Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.110 no.6 Pretoria jun. 2020
http://dx.doi.org/10.7196/SAMJ.2020.v110i6.14120
RESEARCH
Analysis of the airway registry from an academic emergency department in South Africa
J C HartI; L N GoldsteinII
IMB ChB, Dip PEC (SA); Division of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, MMed (Emergency Medicine), FCEM (SA), Cert Crit Care (SA) Phys; Division of Emergency Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Airway management is an essential skill for doctors working in the emergency department (ED). Safety and efficacy are crucial to its success. Analysis of an airway registry can provide feedback that can be used for quality improvement purposes.
OBJECTIVES. To examine the first airway registry from an ED in South Africa (SA), a low- to middle-income country (LMIC), and compare the findings with international data.
METHODS. A retrospective analysis of 13 months' data from the airway registry of an academic ED with an annual census of 60 000 patients. Data analysed included demographics, indications for intubation, intubator training level, type of intubation device, number of attempts, adverse events, pre-oxygenation methods, and drug and intravenous fluid use.
RESULTS. A total of 321 intubations were included. The majority of the patients (71.6%) had non-traumatic indications for intubation. The overall first-pass intubation success (EPS) rate for doctors was 81.8%. Although this rate is lower than the mean rate suggested in an international meta-analysis (84.1%), it is within the 95% confidence interval (80.1 - 87.4%). Overall EPS rates showed no difference between video laryngoscopy (81.7%) compared with direct laryngoscopy (73.3%) (p-value 0.079), although better glottic views were obtained with video laryngoscopy (80.5% were Cormack-Lehane grade 1). Analysis of pre-oxygenation methods found that although sicker patients had received more aggressive pre-oxygenation, e.g. with non-invasive or bag-mask ventilation techniques, they still desaturated more often (35.8% and 62.5%, respectively) than less sick patients who received simple non-rebreather facemask pre-oxygenation (4.5%).
CONCLUSIONS. This analysis of the first airway registry from an SA ED highlights that airway management in an LMIC can be performed on par with accepted international standards. It serves as a good baseline for further research into airway management in other LMICs and provides useful feedback for quality improvement purposes.
Airway management is an essential skill for emergency department (ED) doctors. Management of airways in the ED can be fraught with difficulty, from acutely ill patients with deranged physiology to time and resource constraints. In order to ensure that emergency patients always receive the best care, it is necessary to evaluate current practice norms and identify areas that can be improved upon.[1-4] Numerous airway databases already exist around the world, providing insight into the complexity of emergency airway management. These data have been analysed repeatedly to create the many different airway algorithms available today.[1,2,5-8] They assist in providing the necessary insight into clinical practice and aid in identifying areas for improvement.
As emergency medicine develops in South Africa (SA), ED doctors are becoming more skilled in airway management in the ED. International studies have showed widely varying success and complication rates in EDs in North America, Asia, Australasia and Europe, but currently there is very little research available concerning the level of airway management in Africa, and how that standard of care compares with global developed-world standards.[9] The small amount of local data available deal only briefly with success rates, techniques and adverse events (AEs) in an isolated single-centre report.[10]
Objectives
This retrospective analysis from the first airway registry in an SA ED serves as the initial step in understanding how management of emergency patients and their airways can be improved. Our objectives were to analyse first-pass as well as direct laryngoscopy (DL) and video laryngoscopy (VL) success rates; to assess the adequacy of pre-oxygenation; and to compare AE rates and factors affecting patient deterioration during airway management in an SA ED with international data.
Methods
Study setting
This was a retrospective registry review of all patients who required airway interventions in an academic ED in Johannesburg, SA, from 1 September 2015 to 31 October 2016. The ED is staffed by full-time emergency physicians, emergency medicine registrars and medical officers (most with <5 years of postgraduate experience). Interns, paramedics and nursing staff also rotate and train in the ED. The department has an annual census of 60 000 patients, and is a mixed ED treating both trauma and medical emergencies. Because there is a dedicated 'mother and child' hospital nearby, the department sees fewer gynaecological and paediatric cases than other mixed EDs.
Airway management decisions are left to the discretion of the operator; however, a standard pre-procedure checklist is available in the ED protocol book.
Permission to conduct this research was obtained from the hospital ethics committee, as well as the Human Research Ethics Committee of the Faculty of Health Sciences, University of the Witwatersrand (ref. no. M161150).
