Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 no.11 Pretoria Nov. 2019
http://dx.doi.org/10.7196/samj.2019.v109i11.14017
RESEARCH
Closed traction reduction of cervical spine facet dislocations: Compelled bylaw
Μ PotgieterI; D Η BadenhorstI; Μ MohideenII; J Η DavisIII
IMB ChB, MMed (Orth), FC Orth (SA); Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University Cape Town, South Africa
IIMB ChB, FC Orth (SA), MMed (Orth)]; Department of Orthopaedic Surgery, University of KwaZulu-Natal, Durban, South Africa
IIIMB ChB, FC Orth (SA), MMed (Orth); Spinal Surgery, Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University Cape Town, South Africa
ABSTRACT
BACKGROUND. Following a 2015 ruling, the South African (SA) Constitutional Court obligates closed reduction of cervical facet dislocations sustained through low-energy injury mechanisms, within 4 hours of injury. Closed traction reduction of cervical facet dislocations requires specific equipment and expertise, which have limited availability in SA.
OBJECTIVES. To review the time delays, delaying factors and success rate of closed reductions of cervical facet dislocations in a tertiary-level orthopaedic department and training facility, and to consider the feasibility of such a reduction within 4 hours after injury.
METHODS. The clinical records and imaging screens of patients presenting with cervical facet dislocations to an academic training hospital between November 2008 and March 2016 were retrospectively reviewed, with specific attention to demographic information, mechanism of injury, time delays from injury to treatment and factors resulting in delay, as well as the success rate in closed cervical reduction.
RESULTS. Ninety-one patients with cervical dislocation presented during the study period, of whom 69 were included for further review. The mean age at presentation was 37.6 (range 18 - 65) years. Successful reduction was achieved in 71% (n=49) of cases, with a median delay time from injury to reduction of 26 (interquartile range (IQR) 19.50 - 31.75) hours. Only 1 patient of 69 patients received successful reduction within 6 hours after injury. Neurological improvement was noticed in 5 of 53 patients with neurological deficit - after successful reduction. Two patients improved with two American Spinal Injury Association (ASIA) grades (from A to C), and 2 improved with one ASIA grade (from A to Β and D to E).
CONCLUSIONS. Successful reduction of a cervical facet dislocation within 4 hours presents a challenge to healthcare infrastructure globally. The relative scarcity of this type of injury (91 cases during 8 years in a tertiary referral hospital) prevents district-level clinicians from readily acquiring a level of experience to confidently perform closed reduction of these injuries, unless very specific training and support are provided towards this end.
The urgency of closed reduction of acute low-velocity cervical facet dislocations has recently been highlighted by the Constitutional Court of South Africa (SA), following a permanent spinal cord injury that a young rugby player sustained during a club-level match. The court found that if emergency care of the complainant had resulted in rapid closed reduction of his cervical spine injury, he might not have suffered permanent neurological damage.[1] The findings of the court were based on research by Newton et al.,[2]who specifically looked at the timing of reduction of low-velocity cervical facet dislocation sustained by rugby players. In their cohort, reduction of facet dislocation within 4 hours after injury was associated with improved neurological outcomes. By performing an early closed reduction of the cervical spine, pressure is relieved from the spinal cord, preventing secondary ischaemic trauma and thus improving the possibility of neurological recovery[3-5] It is important to note that this cohort of patients sustained low-velocity injuries. These may include sports-related injuries, falls from a standing height and blunt object assault. The severity of spinal cord trauma, or the viscous response of spinal cord tissue, is a product of the severity of compression, duration of compression and rate at which compression is applied,[6] which can also be referred to as the velocity of trauma. When compression is applied at a lower velocity, the spinal cord is more likely to show recovery and can withstand higher loads of compression than when subjected to the same compressive load applied at a higher velocity. Animal studies demonstrated this threshold to be 3 m/s, which equates to a fall from a standing height.[7]
The current dispensation in SA demands that injuries of this nature be treated in specialised orthopaedic or neurosurgical units, or by qualified surgeons, with limited, if any, attempts at a closed reduction prior to arrival at a dedicated unit or service. The question of feasibility of mandatory closed reduction of cervical facet dislocations within 4 hours is therefore raised.
