Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 no.11 Pretoria Nov. 2019
http://dx.doi.org/10.7196/samj.2019.v109i11.14442
CME
GUEST EDITORIAL
Rudolf Ludwig Carl Virchow (13 October 1821 - 5 September 1902) was a German physician, anthropologist, pathologist, prehistorian, biologist, writer, editor and politician who is widely regarded as the the 'father of modern pathology' and was affectionately called the 'Pope of medicine' by his friends. His investigation of the 1847 -1848 typhus epidemic laid the foundation for the establishment of public health as a discipline in Germany, and paved his political and social careers. He famously coined the aphorism: 'Medicine is a social science, and politics is nothing else but medicine on a large scale.'
Virchow was the first to describe and christen conditions such as thrombosis, embolism, leukaemia, chordoma and ochronosis. He was also the first to correctly describe the mechanisms of the development of cancers. He coined many biological and medical terms in everyday use, including chromatin, neuroglia, agenesis, parenchyma, osteoid, amyloid degeneration and spina bifida. There are many terms, such as Virchow's triad, Virchow's node, Virchow-Seckel syndrome and Virchow-Robin spaces, which are named after him. He developed the first systematic method of autopsy and introduced hair analysis in pathological and forensic investigation. His description of the life cycle of the roundworm, Trichinella spiralis, established the practice of meat inspection.
Virchow's triad describes the three broad categories of factors that are thought to contribute to thrombosis: hypercoagulability, haemodynamic changes and endothelial injury. Interestingly, the elements comprising Virchow's triad were neither proposed by Virchow, nor did he ever suggest a triad to describe the pathogenesis of venous thrombosis. In fact, it was decades following his death before consensus was reached proposing that thrombosis is the result of alterations in blood flow, vascular endothelial injury or alterations in the constitution of the blood. However, our current understanding of the pathophysiology of thrombosis is similar to his proposed description of the mechanism of embolism, published in 1856.[1]
Pregnancy and the puerperium are well-established risk factors for venous thromboembolism (VTE). The overlap with symptoms of pregnancy may impair clinical suspicion, making the diagnosis of VTE more challenging. VTE can manifest during pregnancy as an isolated lower-extremity deep-vein thrombosis (DVT), or a clot can break off from the lower extremities and travel to the lung to present as a pulmonary embolus (PE), the 7th leading cause of maternal mortality and responsible for 9% of maternal deaths.[2] The detection of DVT during pregnancy is critical to prevent deaths from PE. Pregnancy-related mortality has the largest racial disparity among the maternal and child health indicators: black women have a 3 - 4 times higher pregnancy-related mortality ratio than white women. Although the reasons for this cannot be directly attributed to increased rates of VTE, the number of deaths from this condition are higher in black than in white women.[2]
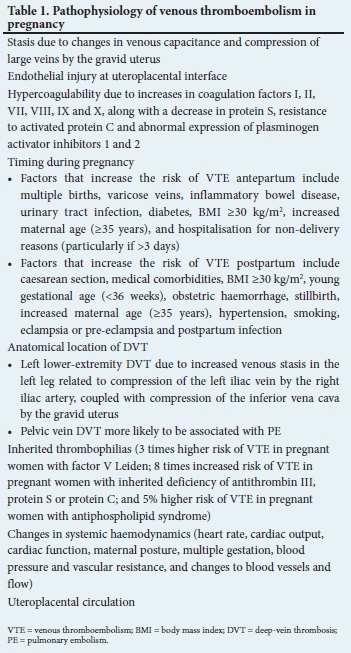
A risk model for VTE within the first 6 weeks postpartum has been developed and externally validated, based upon two large European cohorts.[3] Among the many factors that contribute to the model, those associated with the highest risk were emergency caesarean section, stillbirth, varicose veins, pre-eclampsia/eclampsia, postpartum infection and comorbidities. Further validation is needed to confirm these results. The mechanisms leading to VTE in pregnancy are included in Table 1.
In this issue of CME, there are two articles. The first article by Wessels[4] on pregnancy-associated VTE reviews the epidemiology, risk factors, pathophysiology, approach to initial assessment, diagnosis and management of VTE. The guidance is appropriate for local practice, and situations where specific hypercoagulation problems manifest, are reviewed. Further, the appropriate management of labour and neuraxial anaesthesia is also discussed. The author concludes that, although managing VTE in the pregnant patient is complex, a team approach taking all factors in the individual patient into consideration is essential.
The second article, by Menard et al.,[5] reviews transfusion thresholds in clinical practice. It provides a practical and evidence-informed approach to the transfusion of red blood cells and platelets in commonly encountered clinical settings. While transfusion improves oxygen delivery in patients with anaemia, injudicious use of red blood cells may be associated with complications, including infection, allergic and immune reactions, volume overload, hyperkalaemia and iron overload. Even though numerous studies have shown an association between anaemia and increased mortality, it is not clear whether aggressive correction of anaemia improves mortality. The appropriate and evidence-based use of red blood cell and platelet transfusions is reviewed. The authors conclude that, while transfusion of blood products is one of the most routinely administered interventions in healthcare, blood products are a limited resource and transfusion practices need to be carefully scrutinised. The authors remind us that a one-size-fits-all approach in clinical practice has appropriately fallen by the wayside.
It is our hope that the readers of CME will find these articles to be of utility in enhancing their clinical practice.

Vernon J Louw
Division of Clinical Haematology, Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa

Ntobeko A B Ntusi
Division of Cardiology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital; Cape Universities Body Imaging Centre, Faculty of Health Sciences, University of Cape Town; and Hatter Institute for Cardiovascular Research in Africa, Department of Medicine, Faculty of Health Sciences, University of Cape Town, South Africa. ntobeko.ntusi@uct.ac.za
References
1. Virchow RLK. Gesammelte Abhandlungen zur wissenschaftlichen Medicin. Frankfurt am Main: Von Meidinger & Sohn, 1856. [ Links ]
2. Chang J, Elam-Evans LD, Berg CJ, et al. Pregnancy-related mortality surveillance - United States, 1991 - 1999. MMWR Surveill Summ 2003;52(2):1-8. [ Links ]
3. Sultan AA, West J, Grainge MJ, et al. Development and validation of risk prediction model for venous thromboembolism in postpartum women: Multinational cohort study. BMJ 2016;355:i6253. https://doi.org/10.1136/bmj.i6253 [ Links ]
4. Wessels PF. Venous thromboembolism in pregnancy. S Afr Med J 2019;109(11):824-832. https://doi.org/10.7196/SAMJ.2019.v109i11.14365 [ Links ]
5. Menard CE, Seftel M, Ponnampalam A, Zarychanski R. When to transfuse? Red blood cell and platelet transfusion thresholds in clinical practice. S Afr Med J 2019;109(11):833-837. https://doi.org/10.7196/SAMJ.2019.v109i11.14317 [ Links ]