About the airway registry
The airway registry was started in August 2015. Every patient who required airway intervention (uniformly meaning intubation) was entered into the registry. Records were entered into a pre-designed REDCap (Research Electronic Data Capture) database, a secure web application used for building and maintaining online databases. Access was restricted to the departmental head and registry co-ordinator. Record entry was followed up on a regular basis by the registry co-ordinator to ensure correct recording and consecutive patient sampling. Any missing information was added from hospital records. Patients who required re-intubation for any reason were also recorded in the registry, as were any patients intubated in the ED by non-ED staff. Patients intubated in the operating room or wards and in the pre-hospital environment were not entered in the registry. Doctors working in the ED were all trained in filling out the registry, and regular reminders were distributed via email as well as at the weekly academic round.
The primary airway operator (the intubator) was responsible for retrospectively completing the registry after the patient was stabilised. Information regarding patient demographics; body habitus; pathology; preparation, including preload volume and inotrope use; methods of airway management, including pre-oxygenation, devices used, success or failure, and operator level; drugs used; vital signs and complications was recorded.
Levels of operators were divided into interns (<2 years of post-qualification experience), medical officers (2-5 years of postgraduate training), registrars (>3 years of postgraduate training), and other, which included medical students, paramedic students and trauma nurse trainees. Where the operator level was unclear or not recorded the other' category was checked, and it was indicated further that 'operator was not known'.
In emergency intubation, a failed airway has been defined as there having been three failed attempts to intubate a patient by an experienced operator, even when bag-mask ventilation is capable of maintaining adequate oxygen saturation.[11] Intubation success was therefore defined as passage of an endotracheal tube (ETT) through the vocal cords within three attempts, whereas first-pass success (EPS) was defined as successful intubation by the first operator on the first attempt.[12] A single attempt resulted in either correct placement of the ETT or re-oxygenation and a subsequent attempt. A failed airway was failure to correctly place the ETT within three attempts, necessitating a rescue airway such as a surgical airway or supraglottic device. DL was performed with a standard Macintosh direct laryngoscope, with a choice of size 2-4 blades. The GlideScope video laryngoscope (with a hyper-angulated blade) was used in all video-assisted intubations. Either a size 3 or 4 blade was available, as well as the manufacturer-provided intubating stylet. The choice of DL or VL was at the discretion of the intubator.
Vital signs were recorded from monitors in the ED, which were calibrated regularly and had minute-to-minute recall. Correct monitor placement, time-cycling and blood pressure cuff sizing were done by nursing staff. Significant hypoxaemia was defined as oxygen saturation <90%. A heart rate >100 or <50 bpm or systolic blood pressure <90 mmHg, or a 20% change from baseline of either parameter, were considered significant.
Data collection
Data were extracted in spreadsheet format after each record had been checked for completeness. Any patients aged < 18 years, all obstetric and gynaecology patients, and any patients with incomplete records were excluded. Some data were extracted from patient records where available.
Statistical analysis
All eligible records from the study period were included. Comparison of the EPS rate for DL v. VL was carried out using the z-test for proportions. The x2test was used to assess the relationship between grading of the laryngoscopic view at the first attempt between DL and VL, comparison of the grading for unsuccessful v. successful attempts within each device, determination of the association between desaturation and pre-oxygenation method, and determination of the association between time of intubation and number of attempts at intubation. Fisher's exact test was used for 2x2 tables or where the requirements for the x2test could not be met.
The relationships between number of attempts at intubation and blood pressure, heart rate and oxygen saturation were assessed with the t-test (or analysis of variance for more than two categories). Where the data did not meet the assumptions of these tests, a non-parametric alternative, the Wilcoxon rank-sum test (or the Kruskal-Wallis test for more than two categories), was used. The strength of the associations was measured by Cohens d for parametric tests and the R-value for the non-parametric tests.
Data analysis was carried out using SAS (version 9.4 for Windows, SAS Institute, USA). The 5% significance level was used, except where multiple comparisons were made.
