Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.110 no.6 Pretoria Jun. 2020
http://dx.doi.org/10.7196/SAMJ.2020.v110i6.14422
RESEARCH
Ever and repeat HIV testing rates among male and female clients: Findings from a reproductive health services integration project in South Africa
C MilfordI; M E BeksinskaI; Z MabudeII; J A SmitI
IPhD; MRU (MatCH Research Unit), Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of the Witwatersrand Durban, South Africa
IIMA; MRU (MatCH Research Unit), Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of the Witwatersrand Durban, South Africa
ABSTRACT
BACKGROUND. HIV testing rates have increased in recent years. Repeat testing is recommended to identify and treat new HIV infections timeously. However, there are limited data on repeat HIV testing, especially in South Africa (SA).
OBJECTIVES. To provide data on repeat HIV testing rates in males and females in a district in SA.
METHODS. A sexual and reproductive health (SRH) service integration model was implemented in seven healthcare facilities in eThekwini District, KwaZulu-Natal Province, SA, between 2009 and 2011. HIV testing data were collected from male and female clients attending these facilities, prior to (baseline) and after the implementation (endline) of the 3-year health services integration intervention.
RESULTS. There were 230 clients at baseline (195 female, 35 male) and 200 at endline (169 female, 31 male). High ever-tested rates were reported at baseline (females 95.4%, males 74.3%) and endline (females 91.7%, males 87.1%), with large increases in male testing rates over time. In addition, high increases were seen between baseline and endline among those who had tested more than once and more than twice in their lifetime. Increases between baseline and endline testing rates were highest in HIV testing services (HTS) (37.0 - 93.3% for clients who had tested more than once, and 11.1 - 53.3% for those who had tested more than twice).
CONCLUSIONS. HIV testing and repeat testing increased over time, especially in males and in HTS. Promotion and integration of SRH services are critical to facilitate improved health-seeking behaviour and HIV testing of both male and female clients. They are also important for continued access to HTS at multiple service delivery points.
Evidence from national surveys shows significant increases in HIV testing in South Africa (SA) over the past 20 years.[1-4] In a national HIV survey conducted in 2017, 70.9% of males and 79.3% of females had been tested for HIV at least once,[2] compared with only 43% of males and 56.7% of females in 2008.[1] This gender disparity in testing rates has been reported previously,[5] and in one study in KwaZulu-Natal Province, SA, less than a fifth (18.5%) of men compared with women had tested for HIV in 2010.[6] Furthermore, factors associated with repeat testing in an SA study included female gender, young age, knowing someone living with HIV, self-referral, and number of prior tests.[5] In addition, it has been reported that clients who view HIV testing as part of routine care (for example, in provider-initiated prenatal screening) may be more comfortable requesting HIV tests in the future.[5,7] Perceptions of not being at risk of HIV infection, and previous HIV-negative results, have been found to reduce uptake of repeat testing.[7] Although repeated HIV testing has been recommended by the World Health Organization (WHO) since 2007,[8] there are only a few studies, most conducted some time ago, reporting repeat testing rates in SA.[5,7,9,10]
The National HIV and AIDS Strategic Plan (NSP) 2017 - 2022[11] promotes universal HIV testing of all sexually active individuals aged >12 years on an annual basis, and consistent with the 90-90-90 approach,[12,13] promotes testing to find the remaining people who do not know their status. Furthermore, the SA government formally adopted a universal test and treat approach in 2016, in support of meeting these 90-90-90 targets.[14] In spite of these efforts, at the end of 2016, ~30% of people globally living with HIV were still unaware of their status.[13] The identification of newly infected people is important for early treatment initiation, and enables individuals to make informed decisions about effective HIV prevention options.[13] The latest SA NSP[11] reported that 10 million people voluntarily test for HIV in SA annually. The previous NSP for SA, 2012 - 2016,[15] highlighted good coverage of testing sites, reporting that nearly all public sector facilities in the country (96%) offered HIV testing services (HTS) to clients.[15] In addition, self-screening has been recommended by the WHO as an additional option for people to test for HIV.[13] Self-screening for HIV is now available in SA, broadening access to testing options, enabling more people to know their HIV status, and facilitating early access to prevention, treatment and care.[16]
Several SA studies have shown that many people who test HIV-positive have CD4+ counts <350 cells/μL[17] and have high viral loads before they start treatment, although the proportion has fallen since the introduction of antiretroviral treatment (ART).[18] It is therefore imperative that if we are to align with the goals of the NSP, HIV testing on a routine and regular basis must be encouraged.