This study reviews the time delays, delaying factors and success rate of closed reductions of cervical facet dislocations in an orthopaedic department at a tertiary-level training hospital over a period of 8 years.
Methods
A retrospective review of case notes and imaging screens of patients >18 years of age with cervical facet-joint dislocations presenting to a tertiary-level academic hospital in Western Cape Province of SA was performed. The university-affiliated hospital has a capacity of 1 899 beds and provides advanced trauma and orthopaedic treatment to a population of -3.6 million, and is one of the largest facilities providing spinal surgery and treatment for adult polytrauma patients in the province. A significant proportion of patients are referred from surrounding rural areas, with minimal transport infrastructure, and delayed transport by road very often being the only option. The primary objective of this study was to establish a time line of events from the moment the injury happened until active closed cervical spine reduction was performed.
All of the enrolled patients presented to our institution between January 2008 and March 2016 with acute uni- or bifacet dislocations. Our unit routinely treats such injuries with an active closed reduction: therefore, this study excluded any patients in whom an active closed reduction was not performed, regardless of the reason. No distinction was made between the presence or absence of facet fractures. Considering that a closed reduction for facet dislocations is performed with the exact same technique, irrespective of the involved levels of energy in the causative mechanism, dislocations sustained through both high- and low-energy injury mechanisms were included in this feasibility evaluation.
Closed reduction is typically performed using flexion traction through sequentially increased weights applied via Cones calipers fixed to the skull with rope over a bed- or stand-mounted pulley system. Progression to an extension position follows successful reduction of the dislocated facets. Once reduced, the weight load is lowered to a maintenance weight to retain reduction (Figs 1 and 2). The reduction is performed under radiographic surveillance. Perfect spinal alignment on a final lateral radiograph following release of traction is deemed a successful reduction.
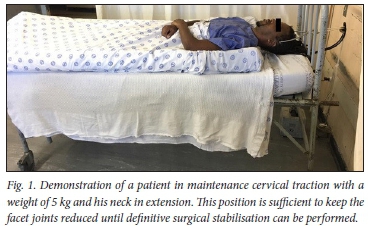

In this series, the reduction process described was used and performed in patients who were awake and co-operative, and who were able to perform motor functions on command and verbalise any alteration of their sensation to allow surveying of changes in neurological condition. Procedural monitoring included noninvasive blood pressure monitoring, pulse oximetry and serial neurological assessments. Small doses of intravenous morphine and intermediate-working diazepam were titrated to response to provide analgesia during the procedure. Patients were kept in skull traction with a maintenance weight until definitive surgical stabilisation could be performed, allowing for safe, out-of-bed mobilisation.
Patient records were reviewed for basic demographic data, mechanism of injury and severity of neurological injury. A time line of events was established by combining recorded time of injury emergency medical service response records and radiology time stamps. The timeline was used to determine:
• delay from the moment injury occurred to admission to our emergency room
• referral from the emergency room to the orthopaedic surgeon on call
• initiation of cervical spine reduction
• time spent performing the reduction
• overall time from injury to reduction.
Radiographs were used to describe the type and level of injury Pre- and post-reduction neurological assessment were recorded as reported in the clinical notes, and stratified using the American Spinal Injury Association (ASIA) score.
Statistical analysis
Statistical analysis was performed using Statistica software version 13.0 (StatSoft Inc, USA).
Data were tested for normality using the Shapiro-Wilk test and expressed as means and standard deviations when normally distributed and as medians with interquartile ranges (IQRs) when not normally distributed
Ethical approval
This study was approved by the Human Research Ethics Committee of Stellenbosch University (ref. no. N15/10/116) and institutional permission was obtained. The study was conducted according to the internationally accepted ethical standards and guidelines of the Declaration of Helsinki, the South African Guidelines for Good Clinical Practice and the Medical Research Council (MRC) Ethical Guidelines for Research.
Results
Records of 91 patients presenting to our institution with cervical facet dislocations between November 2008 and March 2016 were reviewed. Twenty-two patients were excluded because closed reduction was not performed; 69 patients were included in the final analysis.