Results
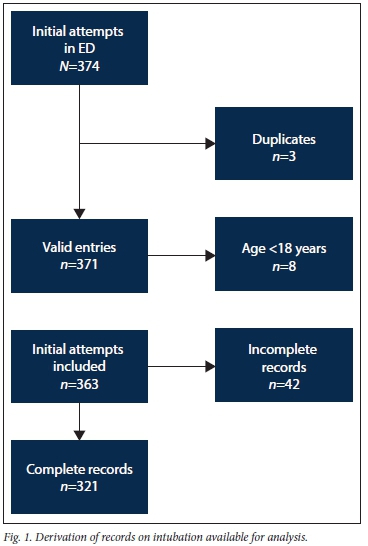
During the study period, a total of 374 records were captured on the registry. Fig. 1 shows the derivation of eligible records. Most of the excluded patients were 'unknown' trauma patients where approximate age was not recorded, and hospital records were missing or incomplete for comparison even on follow-up. The mean patient age was 41 years (range 18 - 91), with males accounting for 58.3% of the study population. Pathologies requiring airway intervention are recorded in Table 1.
Methods of visualisation
Table 1 also shows the FPS of DL and VL, as well as the Cormack-Lehane grading of visualisation[13] for all intubators, including students. The difference in overall success rates of DL and VL was not statistically significant (p=0.079).
Intubation success rates and AEs
The overall FPS rate for doctors was 81.8%. Medical officers and registrars had similar success rates. Fig. 2 depicts the success rates of each level of operator, as well as success after multiple attempts, and rescue attempts. Only 2 patients ultimately had failed intubations: one surgical airway (0.3%) was performed by an emergency physician, and another patient was ventilated with a laryngeal mask airway and later intubated in the operating room. Rescue attempts in Fig. 2 refer to a second operator attempting to intubate the patient after initial attempts by the first operator had failed.

AEs associated with each intubation attempt are summarised in Table 2. Endobronchial (mainstem) intubation was diagnosed clinically. There is no section on the registry for patient follow-up, so the significance of AEs is difficult to quantify past the initial ED evaluation. A total of 207 events occurred in 106 patients, with an overall AE rate of 33.0%.
Pre-oxygenation
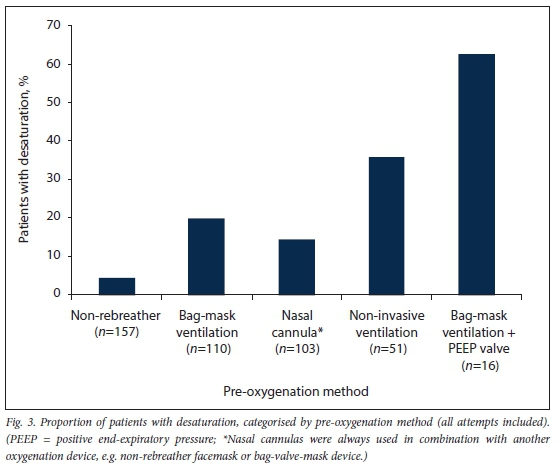
Some patients received more than one method of pre-oxygenation simultaneously: nasal cannulas were never a sole method of pre-oxygenation - they were always combined with another oxygenation device, either a non-rebreather facemask or bag-valve-mask device. In our ED, the bag-valve-mask device does not come standard with a positive end-expiratory pressure (PEEP) valve attached, and it is therefore not utilised for all intubations. Bag-mask ventilation with and without a PEEP valve is therefore presented separately Fig. 3 shows each pre-oxygenation method, with the incidence of desaturation categorised by method. Including all intubation attempts, 52 patients (16.8%) had an oxygen saturation <90% at some point between starting the first attempt and securing the airway.
Factors affecting vital signs
The only factor producing a noticeable effect on patient vital signs in the post-intubation period was the choice of induction drug, although no agent caused a statistically significant change in vital signs. No benzodiazepines were used for induction; 3.7% of patients did not receive any induction agents, and 2.8% received no muscle relaxants. Although 7.4% of intubations were performed due to tardiac arrest', some intubations were performed after return of spontaneous circulation (medications were utilised for intubation) and others were performed during cardiac arrest (no or minimal medications utilised).
Etomidate was used most frequently (n=149), and was associated with the least change in blood pressure and heart rate (a mean decrease of 9 mmHg at 20 minutes from baseline systolic blood pressure). Ketamine was used in 115 patients, with a decrease from baseline of 9 - 12 mmHg. Propofol was used least frequently, in 45 patients, with a decrease of 14 - 18 mmHg from baseline.