Objectives
We report ever and repeat HIV testing rates of male and female clients attending sexual and reproductive healthcare (SRH) services at healthcare facilities participating in an HIV and SRH services integration model in eThekwini District, KwaZulu-Natal, SA. We used an implementation science approach, and describe any trends in the data that could be attributable to the integration model. We provide recommendations for further research and to inform guideline development to be able to work towards the 90-90-90 goals,[12] to facilitate promotion of HIV testing for prevention, treatment and care.
Methods
Study setting
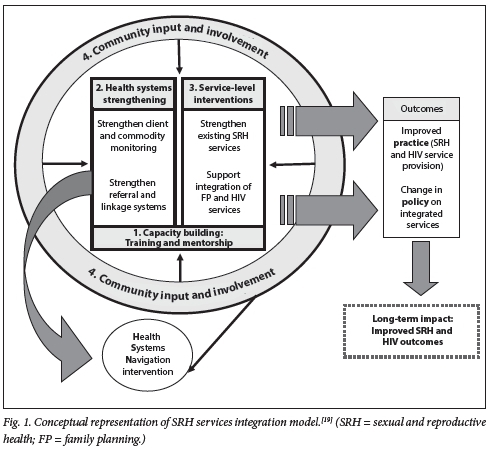
This study was conducted in a district hospital and its six feeder clinics - including five primary healthcare clinics and one community health centre - in eThekwini District. Data were collected as part of a project that implemented a model for integrating SRH and HIV services at subdistrict level.[19-21] Baseline data were collected as part of a cross-sectional survey with healthcare providers and female and male clients in 2009, prior to implementation of the integration model, and cross-sectional endline data were also collected from healthcare providers and male and female clients in 2011. Baseline data from the cross-sectional survey and a facility audit were used to better understand the status of SRH service integration and to inform the model development, and endline data were used to assess the effectiveness of the SRH and HIV services integration model. The final integration model was made up of four interconnected intervention areas, and included (i) health systems strengthening, (ii) service-level activities and interventions, (iii) capacity building, and (iv) community input and involvement[19] (Fig. 1). Various components of the integration model have been evaluated, and its successes and challenges in a resource-limited environment have been described elsewhere.[20,21]
Data collection and analysis
Male and female clients who participated in the cross-sectional surveys were recruited from primary healthcare (PHC), family planning (FP), termination of pregnancy (TOP), antenatal care (ANC, first and repeat visits), immunisation, postnatal care (PNC), sexually transmitted infection and HTS and ART services. The client sample was selected in order to ensure representation of clients attending these SRH services in the different facilities. Where low numbers of clients were attending a particular service, additional clients were purposefully sampled in order to include at least one client per service. We aimed to interview -30-40 clients per clinic, and -50 clients at the hospital, for a total sample size of 250 - 300 clients for baseline, and a further 250 - 300 for the endline components of the integration study. It was considered that this sample was sufficient to ensure reliability of study data for measuring overall integration success.
The survey was conducted as exit interviews - when clients were leaving the facility. Ever and repeat HIV testing rates of the male and female clients were explored and are the focus of this article. To avoid bias, we excluded all those clients who were interviewed in the ART services who would have had an HIV test in the past. The final sample for this study component therefore included 230 clients (195 female and 35 male) at baseline in 2009, and 200 clients (169 female and 31 male) at endline in 2011.
Data were entered into SPSS V25 (IBM, USA), and descriptive analyses were conducted. Pearson's x2was calculated for some categorical variables to determine the significance of differences between baseline and endline data.
Ethical considerations
This study was approved by the Human Research Ethics Committee of the University of the Witwatersrand (ref. no. M080624). Reciprocity approval was granted by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal. In addition, the study was supported by the provincial, district and local departments of health and health facilities within which the research was conducted. All participants were aged >18 years of age and provided written informed consent.
Results
Basic demographic details of participants are presented in Table 1. At both baseline and endline, the majority were unemployed, had some secondary-level schooling (or grade 12), had a regular partner who did not live with them, and had <2 children. A higher proportion of participants in the endline group had >3 children.
Ever-tested rates for male and female clients at baseline and endline were high (baseline: females 94.8%, males 74.3%; endline: females 91.1%, males 87.1%) (Table 2). Although the proportion of females who had ever tested decreased between baseline and endline, the proportion who had tested more than twice increased markedly. For males (all groups), testing history increased between baseline and endline. There were significant differences between baseline and endline for those who had ever tested, those who had tested more than twice, and those who had ever received HIV test results.