Clinical and demographic characteristics
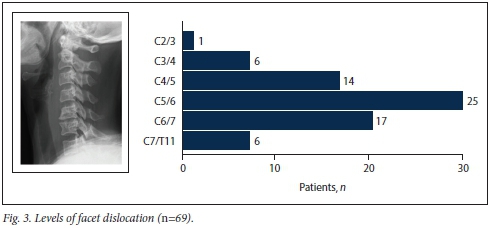
This series included 58 (84%) male patients and 11 (16%) female patients (mean age 37.6 (range 18 - 65) years). The most common cause of injury was motor vehicle accidents (n=46; 67%), followed by a fall from a height (n=14; 20%) and low-energy injuries (e.g. same-level fall, sports injuries or interpersonal violence) (n=9; 13%). Thirty-eight (55%) patients had unifacet dislocations and 31 (45%) bifacet dislocations. The most common injury was at the C5/6 intervertebral disc level, followed by the C6/7 and C4/5 levels (Fig. 3).
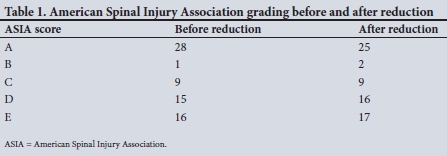
Neurological assessment at time of presentation demonstrated that 28 (41%) patients suffered a complete spinal cord injury recorded as ASIA A. Of the remaining patients, 16 (23%) had no spinal cord injury (ASIA E) and 25 (35%) had incomplete spinal cord injury (ASIA B, C, D).
Time to reduction
The median time between evacuation from the scene of injury and arrival at the emergency department was 3 (IQR 2-3) hours, with a median in-hospital delay from emergency admission to review by an orthopaedic surgeon of 9 (IQR 4.75 - 14.5) hours. The median time delay from first orthopaedic consult to starting the reduction attempt was a further 10 (IQR 6-15) hours. The various components of delay prior to initiating closed reduction are shown in Fig 4. There was a greater delay in in-hospital referral of patients with complete neurological injury, with a median delay of 9 (IQR 5.5 - 14.75) hours, than in cases of no recorded deficit (ASIA E), with a median delay of 5.5 (IQR 2-11) hours. However, this difference was not statistically significant (p=0.118).
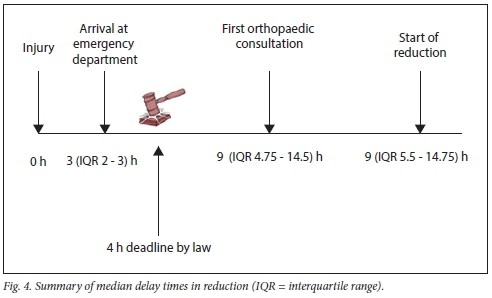
The median time from injury to reduction was 26 (IQR 19.5 - 31.75) hours. In only 1 case of 69 cases was there successful reduction within 6 hours after injury. Reduction in all other recorded cases was >12 hours after time of injury.
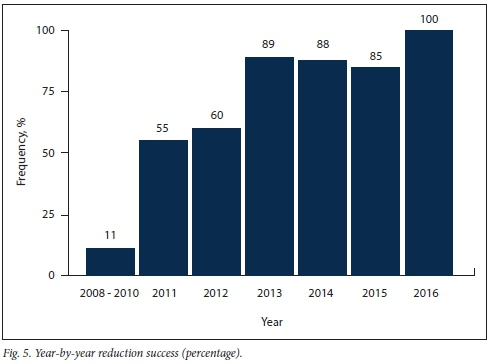
Reduction outcomes
Successful reduction was achieved in 71% (n=49/69) of cases. Improvement in success rate was seen year on year, from 50% in 2013 to 100% in 2016 (Fig. 5). A significant difference (p=0.024) was demonstrated in the reduction success between unifacet dislocations (58%; n=18/31) and bifacet dislocations (81%; n=31/38). The median time of the reduction process was 51 (IQR 34 -82) minutes in successful cases, and 60 (IQR 45 - 89) minutes in unsuccessful cases.
Neurological deficit improvement was noticed in 5 patients after successful reduction. Two patients improved with two ASIA grades (from A to C), and 2 improved with one ASIA grade (from A to Β and D to E) (Table 1).