There was no association between change in vital signs and number of attempts at intubation, choice of paralysing agent, or use of other premedications (including adrenaline, atropine and midazolam). Time of day of intubation did not have any effect on FPS rates (07h00 - 19h00: 77.8% and 19h00 - 07h00: 75.3%; p=0.69), vital signs or number of intubation attempts.
Discussion
This analysis is the first of its kind from SA, and as such there are very few data with which to compare it. Our single-centre database captured 321 valid patient entries during the 13 months under review. Owing to inadequate hospital records, 11 % of the initial dataset had to be excluded; these were mainly 'unknown trauma patients. Trauma patients present a unique challenge for airway management, and this large group of missing data could represent multiple potentially difficult airways that may have affected our analysis.
Intubation success rates
The overall FPS rate for doctors was 81.8%. Although this rate is slightly lower than the suggested mean ED FPS rate of 84.1% from one meta-analysis of 42 081 intubations in 10 countries, it is within their 95% confidence interval (80.1 -87.4%).[12]Table 3 tabulates and compares the results of our database with other airway databases from EDs around the world. The overall FPS rate in the present study appears to have been affected by the low success rates of the interns, probably due to their limited exposure to emergency airway management prior to their rotation in the ED. Very few of the studies in Table 3 have adequate data to compare each level of operator, but those that do show a wide range of success in the junior group. Directly comparing senior personnel across studies shows a more equivalent success rate.
Most of the comparison studies are multicentre trials from North America. The generalisability of their results to an African context is debatable, especially when considering the resource restrictions in low- and middle-income countries. A Nigerian study of 94 patients (not included in Table 3) documented an 81.9% FPS rate in their ED, but these intubations were mainly performed by anaesthetic registrars (73.9%).[9] They documented an overall AE rate of 93.6% (notably hypotension and desaturation rates of 42.5% and 34.0%, respectively). This seemingly high AE rate was probably due to large delays in securing patients' airways - the mean time to intubation was 129 minutes, for a variety of reasons including lack of staff, drugs and oxygen.[9] A single-centre study from Thailand with 757 patients showed an overall FPS rate of 79.6%, but with a complication rate of 37%. In their ED, which saw only medical patients, most were intubated without muscle relaxants and sedated with benzodiazepines alone, which together were cited as possible causes of their AEs. [14] Several studies have documented increased success rates when using a rapid-sequence intubation technique. The addition of muscle relaxants is associated with an 8 - 16% increase in FPS, as well as decreased complication rates including oesophageal intubation.[3,5,6]
In the present study, 106 patients experienced AEs (33.0%). The number of AEs was not significantly affected by number of intubation attempts, and even fewer AEs were seen after three attempts. This trend is likely to be due to reporting bias, as it does not correspond with the multiple other studies cited above, including the 14% AE rate for single intubation attempts in Sakles etal,'s[4]2013 study, which went up to 53% for multiple attempts.[4]
The number of rescue attempts probably reflects doctors' level of experience. Patients who require intubation in the ED are generally in extremis, and this state may not always permit the intern to 'try again (in order to prevent patient harm), resulting in a higher 'rescue rate' for interns compared with medical officers and registrars, none of whom were documented as needing a rescue intubation. The lack of rescue attempts for senior doctors may also be due to under-reporting of failures, or it may be that registrars are often the most experienced doctors in the ED apart from specialists. In 2013, Sakles et al[6]found that three or more intubation attempts were associated with an AE in up to 70% of cases. Whether rates of first-pass success, adverse events and rescue attempts are due to skilled airway management, reporting biases, ego or staff availability, airway operators should be encouraged to ask for help as early as possible when needed in order to avoid negative patient sequelae.
The rate of surgical airways appears to have declined over time. Sakles et al.[4]reported that the rate of surgical intervention was 1.1% in 1998, whereas in later studies rates are <0.5% (Table 3). While this may not be a significant difference, it represents a change in airway practice over the 20 years between these studies. More tools are available to the ED doctor outside the operating room, and more emphasis is being placed on adequate airway preparation. While many of these methods are not commonplace in the African setting, the basics of adequate preparation, and a logical progression through an airway algorithm', have permeated clinical practice, as is evident by the comparable intubation success and surgical airway rates from the present study.