Participants who had tested for HIV were asked why they tested (provider v. client initiated, or for insurance purposes) (Table 2). For the majority of female clients, HTS was provider initiated, while for males it was largely client initiated. The proportion of client-initiated testing increased for female clients between baseline and endline. The proportion of provider-initiated testing of male clients increased between baseline and endline. The rate of HTS for insurance purposes was low for both male and female clients (except at baseline, where it was higher than provider-initiated testing for males). Receiving HIV test results decreased for females and increased for males between baseline and endline.
HIV testing history was explored by service/s the client was attending on the day of the survey for male and female clients combined (Table 3). Numbers of male clients were low overall, and some services were only attended by female clients (FP/TOP, ANC, immunisation/PNC). A small portion of clients (just under 10%) attended more than one service, and HIV testing history is reported per service attended and not per client.
All categories of HIV testing (ever tested, tested more than once, and tested more than twice) increased between baseline and endline according to service accessed. The highest increases over time were seen in HTS services, where at endline, 93.3% had tested more than once, compared with 37% at baseline. In the same service (HTS), those who had tested more than twice increased from 11.1% to 53.3% (males and females combined). Lower increases were seen in PHC services, where those who had tested more than once increased from 47.8% to 51.8% and those who had tested more than twice increased from 22.4% to 30.6%.
Discussion
Our data show high HIV testing rates among female and male clients accessing healthcare services in eThekwini District. Repeat testing for both male and female clients increased over time, consistent with other studies that demonstrate increases in testing.[1-4] Provider-initiated testing in females was high at baseline, possibly linked to HIV testing as part of ANC services. Client-initiated testing increased for female clients at endline, demonstrating improved health-seeking behaviour over time, similar to other research that found increased comfort with requesting HIV testing when it was viewed as part of routine care.[5,7] Based on our findings of increased female client-initiated testing over time, and this report of improved comfort requesting HTS when it is part of routine care,[5] further research can be done on who currently initiates testing, views on who should initiate testing, and the acceptability of other approaches to HIV testing, such as HIV self-screening. In addition, research can explore how initiation of testing can be used to lead to improved HTS uptake and more appropriate service delivery.
Male clients' HIV testing rates improved markedly, but despite this they still had gaps in accessing HIV test results. The majority of males self-initiated testing, although the proportion of provider-initiated testing in males increased at endline. There is therefore scope for more healthcare providers to initiate and encourage HIV testing in males, and to facilitate retrieval of test results. Promotion of HTS in male and female clients can encourage self-testing options, but it is also necessary to encourage access through healthcare facilities to facilitate face-to-face counselling. Promotion of HIV testing needs to include the importance of knowing HIV test results, to facilitate access to prevention, treatment and care according to the 90-90-90 goals.[12,14] Furthermore, early identification of HIV-positive status contributes to prevention and can lead to better treatment outcomes.[8]
Although repeat testing rates were low compared with ever-tested rates in our study, more clients underwent repeat tests at endline v. baseline, following implementation of the integration project. While the testing and treatment environment is constantly evolving and improving, it is possible that some of the improvements in testing may be linked to implementation of the integration project. Integration of services is necessary to facilitate access to HTS at multiple service points within a healthcare facility. In our project, the proportion of providers providing HTS increased across all services by endline,[19] which is reflected in the improvements in provider-initiated testing by male clients. These improvements in provider-initiated testing highlight the feasibility of supporting males to access HTS through services that they attend (such as PHC), and of encouraging females to access HTS even when they are not pregnant. The SA government is prioritising integration of services,[22] and findings from this study highlight that integration of HTS in other SRH services is feasible and helpful in promoting increased testing and repeat testing. Recommendations can be made for continued integration of services, and training of healthcare providers to offer ongoing HTS services to meet the 90-90-90 targets.[12]
Study limitations
The data were collected some time ago, and since data collection there have been changes in the HIV testing and treatment environment that may be reflected in changes in testing rates. Despite the fact that the data were collected some time ago, there are limited data on repeat testing practices, so these findings are important for informing guidelines on HTS services and health systems integration practices. Our data focus on HTS in clinic attendees, although HIV self-testing is now recommended and available[13,16] and increasing in acceptability,[23-25] and our data may be different to what is observed in the general population. However, research demonstrates that face-to-face counselling has been viewed as invaluable,[23,25] and people are therefore still likely to access HTS in healthcare facilities. Trends in HIV testing patterns among males and females in this study can be observed and compared with other similar studies. Furthermore, owing to the changing HIV testing and treatment environment during the course of implementation of the integration model, and the lack of a control environment, changes in behaviour could be attributable to a variety of factors. However, the trends observed in HIV testing behaviour over the course of this study are useful as exploratory findings and to inform future research on health services integration. Finally, owing to low numbers of clients (specifically male clients) in some service categories, multivariate analyses were not possible. However, the data are descriptive, and where possible bivariate analyses have been conducted
Conclusions
Data from this study highlight that promotion and integration of SRH services are critical to facilitate improved health-seeking behaviour and HIV testing of both male and female clients, and for continued access to HTS at multiple service delivery points. Increased testing rates are important for early identification of HIV-positive status, HIV prevention and improved treatment outcomes. Guidelines for HTS should also focus on health systems integration as a strategy to improve access to and uptake of HTS.