Discussion
The recent literature provides a strong argument for the reduction of low-velocity cervical facet dislocations within 4 hours.[2] The authors noted that in low-velocity cervical spine facet dislocation early reduction within 4 hours plays a more important role in neurological recovery than the initial neurological presentation. The international multicentre Surgical Timing in Acute Spinal Cord Injury Study (STASCIS), however, recommends reduction within 24 hours -the point after which neurological recovery is highly unlikely[8] Several other human[3,4,912] and animal studies[13-15] similarly found that decompression in <12 hours is associated with better outcomes, and that delay of >24 hours may result in permanent neurological damage. The difference between 4 and 24 hours is significant, considering the practicality of performing a reduction, closed or open, within the limits of healthcare resources available in SA. This study examines the feasibility of achieving early reduction of any cervical facet dislocation regardless of mechanism of injury. Therefore, this discussion refers mostly to time delays to successful reduction.
The demographic distribution of our study population echoes that of previous investigators,[4,16,18] identifying that young male patients are most commonly injured. This includes their participation in contact sports, i.e. rugby, high-risk occupations, high-risk behaviour patterns and alcohol abuse, more frequently seen in young men. The majority of this study group was involved in road traffic accidents (66%) and there were 9 (11%) sports-related injuries. This was in keeping with the findings of Lee et al.[4]who reported 58% road traffic injuries and 5.7% sports-related injuries. Eranki et al.[16]reported 65% road traffic accidents and Anderson et αl.[17]48% motor vehicle accidents and 13.3% sports-related injuries.
In this study, the median delay from injury to reduction was 26 hours (IQR 19 h 30 min - 31 h 45 min), already falling beyond the STASCIS[19] recommendations. A previous SA study of 1981 - 1993 by Lee et al.[4] reported average delays in reduction of between 58 and 78 hours. A more recent study from Australia by Eranki et al[16] reported facet enlocation within 10.5 hours for urban patients and 27 hours for patients living in rural areas, highlighting the impact of available resources on the speed of reduction. Lins et al.[20]from Brazil discuss the outcome after surgical reduction of cervical facet dislocation. They were successful in achieving reduction within 24 hours in 58% of cases. The STASCIS trial also reported successful reduction and decompression within 24 hours in 58% of their patients.[8] In the study of cervical spine injuries in rugby players, Newton et α/.[2] reported successful reduction of facet dislocation in a median of 9 (1 - 720; IQR 4 - 27) hours after injury. Important to note is that they achieved reduction within 24 hours in 78% of cases and within 4 hours in 24.7% of cases after injury. These patients had isolated cervical spine injuries sustained during a rugby match. This fact could have influenced their treatment pathway compared with high-velocity poly-traumatised patients. Faster response times to the scene, with emergency medical services being present at rugby matches, awareness by healthcare professionals of this injury type, rapid referral pathways and dedicated management teams to treat rugby injuries make this a very unique subgroup when used for comparison.
There are numerous delay points in the process of successfully reducing a facet dislocation. Various factors contribute to the delays between each point. Some of these factors may be obvious and others more obscure, and they are also not routinely or accurately documented in patient records. This makes it difficult to study the impact of each factor on the group as a whole. It is clear, however, that the management pathway of rugby injuries in SA differs from that of other more common injury mechanisms.
In this study, the median time delay from injury to hospital was 3 (IQR 2-6) hours. Factors influencing the prehospital delays included: distance from hospital, i.e. rural or urban; level of available emergency medical and ambulance services; current load on healthcare resources at the given point in time; severity of other injuries; and nature of the injury pattern. There may also be a delay in interhospital referrals owing to health resource availability, such as ambulance services or after-hours radiography services. In our study this was the shortest period of delay in the management pathway, which brings credit to the emergency medical services. Eranki et al[16]similarly found that the geographical location of the patient at the time of injury and availability of resources are major contributory factors influencing time delays in facet enlocation.
