Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 no.10 Pretoria Out. 2019
http://dx.doi.org/10.7196/samj.2019.v109i10.13951
RESEARCH
Medicolegal perspectives of interpersonal violence: A review of first-contact clinical notes
D P Loots
BSc, MB ChB, Dip PEC (SA), Dip For Med (SA) Path, FC For Path (SA); G Saayman, MB ChB, MMed (Med Forens), FC For Path (SA) Department ofForensic Medicine, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
BACKGROUND. South Africa has one of the highest rates of interpersonal violence (IPV), in all its forms, in the world. Incidents of assault are largely under-reported and place an immense burden on the healthcare, fiscal and judicial systems. The first contact a victim of IPV has with a medical practitioner may be the only opportunity to identify, record and preserve valuable evidence, as evidence not captured on this occasion may be lost forever. The accuracy and quality of clinical notes taken at the time may be of paramount importance in facilitating the administration of justice.
OBJECTIVES. (i) To investigate the adequacy of medicolegal note keeping by doctors in cases where subsequent legal proceedings may ensue; and (ii) to apprise clinicians of their shared responsibility in contributing to the administration of justice through both appropriate patient management and objective and contemporaneous recording of findings from a medicolegal perspective.
METHODS. A prospective descriptive study was conducted over a period of 18 months from 2016 to 2018. The investigators reviewed patient files and critically appraised first-contact clinical notes in fatal-outcome cases of IPV admitted to the Pretoria Medico-Legal Laboratory during the study period. The cases were reviewed using rubrics specifically designed by the investigators to critically but consistently assess the adequacy of documentation of the medicolegal aspects applicable to each case.
RESULTS. One hundred cases met the defined criteria for inclusion in the study. The victims were predominantly male (98%), and most (79%) were aged <40 years. Blunt-force injuries were the most frequent type of injury (43%), while gunshot wounds accounted for 36% of cases and sharp-force injuries were documented in 11%. Insufficient medicolegal documentation, wound description and evidence collection, by medical practitioners, was identified across all wounding modalities in the study sample.
CONCLUSIONS. This study showed that medicolegal documentation in cases of IPV is suboptimal, with many important parameters not being routinely recorded, which is likely to impact negatively on criminal investigations and downstream legal proceedings. Greater emphasis on these issues is required during the undergraduate training of healthcare workers in a society as severely afflicted by IPV as SA. Although this study focused on fatal-outcome cases, these conclusions are equally applicable to many more cases where investigators, prosecutors and presiding judicial officers may be dependent on findings contemporaneously and objectively recorded by medical professionals.
Interpersonal violence (IPV) is a serious epidemic in South Africa (SA). SA has one of the highest rates of IPV, in all its forms, in the world and a low rate of conviction of perpetrators of violence compared with other countries.[1-3] The World Health Organization (WHO) has adapted its framework definition for IPV as violence between individuals, with further subdivision into family and community violence.[2-4] In 2016, Statistics South Africa reported 456 612 deaths in SA[5] Approximately 11% (n=51 242) of these deaths were reported as being due to external causes of morbidity and mortality (non-natural deaths). The second most common cause of non-natural deaths across all age groups was related to assault.^] In the South African Police Service (SAPS) crime statistics report for the years 2017/18, of the 1 662 815 crimes that were reported to the SAPS, 601 366 (36.1%) were contact crimes, of which an estimated 19 016 were murders (homicides).[6] These figures may not represent the full picture, as cases of IPV are often under-reported.[7,8] This epidemic of violence greatly burdens fiscal and human resources in healthcare and judicial domains in SA.[4,9,10]
Previously, medical practitioners were formally appointed in all magisterial regions to the position of 'district surgeon' with dedicated medicolegal duties including the clinical assessment and treatment of victims of IPV. In most cases, these doctors developed great experience and expertise in the field of especially clinical forensic medicine, having also to appear regularly in courts of law. The official position of district surgeon has unfortunately been abolished, the expectation now being that clinical forensic medical services will be provided by state-employed medical practitioners, generally attached to emergency medical departments of hospitals.[11] An estimated 50% of all trauma cases treated at hospitals in SA are due to IPV. [9,10] The WHO reports that for every incident of IPV with a fatal outcome, an estimated further 20 - 40 victims sustain injuries, seek medical treatment and survive [2,12] It is in these cases (which greatly outnumber the fatal-outcome cases) that the attending medical practitioner may well be called upon to testify in court, or where the court may subsequently rely heavily on contemporaneously recorded notes of injuries and other potentially valuable evidentiary information (such as states of intoxication, etc.). The quality of investigative work by police officers has been questioned (whether this is because of workload or other inefficiencies), perhaps adding to the expectation that the records and reports generated by medical professionals will specifically be relied upon to add value in this setting. !7,8]