Visualisation and method of laryngoscopy
Ongoing debate is raging in the emergency medicine community about the usefulness of VL, and loss of the skill of DL.[18] What would happen if the video device had a flat battery? What if the wires or screen were broken? Neither modality could exist without the other and yet the usefulness of VL in the ED is still being determined. Currently, its greatest potential is as a rescue device.[7,19]
In a 2016 Cochrane review by Lewis et al.,[20] VL and DL were compared using the results of 64 studies. Although a large amount of heterogeneity becomes apparent in such a review and all participants were unblinded, the authors concluded that for anticipated difficult airways VL had fewer failed intubations, while in patients without a difficult airway neither option showed more benefit. In a similar meta-analysis by Pieters et al.,[21] specifically of predicted difficult airways, VL was shown to have better glottic views, translating to a 9% higher FPS rate and less mucosal trauma. In contrast, the present study showed that neither modality resulted in a higher success rate, despite VL having substantially better grade 1 Cormack-Lehane views.
Some argue that there may be increased risk in using VL because it could give a false sense of security, as well the 'distraction of a pretty screen' and 'mesmerising views of the glottic inlet'.[22,23] In trauma patients, VL may be negatively affected by blood in the airway, producing longer durations to intubation with associated desaturation.[24] Skill with VL requires careful training and practice with a specific technique. [25,26]A 7-year study by Sakles et al.[27]published in 2014 showed that the FPS rate of GlideScope intubation improved from 74% for first-year registrars up to 90% for third-year registrars, while success rates for DL remained relatively similar for the different experience levels. A potential confounder to this finding is relative lack of training in DL, as VL is used as a rescue device for failed DL, so trainees never get the opportunity to fine-tune the DL skill set.[27]
In the present study, the choice of device was left to the discretion of the airway operator, and VL was the primary method in over half of the intubation attempts. Whether this choice could lead to loss of DL skill as a result of lack of practice or potentially save patients owing to proficiency with VL would require further investigation. Another point to consider is the availability of VL in the SA context. Not every ED has access to this expensive piece of equipment, and anecdotal experience shows that most other EDs primarily use DL, although no studies are currently available to prove this, or the implications thereof.
For our ED, where inexperienced operators often train, one potential benefit of VL is that the teacher sees on a video screen what the student sees during laryngoscopy, allowing real-time feedback while at the same time offering the security for the teacher to take over at any time. There is also an option to watch video playback of the intubation and advise on how to approach the airway better in future.[28]
Pre-oxygenation
In recent years, there has been considerable emphasis on the use of nasal cannula oxygen in conjunction with other pre-oxygenation ('de-nitrogenation') methods, both to aid pre-oxygenation and to provide apnoeic oxygenation'. [29,30]
In our ED, unavailability of end-tidal oxygen detectors as used in other oxygenation studies, as well as relatively infrequent transfer of oxygen saturation parameters to the registry, make the data from the registry insufficient to analyse the apnoeic period. Although the patient's oxygenation is monitored continuously during intubation, the saturation parameters are only recorded in the registry just before the first intubation attempt starts and thereafter every 5 minutes up to 20 minutes post-intubation. However, the available data were used to determine adequacy of pre-oxygenation, using the oxygen saturation before the first intubation attempt as a surrogate.
Most of the patients in the present review received more than one method of pre-oxygenation, with a non-rebreather facemask being the most common - probably as it was most readily available. Only 4.5% of patients in whom this method was used experienced oxygen saturation <90% during their intubation. These patients may have had less severe disease, thereby skewing the success in favour of this method. Any patient requiring additional pre-oxygenation techniques was probably more sick and therefore more likely to desaturate. However, the patient's severity of disease was not recorded in this registry, and so cannot be compared with frequency of desaturation. A single study in 2017 from Minneapolis showed that the concept of using a non-rebreather at 'flush-rate' was superior to standard non-rebreather facemask or bag-mask ventilation, and demonstrated mean expired oxygen levels of 86%.[31] This method, and even standard flow rate at 15 L/min, depends on an awake, spontaneously breathing patient, but should be further investigated in an SA context as it is a simple, inexpensive method of preoxygenation.
The addition of nasal cannulas for the period of preoxygenation has been shown to improve oxygen delivery in masks with improper seals, as well as potentially delay desaturation when used in combination with a non-rebreather mask.[29,32] However, we found no significant benefit in patients who received this form of oxygenation compared with those who did not.