In-hospital delays can occur within two steps of the management pathway. The first delay point is in the emergency room. In this study, the median delay from hospital admission to referral for an orthopaedic review was 9 hours (IQR 4 h 45 min - 14 h 30 min). Delays in recognising or failing to recognise the injury and obtaining an early orthopaedic consultation may be influenced by the severity of the patient's other injuries, awareness of cervical spine injury (referred to as C spine injury v. new diagnosis), waiting for further imaging (computed tomography (CT)/magnetic resonance imaging (MRI)), management of immediate life-threatening injuries and severity of neurological injury.
The second delay point is the time to initiating the reduction process by the orthopaedic surgeon on call. The median time from the first orthopaedic consultation until initiation of a reduction attempt was 10 (IQR 6 - 15) hours. These delays may include one or several of the following: waiting for further imaging (CT/MRI); availability of Cones calipers and equipment to perform the reduction, including availability of a bed on which to perform the reduction (in some cases), and associated head injuries that may prevent urgent closed reduction; and other life-threatening injuries requiring stabilisation. Until recently, there was a lack in consensus with regard to MRI before attempting closed reduction due to the risk of disk herniation into the canal during the reduction process.[21-23] In 2013, the Society of Neurological Surgeons guideline[24] recommended MRI only if closed reduction fails and for unconscious patients. In a patient with sufficient cognition, obtaining an MRI prior to closed reduction delays decompression and promotes secondary cord injury. An MRI should be performed after facet enlocation, before definitive surgical stabilisation, as this aids in decisionmaking regarding the surgical approach. Since 2015, our unit has adopted a practice of early reduction followed by MRI, resulting in a noticeable decline in in-hospital delays.
Conclusions
Successful reduction of a cervical facet dislocation within 4 hours presents a challenging problem to healthcare infrastructure globally. The relative scarcity of this injury (91 cases during 8 years in a tertiary referral hospital) prevents district-level clinicians from readily acquiring the level of experience to confidently perform closed reduction of these injuries, unless very specific training and support are provided towards this end. The reported body of literature supports feasibility within 24 hours, as recommended by STASCIS. The benefit of a reduction within 4 hours of a low-energy injury is well supported and undeniable in biophysiological models and is therefore a goal that should certainly be strived for. The reality of successfully achieving this within a resource-limited environment remains debatable. To achieve this, we need to increase awareness among all role players in the treatment pathway and there should be sufficient resources to perform the reduction.
Recommendations
We recommend training and increased awareness of all staff working in emergency medical services on the management pathway of patients with cervical spine injuries. The goal of treatment should be to achieve closed reduction as rapidly as possible, ideally within 4 hours and no later than 24 hours after injury. In most instances, this can be performed more rapidly than moving the patient to an operating theatre for open surgical reduction. Specific training should be provided to emergency unit staff (preferably within specified central units located within referral hubs) in the application of calipers and the process of closed reduction of cervical facet dislocation. Referring hospitals should liaise directly with the treating surgeon at the appropriate referral hospital, which should be communicated to the emergency department at the relevant hospital. These patients need urgent attention on arrival and should be evaluated immediately by the casualty officer and stabilised according to the advanced trauma life-support guidelines. The minimum imaging necessary is a good-quality lateral shoot-through radiograph, including CI and the superior endplate of Tl.[24] We recommend early contact with the orthopaedic surgeon with regard to further imaging. A CT scan should not delay the reduction process if adequate radiographs reveal sufficient information. The primary aim of treatment is to prevent secondary injury to the spinal cord.[5] Oxygen should be administered to maintain saturation at 100% and circulatory support should target a mean arterial pressure of >75 mmHg. In-line stabilisation is paramount and applying Cones calipers is a safe and easy procedure to aid with this.[25] In-line traction can be maintained with 5 kg weight for adult patients.[22] This is also the first step in the reduction process and helps to relax the spasticity in the paravertebral muscles and to diminish pressure on the spinal cord and nerve roots. The patient can be safely transferred, in traction, to a referral hospital, if needed.[26] We therefore recommend all referral hospitals to have equipment and expertise to apply in-line skull traction with Cones calipers. MRI prior to closed reduction is not indicated, unless the patient is unable to communicate neurological changes during the reduction process.[27] Neurological examination should be performed before and after any intervention and must be clearly documented. Rapid neurological decline may be due to ongoing compression or significant instability and may necessitate urgent open reduction. All the required equipment to perform a closed reduction should be readily available and preferably in a single place. This includes various weights, calipers in different sizes, string to attach weights to calipers, a pulley system, a bed and two mattresses. Purpose-built closed reduction systems might, in future, offer value in limiting time and improving efficiency of the reduction process.