Declaration. The research for this study was done in partial fulfilment of the requirements for CM's PhD degree at the University of KwaZulu-Natal.
Acknowledgements. This study was supported by a grant from the William and Flora Hewlett Foundation. The authors thank the provincial and district departments of health, the management and staff of participating healthcare facilities, and the clients who gave their time to participate in and support the study activities. They thank the team who provided support to the project and facilitated and conducted the research activities, including Letitia Rambally Greener, Kedibone Sithole, Claudia Ngoloyi. Melanie Drace, Ross Greener, Fiona Scorgie, Jacqueline Pienaar, Muriel Kubeka, Sibusiso Sibiya, Sithembile Chonco and Smangele Faith Luthuli.
Author contributions. CM, MEB, ZM, JAS contributed to the development and assessment of the integration model. CM, MEB, JAS developed and implemented the baseline and endline research. CM and MEB analysed the data. CM and MEB drafted the manuscript. All authors read and contributed to the draft and final versions of the manuscript.
Funding. This research was funded by the William and Flora Hewlett Foundation.
Conflicts of interest. None.
References
1. Shisana O, RehJe T, Simbayi L, et aJ. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey 2008. A Turning Tide among Teenagers? Cape Town. HSRC Press, 2009. [ Links ]
2. Human Sciences Research Council. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. HSRC Launch, 17 July 2018. http://www.hsrc.ac.za/uploads/pageContent/9234/FINAL%20Presentation%20for%2017%20July%201aunch.pdf (accessed 1 August 2018) [ Links ]
3. MakushaT, Mabaso M, Richter L, Desmond C, JoosteS, Simbayi L. Trendsin HIV testing and associated factors among men in South Africa. Evidence from 2005, 2008 and 2012 national population-based household surveys. Public Health 2017;143:1-7. https://doi.org/10.1016/j.puhe.2016.10.017 [ Links ]
4. Rehle TM, Hallett TB, Shisana O, et al. A decline in new HIV infections in South Africa. Estimating HIV incidence from three national HIV surveys in 2002, 2005 and 2008. PloS ONE 2010;5(6):e11094. https://doi.org/10.1371/journal.pone.0011094 [ Links ]
5. Regan S, Losina E, Chetty S, et al. Factors associated with self-reported repeat HIV testing after a negative result in Durban, South Africa. PLoS ONE 2013;8(4):e62362. https://doi.org/10.1371/journal.pone.0062362 [ Links ]
6. Ramkissoon A, Beksinska M, Searle C, Govender T, Smit J, Kleinschmidt I. HIV counseling and testing in an urban reproductive primary health clinic in South Africa. Gender differences among clients. I Acquir Immunce DeficSyndr 2011;58(5):e138-14. https://doi.org/10.1097/QAI.0b013e3182381171 [ Links ]
7. Harichund C, Kunene P, Simelane S, Abdool Karim Q, Moshabela M. Repeat HIV testing practices in the era of HIV self-testing among adults in KwaZulu-Natal, South Africa. PLoS ONE 2019;14(2):e0212343. https://doi.org/10.1371/journal.pone.0212343 [ Links ]
8. Church K, Warren CE, Birdthistle I, et al. Impact of integrated services on HIV testing. A randomised trial among Kenyan family planning clients. Stud Farn Plann 2017;48(2):201-218. https://doi.org/10.1111/sifp.l2022 [ Links ]
9. Kranzer K, van Schaik N, Karmue U, et al. High prevalence of self-reported undiagnosed HIV despite high coverage of HIV testing. A cross-sectional population based sero-survey in South Africa. PLoS ONE 2011;6(9):e25244. https://doi.org/10.1371/journal.pone.0025244 [ Links ]
10. Nglazi MD, van Schaik N, Kranzer K, Lawn SD, Wood R, Bekker L-G. An incentivized HIV counseling and testing program targeting hard-to-reach unemployed men in Cape Town, South Africa. J Acquir Immune Dene Syndr 2012;59(3):e28-e34. https://doi.org/10.1097/QAI.0b013e31824445f0 [ Links ]
11. National Department of Health, South Africa. HIV and AIDS and STI National Strategic Plan for South Africa, 2017 - 2022. Pretoria. NDoH, 2017. https://sanac.org.za//wp-content/uploads/2017/06/NSP_FuliDocument_FINAL.pdf (accessed 4 May 2020). [ Links ]