Similarly, patients in whom non-invasive ventilation and bag-mask ventilation with a PEEP valve adaptor were used experienced significant desaturations (35% and 61%, respectively). These rates of desaturation may have been confounded by the fact that the patients who received these types of pre-oxygenation methods were probably more sick with poor reserve, and were therefore prone to more rapid desaturation. This trend contrasts with other smaller studies that have shown that critically ill patients do benefit from increasing mean airway pressure with some type of PEEP device. Baillard et al[33] demonstrated improved oxygen saturation before, during and after intubation when non-invasive ventilation was used for pre-oxygenation, with no increase in AEs due to regurgitation with gastric distension, increased intrathoracic pressure or decreased cardiac output. The benefit may be due to recruitment of alveoli in physiologically shunted lungs, or attenuation of diffusion-atelectasis caused by the process of de-nitrogenation.
Factors affecting vital signs
Various factors examined from the registry may have had the potential to cause post-intubation decompensation. Time of day and additional drugs had no effect on vital signs. Airway operator fatigue might be expected to lead to poorer success rates, but in fact FPS remained equal regardless of day or night.[34,35] Induction agents all affected vital signs, but none was statistically or clinically significant. Most patients returned to pre-intubation parameters within 20 minutes. Etomidate was used most frequently, and patients receiving it appeared to be the most haemodynamically stable. However, ketamine displayed a similar profile, and was used in patients with lower initial blood pressures. Interestingly, ketamine was not associated with a significant change in heart rate. If patient weight and disease severity had been more accurately documented, a correlation between these parameters and the ideal induction dose could potentially have been described. This should be more closely studied in future versions of this database.[36]
Study limitations
A portion of the dataset (11%) was excluded owing to unavailability of patient records, most of which were for trauma patients. These records could represent a potentially difficult airway scenario due to in-line spinal stabilisation and deranged physiology, so their exclusion could have caused a significant skewing of the data. FPS rates have been shown to be lower in this subset of patients.[12]
The study data came from a single centre so could have been affected by regional practices as well as regional resource issues, e.g. stock availability, time to hospital, and airway management protocols.
Consecutive patient sampling was the goal for the registry, requiring each doctor to complete the registry after managing their patients. Patient logbooks were audited weekly to ascertain a level of compliance with registry completion. However, the sample may nevertheless not have included all patients intubated in the ED.
The registry was completed by the person responsible for managing the patient. While random audits of registry entries were conducted self-reporting bias may still have influenced the data, especially regarding complications.
The registry itself was not initially set up for some of the study outcomes, so extrapolating data, particularly for operator level, was not always possible.
Conclusions
This single-centre retrospective registry review provides insight into current airway practices in our SA ED. The patient population had a wide range of clinical presentations and disease severities, which would challenge the most seasoned ED doctor. The level of intubation success for ED medical officers and registrars, however, was comparable to international developed world standards, while still offering areas for improvement, including the reporting and managing of AEs.
Data from this registry are invaluable in evaluating current practice and identifying areas for improvement. More EDs should consider implementing this form of data capture to assess practice and identify areas for quality improvement purposes.
Declaration. The research for this study was done in partial fulfilment of the requirements for JCH's MMed (Emergency Medicine) degree at the University of the Witwatersrand.
Acknowledgements. None.
Author contributions. LNG conceptualised the study. JCH extracted from the registry. LNG and JCH were involved in the statistical analysis and interpretation of data. JH drafted the initial version of the manuscript. Both authors revised, edited and contributed substantially to the critical revision of the manuscript. Final approval of the version to be published was made by both authors, who agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JH takes responsibility for the article as a whole.
Funding. None.
Conflicts of interest. None.