The most important part for all key personnel in the treatment pathway is to stay cognisant of the urgency of early reduction in all patients with low-energy cervical spine facet dislocations. It is currently accepted that reduction within 24 hours after injury may improve the neurological condition with up to two functional levels. The best outcomes can be expected in patients treated within 4 hours after injury and is a goal that should be aimed for.[2]
Declaration. None.
Acknowledgements. Division of Orthopaedic Surgery Tygerberg Hospital and Stellenbosch University for research support.
Author contributions. Proposal: DHB, MM; data capture and analysis: MP, DHB, MM; manuscript preparation: JHD, MP; senior author and supervisor: JHD; principal author: MP.
Funding. Tygerberg Hospital Orthopaedic research fund.
Conflicts of interest. None.
References
1. Oppelt vHead. Health, Department of Health Provincial Administration. Western Cape (CCT185/14) (2015) ZACC 33,2016(1) SA 325 (CC), 2015 (12) BCLR1471 (CC) (14 October 2015). [ Links ]
2. Newton D, England M, Doll H, Gardner BP. The case for early treatment of dislocations of the cervical spine with cord involvement sustained playing rugby. Bone Joint J 2011,93B(12).1646-1652. https://doi.org/10.1302/0301-620X.93B12.27048 [ Links ]
3. Furlan JC, Noonan V, Cadotte DW, Fehlings MG. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury. An evidence-based examination of pre-clinical and clinical studies. J Neurotrauma 2011,28(8).1371-1399. https://doi.org/10.1089/neu.2009.1147 [ Links ]
4. Lee AS, Maclean JCB, Newton DA. Rapid traction for reduction of cervical spine dislocations. J Bone Joint Surg 1994,76(3):352-356. [ Links ]
5. Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991,75(1)15-26. https://doi.org/10.3171/jns.l991.75.1.0015 [ Links ]
6. Kearney PA, Ridella SA, Viano DC, Anderson TE. Interaction of contact velocity and cord compression in determining the severity of spinal cord injury J Neurotrauma 2009,5(3).187-208. https://doi.org/10.1089/neu.l988.5.187 [ Links ]
7. Lau IV, Viano DC. The viscous criterion - bases and applications of an injury severity index for soft tissues. SAE Tech Paper 2010,1. https://doi.org/10.4271/861882 [ Links ]
8. Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury. Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLOS ONE 2012;7(2)re32037. https://doi.org/10.1371/journal.pone.0032037 [ Links ]
9. Lee D, Park Y, Song S, Hwang S. The importance of early surgical decompression for acute traumatic spinal cord injury Clin Orthop Surg 2018,10(4)7448-454. https://doi.org/10.4055/cios.2018.10.4.448 [ Links ]
10. Koivikko MP, Myllynen P, Santavirta S. Fracture dislocations of the cervical spine. A review of 106 conservatively and operatively treated patients. Eur Spine J 2004,13(7).610-616. https://doi.org/10.1007/S00586-004-0688-2 [ Links ]
11. Burke JF, Yue JK, Ngwenya LB, et al. Ultra-early (>12 hours) surgery correlates with higher rate of American Spinal Injury Association impairment scale conversion after cervical spinal cord injury. Neurosurgery 2019,85(2).199-203. https://doi.org/10.1093/neuros/nyy537 [ Links ]
12. Li Y, Walker CL, Zhang YP, Shields CB, Xu X-M. Surgical decompression in acute spinal cord injury. A review of clinical evidence, animal model studies, and potential future directions of investigation. Front Biol (Beijing) 2014,9(2).127-136. https://doi.org/10.1007/sll515-014-1297-z [ Links ]