12. Joint United Nations Programme on HIV/AIDS. 90-90-90. An ambitious treatment target to help end the AIDS epidemic. UNAIDS, 2014. https://www.unaids.org/en/resources/documents/2017/90-90-90 (accessed 4 May 2020). [ Links ]
13. World Health Organization, Joint United Nations Programme on HIV/AIDS. WHO, UNAIDS statement on HIV testing services. New opportunities and ongoing challenges. 2017. https://www.unaids.org/sites/default/nles/media_asset/2017_WHO-UNAIDS_statement_HIV-testing-services_en.pdf (accessed 4 May 2020). [ Links ]
14. National Department of Health, South Africa. Circular. Implementation of the universal test and treat strategy for HIV positive patients and differentiated care for stable patients. 26 August 2016. https://sahivsoc.org/Files/22%208%2016%20Circular%20UTT%20%20%20Decongestion%20CCMT%20Directorate.pdf (accessed 11 November 20lyj. [ Links ]
15. National Department of Health, South Africa. HIV and AIDS and STI Strategic Plan for South Africa, 2012 - 2016. Pretoria. NDoH, 2012. https://www.hst.org.za/publications/NonHST%20Publications/hiv-nsp.pdf (accessed 4 May 2020). [ Links ]
16. Venter F, Majam M, Jankelowitz L, et al. South African HIV self-testing policy and guidance considerations. S Afr J HIV Med 2017;18(1):775. https://doi.org/10.4102/sajhivmed.vl8il.775 [ Links ]
17. Drain PK, Losina E, Parker G, et al. Risk factors for late-stage HIV disease presentation at initial HIV diagnosis in Durban, South Africa. PLoS ONE 2013;8(1):e55305. https://doi.org/10.1371/journal.pone.0055305 [ Links ]
18. Osler M, Hiidebrand K, Goemaere E, et al. The continuing burden of advanced HIV disease over 10 years of increasing antiretroviral therapy coverage in South Africa. Clin Infect Dis 2018;66(Suppl 2):S118-S125. https://doi.org/10.1093/cid/cix1140 [ Links ]
19. Milford C, Scorgie F, Rambally Greener L, et al. Developing a model for integrating sexual and reproductive health services with HIV prevention and care in KwaZulu-Natal, South Africa. BMC Reprod Health 2018;15:189. https://doi.org/10.1186/s12978-018-0633-l [ Links ]
20. Milford C, Rambally Greener L, Beksinska M, Greener R, Mabude Z, Smit J. Provider understandings of and attitudes towards integration. Implementing an HIV and sexual and reproductive health service integration model, South Africa. Afr J AIDS Res 2018;17(2):183-192. https://doi.org/10.2989/16085506.2018.1478314 [ Links ]
21. Milford C, Beksinska M, Rambally Greener L, Mabude Z, Smit J. Implementation of a sexual and reproductive health service integration model. South African providers1 reports. Cogent Med 2019;6(1):1592740. https://doi.org/10.1080/2331205x.2019.1592740 [ Links ]
22. Mantel! JE, Cooper D, Exner TM, et al. Emtonjeni - a structural intervention to integrate sexual and reproductive health into public sector HIV care in Cape Town, South Africa. Results of a phase II study AIDS Behav 2017;21(3):905-922. https://doi.org/10.1007/sl0461-016-1562-z [ Links ]
23. Harichund C, Moshabela M, Kunene P, Abdool Karim Q. Acceptability of HIV self-testing among men and women in KwaZulu-Natal, South Africa. AIDS Care 2019;31(2):186-192. https://doi.org/10.1080/09540121.2018.1503638 [ Links ]
24. Kelvin EA, Cheruviilil S, Christian S, et aL Choice in HIV testing. The acceptability and anticipated use of a self-administered at-home oral HIV test among South Africans. Afr J AIDS Res 2016;15(2):99-108. https://doi.org/10.2989/16085906.2016.1189442.25 [ Links ]
25. Spyrelis A, Abdulla S, Frade S, et aL Are women more likely to self-test? A short report from an acceptability study of the HIV self-testing kit in South Africa. AIDS Care 2017;29(3):339-343. https://doi.org/10.1080/09540121.2016.1234687 [ Links ]
 Correspondence:
Correspondence:
C Milford
cmilford@mru.ac.za
Accepted 22 November 2019














