surgical units or for comparison with other specialties.
This study has shown that certain factors predict which patients are expected to develop a complication and potentially be readmitted after surgery. The information can be used to design a prediction tool that can be applied to assess each individual patient's potential readmission or complication risk. This will assist clinicians and surgical units, in conjunction with primary healthcare providers, to establish more effective follow-up for high-risk patients. Individualised post-surgery surveillance strategies will assist in identifying complications early, improve rapid referral to regional centres and limit the morbidity and costs associated with delayed readmissions. A more appropriate cohort on whom to assess the quality of surgical care are patients who were readmitted unexpectedly after surgery, while predicted to be of low risk for surgical morbidity.
Conclusions
A unplanned 30-day readmission rate provides valuable insight into patient physiology and the effect of operative magnitude on surgical outcomes, rather than being an indicator of the quality of surgical care. This information can play an important role in developing tools that identify patients at risk for surgical morbidity, guide improved postoperative surveillance and act as a benchmark for similar studies in LMICs.
Declaration. None.
Acknowledgements. The authors would like to thank Dr O Swart for continued support and input.
Author contributions. All authors contributed significantly to the preparation of the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Mclntyre LK, Arbabi S, Robinson EF, Maier RV. Analysis of risk factors for patient readmission 30 days following discharge from general surgery JAMA Surg 2016;151(9):855-861. https://doi.org/10.1001/jamasurg.2016.1258 [ Links ]
2. Lee MJ, Daniels SL, Wild JRL, Wilson TR, SYSuRG RAGeS Group. Readmissions after general surgery. A prospective multicenter audit J Surg Res 2017;209:53-59. https://doi.org/10.1016/j.jss.2016.09.020 [ Links ]
3. Dimick JB, Miller DC. Hospital readmission after surgery. No place like home. Lancet 2015;386:837-839. https://doi.org/10.1016/s0140-6736(15)60462-7 [ Links ]
4. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360(14):1418-1428. https://doi.org/10.1056/nejmsa0803563 [ Links ]
5. Tsai TC, Orav EJ, Joynt KE. Disparities in surgical 30-day readmission rates for Medicare beneficiaries by race and site of care. Ann Surg 2014;259(6):1086-1090. https://doi.org/10.1097/sla.0000000000000326 [ Links ]
6. Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical readmission rates and quality of hospital care. N Engl J Med 2013;367(12):1134-1142. https://doi.org/10.1056/nejmsa1303118 [ Links ]
7. Wiseman JT, Guzman AM, Fernandes-Taylor S, Engelbert TL, Saunders RS, Kent KC. General and vascular surgery readmissions. A systematic review. J Am Coll Surg 2014;219(3):1-27. https://doi.org/10.1016/j.jamcollsurg.2014.05.007 [ Links ]
8. Clark DE, Ostrander KR, Cushing BM. A multiState model predicting mortality, length of stay, and readmission for surgical patients. Health Serv Res 2016;51(3):1074-1094. https://doi.org/10.1111/1475-6773.12400 [ Links ]
9. Muthuvel G, Tevis SE, Liepert AE, Agarwal SK, Kennedy GD. A composite index for predicting readmission following emersencv general surgery. J Trauma Acute Care Surg 2014;76(6):1467-1472. https://doi.org/10.1097/ta.0000000000000223 [ Links ]
10. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-assoaated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36(5):309-332. https://doi.org/10.1016/j.ajic2008.03.002 [ Links ]
11. Chen Q, Mull HJ, Rosen AK, Borzecki AM, Pilver C, Itani KMF Measuring readmissions after surgery. Do different methods tell the same story? Am J Surg 2016;212(1):24-33. https://doi.org/10.1016/j.amjsurg.2015.08.020 [ Links ]
12. Lefèvre JH, Reboul-Marty J, de Vaugrigneuse S, Zeitoun JD. Readmissions after surgery. A French nationwide cross-sectional study of 1686 602 procedures performed in 2010. World J Surg 2017;41(1):31-38. https://doi.org/10.1007/s00268-016-3740-6 [ Links ]
 Correspondence:
Correspondence:
P C S Snyders
pcssnyders@gmail.com
Accepted 15 October 2019