13. Delamarter RB, Sherman J, Carr JB. Pathophysiology of spinal cord injury. Recovery after immediate and delayed decompression. J Bone Joint Surg Am 1995,77(7).1042-1049. https://doi.org/10.2106/00004623-199507000-00010 [ Links ]
14. Jazayeri SB, Firouzi M, Zadegan ZA, et al The effect of timing of decompression on neurologic recovery and histopathologic findings after spinal cord compression in a rat model Acta Med Iran 2013,51(7).431-437. [ Links ]
15. Netto C de C, Gaia PLF, Sattin AA, Cristante AF, Marcon RM. Effects of decompression time after spinal injury on neurologic recovery in Wistar rats. Acta Ortop Bras 2010,18(6).315-320. https://doi.org/10.1590/S1413-78522010000600002 [ Links ]
16. Eranki V, Koul K, Mendz G, Dillon D. Traumatic facet joint dislocation in Western Australia. Eur Spine J 2016,25(4).1109-1116. https://doi.org/10.1007/s00586-014-3627-x [ Links ]
17. Anderson GD, Voets C, Ropiak R et al. Analysis of patient variables affecting neurologic outcome after traumatic cervical facet dislocation. Spine J 2004,4(5).506-512. https://doi.org/10.1016/j.spinee.2004.03.001 [ Links ]
18. Sothmann J, Stander J, Kruger N, Dunn R. Epidemiology of acute spinal cord injuries in the Groote Schuur hospital acute spinal cord injury (GSH ASCI) unit, Cape Town, South Africa, over the past 11 years. S Afr Med J 2015;105(10).835-839. https://doi.org/10.7196/SAMJnew.8072 [ Links ]
19. Yousefrfard M, Rahimi-Movaghar V, Baikpour M, et al. Early versus late decompression for traumatic spinal cord injuries. A systematic review and meta-analysis. Emergency 2017,5(1).12. https://doi.org/10.1007/sll999-010-1606-z [ Links ]
20. Lins CC, Prado DT, Joaquim AF. Surgical treatment of traumatic cervical facet dislocation. Anterior posterior or combined approaches? Arquivos de Neuro-Psiquiatria 2016,74(9).745-749. https://doi.org/10.1590/0004-282X20160078 [ Links ]
21. Grauer JN, Vaccaro AR, Lee JY, et al. The timing and influence of MRI on the management of patients with cervical facet dislocations remains highly variable. J Spinal Disord Tech 2009,22(2).96-99. https://doi.org/10.1097/BSD.0b013e31816a9ebd [ Links ]
22. Gelb DE, Hadley MN, Theodore N. Initial closed reduction of cervical spinal fracture-dislocation injuries. Neurosurgery 2013,72(3).73-83. https://doi.org/10.1227/NEU.0b013e318276ee02 [ Links ]
23. Fleming DM, Westgarth-Taylor DT, Dunn PR How does pre-reduction MRI affect surges behaviour when reducing distraction-flexion (dislocation) injuries of the cervical spine? S Afr Orthop J 2015,14(4)τ42-46. https://doi.org/10.17159/2309-8309/2015/vl4n4a5 [ Links ]
24. Ryken TC, Hadley MN, Walters BC, et al. Radiographic assessment. Neurosurgery 2013,72(Suppl 2(3)).54-72. https://doi.org/10.1227/NEU.0b013e318276edee [ Links ]
25. Ryken TC, Huribert RJ, Hadley MN, et al. The acute cardiopulmonary management of patients with cervical spinal cord injuries. Neurosurgery 2013,72(Suppl 2(3)).84-92. https://doi.org/10.1227/NEU.0b013e318276eel6 [ Links ]
26. Theodore N, Aarabi B, Dhall SS, et al. Transportation of patients with acute traumatic cervical spine injuries. Neurosurgery 2013,72(Suppl 2(3)).35-39. https://doi.org/10.1227/NEU.0b013e318276edc5 [ Links ]
27. Kanwar R Delasobera BE, Hudson K, Frohna W Emergency department evaluation and treatment of cervical spine injuries. Emerg Med Clin Ν Am 2015,33(2).241-282. https://doi.org/10.1016/j.emc2014.12.002 [ Links ]
 Correspondence:
Correspondence:
J Η Davis
johanhdavis@gmail.com
Accepted 26 April 2019