References
1. Walls RM, Brown CA III, Bair AE,Pallin DJ. Emergency airway management. A multi-center report of 8937 emergency department intubations. J Emerg Med 2011;41(4):347-353. https://doi.org/10.1016/j.jemermed.2010.02.024 [ Links ]
2. Alkhouri H, Vassiliadis J, Murray M, et al. Emergency airway management in Australian and New Zealand emergency departments. A multicentre descriptive study of 3710 emergency intubations. Emerg Med Aus 2017;29(5);499-508. https://doi.org/10.1111/1742-6723.12815 [ Links ]
3. Martin LD, Mhyre JM, Shanks AM, Tremper KT, Kheterpal S. 3423 emergency tracheal intubations at a university hospital. Airway outcomes and complications. Anesthesiology 2011;114(1):42-48. https://doi.org/10.1097/ALN.0b013e318201c415 [ Links ]
4. Sakles JC, Chiu S, Mosier J, et al. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 2013;20(1):71-78. https://doi.org/10.1111/acem.12055 [ Links ]
5. Sakles JC, Laurin EG, Rantapaa A A, Panacek E A. Airway management in the emergency department. A one-year study of 610 tracheal intubations. Ann Emerg Med 1998;31(3):325-332. https://doi.org/10.1016/SO196-0644(98)70342-7 [ Links ]
6. Sagarin MJ, Barton ED, Chung Y, Walls RM. Airway management by US and Canadian emergency medicine residents. A multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med 2005;46(4):328-336. https://doi.org/10.1016/j.annemergmed.2005.01.009 [ Links ]
7. Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015;115(6):827-848. https://doi.org/10.1093/bja/aev371 [ Links ]
8. Cook TM, Woodall N, Frerk C, Fourth National Audit Project. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Br J Anaesth 2011;106(5):617-642. https://doi.org/10.1093/bja/aer058 [ Links ]
9. Menkiti ID, Badmus OO, Adeloka OO, Asiyanbi GK, Desalu I. Tracheal intubation in the emergency department of a sub-Saharan teaching hospital. A one-year survey at Lagos University Teaching Hospital, Nigeria. West Afr J Med 2014;33(3):201-205. [ Links ]
10. Hardcastle TC, Goff T. Trauma unit emergency doctor airway management. S Afr Med J 2007;97(9):864-867. [ Links ]
11. Brown CA III, Sakles JC, Mick NW The emergency airway algorithms. In. Brown CA, Sackles M, eds. Manual of Emergency Airway Management. 5th ed. Philadelphia. Lippincott Wilhams & Wilkins; 2017:25. [ Links ]
12. Park L, Zeng I, Brainard A. Systematic review and meta-analysis of first-pass success rates in emergency department intubation. Creating a benchmark for emergency airway care. Emerg Med Austraias 2017;29(1):40-47. https://doi.org/10.1111/1742-6723.12704 [ Links ]
13. CormackRS,Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984;39(11).1105-1111. https://doi.org/10.111/j.1365-2044.1984.tb08932.x [ Links ]
14. Wongyingsinn M, Songarj P, Assawinvinijkul T. A prospective observational study of tracheal intubation in an emergency department in 2300-bed hospital of a developing country in a one-year period. Emerg Med J 2009;26(8):604-608. https://doi.org/10.1136/emj.2008.061192 [ Links ]
15. Levitan RM, Rosenblatt B, Meiner EM, et al. Alternating day emergency medicine and anesthesia resident responsibility for management of the trauma airway. A study of laryngoscopy performance and intubation success. Ann Emerg Med 2004;43(l):48-53. https://doi.org/10.1016/S0196-0644(03)00638-3 [ Links ]
16. Kerslake D, Oglesby AJ, di Rollo N, et al. Tracheal intubation in an urban emergency department in Scotland. A prospective, observational study of 3738 intubations. Resuscitation 2015;89:20-24. https://doi.org/10.1016/j.resuscitation.2015.01.005 [ Links ]
17. Tam AYB, Lau FL. A prospective study of tracheal intubation in an emergency department in Hong Kong. Eur J Emerg Med 2001;,8(4):305-310. https://doi.org/10.1097/00063110-200112000-00011 [ Links ]
18. Lee JK, Kang H, Choi HJ. Changes in the first-pass success rate with the GlideScope video laryngoscope and direct laryngoscope. A ten-year observational study in two academic emergency departments. Clin Exp Emerg Med 2016;3(4):213-218. https://doi.org/10.15441/ceem.l6.148 [ Links ]
19. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT. Practice guidelines for management of the difficult airway. An updated report by the American Society of Anesthesiologists task force on management of the difficult airway. Anesthesiology 2013;118(2):251-270. https://doi.org/10.1097/ALN.0b013e31827773b2 [ Links ]
20. Lewis SR, Butler AR, Parker J, et al. Video laryngoscopy versus direct laryngoscopy for adults requiring tracheal intubation. Cochrane Database Syst Rev 2016, Issue 11. Art. No.. CD011136. https://doi.org/10.1002/14651858.CD011136.pub2 [ Links ]
21. Pieters BMA, Maas EHA, Knape JTA, van Zundert AAJ. Video laryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways. A systematic review and meta-analysis. Anaesthesia 2017;72(12):1532-1541. https://doi.org/10.1111/anae.l4057 [ Links ]
22. Janz DR, Semler MW, Lentz RJ, et al. Randomized trial of video laryngoscopy for endotracheal intubation of critically ill adults. Crit Care Med 2016;44(11):1980-1987. https://doi.org/10.1097/CCM.0000000000001841 [ Links ]
23. Lascarrou JB, Boisrame-Helms J, Bailly A, et al. Video laryngoscopy vs direct laryngoscopy on successful first-pass orotracheal intubation among ICU patients. A randomized clinical trial JAMA 2017;317(5):483-493. https://doi.org/10.1001/jama.2016.20603 [ Links ]
24. Yeatts DJ, Dutton RP, Hu PF, et al. Effect of video laryngoscopy on trauma patient survival A randomized controlled trial. J Trauma Acute Care Surg 2013;75(2):212-219. https://doi.org/10.1097/TA.0b013e318293103d [ Links ]
25. Cortellazzi P, Caldiroli D, Byrne A, et al. Defining and developing expertise in tracheal intubation using a GlideScope for anaesthetists with expertise in Macintosh direct laryngoscopy. An in-vivo longitudinal study. Anaesthesia 2015;70(3):290-295. https://doi.org/10.1111/anae.l2878 [ Links ]
26. Bacon ER, Phelan MP, Doyle DJ. Tips and troubleshooting for use of the GlideScope video laryngoscope for emergency endotracheal intubation. Am J Emerg Med 2015;33(9):1273-1277. https://doi.org/10.1016/j.ajem.2015.05.003 [ Links ]
27. Sakles JC, Mosier J, Patanwaia AE, Dicken J. Learning curves for direct laryngoscopy and Glidescope1 video laryngoscopy in an emergency medicine residency. West J Emerg Med 2014;15(7):930-937. https://doi.org/10.5811/westjem.2014.9.23691 [ Links ]
28. Sainsbury JE, Telgarsky B, Parotto M, et al. The effect of verbal and video feedback on learning direct laryngoscopy among novice laryngoscopists. A randomized pilot study. Can J Anaesth 2017;64:252-259. https://doi.org/10.1007/sl2630-016-0792-x [ Links ]
29. Hayes-Bradley C, Lewis A, Burns B, Miller M. Efficacy of nasal cannula oxygen as a preoxygenation adjunct in emergency airway management Ann Emerg Med 2016;68(2):174-180. https://doi.org/10.1016/j.annemergmed.2015.11.012 [ Links ]
30. Sakles JC, Mosier JM, Patanwaia AE, et al. First pass success without hypoxemia is increased with the use of apneic oxygenation during rapid sequence intubation in the emergency department. Acad Emerg Med 2016;23(6):703-710. https://doi.org/10.1111/acem.l2931 [ Links ]
31. Driver BE, Prekker ME, Kornas RL, Cales EK, Reardon RF. Flush rate oxygen for emergency airway preoxygenation. Ann Emerg Med 2017;69(1):1-6. https://doi.org/10.1016/j.annemergmed.2016.06.018 [ Links ]
32. Miguel-Montanes R, Hajage D, Messika J, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mi Id-to-moderate hypoxemia. Crit Care Med 2015;43(3):574-583. https://doi.org/10.1097/CCM.0000000000000743 [ Links ]
33. Baillard C, Fosse JP, Sebbane M, et al. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am J Crit Care Med 2006;174(2):171-177. https://doi.org/10.1164/rccm.200509-1507OC [ Links ]
34. Alien TL, Delbridge TR, Stevens MH, Nicholas D. Intubation success rates by air ambulance personnel during 12- versus 24-hour shifts. Does fatigue make a difference. Prehosp Emerg Care 2001;5(4):340-343. https://doi.org/10.1080/10903120190939481 [ Links ]
35. Maltese F, Adda M, Bablon A, et al. Night shift decreases cognitive performance of ICU physicians. Intensive Care Med 2016;42(3):393-400. https://doi.org/10.1007/s00134-015-4115-4 [ Links ]
36. Leeuwenburg T. Airway management of the critically ill patient. Modifications of traditional rapid sequence induction and intubation. Crit Care Horiz 2015;1.1-10. [ Links ]
 Correspondence:
Correspondence:
J C Hart
jeddcraighart@gmail.com
Accepted 16 September 2019