Victims of IPV may suffer serious injuries, and the primary responsibility of the medical practitioner is of course to attend to patient needs in this regard.[,13] However, in many cases the medical needs of the patient may be of a relatively minor nature, and the primary need for medical attention may then involve proper recording of injuries and gathering of appropriate evidence for further investigative and legal purposes. The emergency medicine practitioner is often the first contact the victim of IPV will have with the health system, making it imperative that appropriate record be made of inter alia the primary and unmodified nature of the injuries, before their appearance may be altered by cleaning or suturing. Even in patients who subsequently die and are referred for forensic medical investigation and autopsy, intervening changes of healing and/or wound complications may make it impossible for a forensic pathologist to differentiate, for example, between entrance and exit gunshot wounds (GSWs), or to accurately record or comment on the primary nature of contusions, abrasions, lacerations, etc. The emergency medical practitioner may therefore be deemed to be the custodian of potentially valuable information from a legal perspective, and should discharge this responsibility meticulously and professionally.[14]
Medical records serve primarily to support patient care by providing a chronological account of the patient's condition and how it develops, and by communicating important information to other healthcare workers. In addition, such records serve to provide data for research, clinical audit and performance monitoring.1151 However, the value and use of medical records for legal purposes (both in criminal proceedings and civil actions) has become a matter of major importance for medical practitioners and other healthcare workers - perhaps nowhere more than in the emergency medical care setting.[14] Contemporaneous clinical notes should provide an objective and accurate record and form a legally binding documented historical record of events.t15,16] Emphasis has been placed on the use of specific, standardised terminology to accurately describe different types of wounds and wound features, to ensure consensus regarding the primary nature or causative mechanisms associated with such woundsJ1,17-211Size, shape, depth, and specific features such as wound margins, foreign material, tissue bridges and associated injuries should be carefully considered and appropriately described.1171 Especially in cases of IPV, proper documentation and reliable record keeping are therefore vital, from both the patient care and legal perspectives.[16,18]
In many countries, template forms have been developed to guide doctors in documenting findings in cases of IPV and sexual assault[22]In SA, doctors are routinely expected to complete the J88 form in cases with medicolegal significance.11,23,241 In many instances, however, the J88 form is not readily available in the emergency room or clinic and will only be completed by the clinician (or indeed a different doctor) at a later stage, once a case has been opened with the SAPS.[23,251 The doctor completing the form may therefore need to rely on the contents of the (initial) clinical notes to compile a medicolegal report and/or complete the J88 form[1,23,24]It is important to appreciate that over and above the J88, other contemporaneous clinical records may be of equal (if not greater) value at subsequent legal inquiry and may of course be subpoenaed.[23]
The National Health Act No. 61 of 2003t261 and the Health Professions Act No. 56 of 1974t[27] are prescriptive in respect of health records. In cases where legal inquiry may follow, accurate and comprehensive completion of the J88 is of paramount importance. Records should be kept of the circumstances of consultation, including, for example, whether the patient was brought in or accompanied by the SAPS and/or whether a form SAP308(a) was produced. Clinical records must be legibly compiled and must be dated and signed by the practitioner[1,23,24] The clinical history and appropriate and relevant demographic, anthropometric and medical information must be noted and injuries should be meticulously examined and clearly and accurately documented, using technically accurate terminology. Sketch annexures and photographs may add great value in this regard[1,23,24]Documentation of the nature/ condition of clothing should be made, with reference (for example) to whether the clothing is blood/fluid stained or torn and/or whether the clothing has been changed.[1,23,24] It may be very important to make a note of the psychological condition of the patient and to record relevant positive and negative findings in relation to the available history[1,23,24]Finally, on completion of the J88, the clinician should conclude whether the findings made during the examination are compatible with the temporal and circumstantial history provided by the victim or (alleged) perpetrator regarding the incident.[1]
Attempts at standardising the clinical record, with specific reference to the structure and quality of the contemporaneous notes, have been a challenging aspect of medical care for many years.[28,29] The format and content of clinical records may be extremely variable, and many attempts have been made to standardise these through the publication of guidelines and the introduction of the problem-orientated medical record.[15,29] The Health Professions Council of South Africa booklet titled Guidelines for Good Practice in the Health Care Professions[30]provides generic guidelines on the documentation and keeping of patient records, but does not specifically address the important medicolegal aspects of documentation.[30] A review of the literature did not yield specific guidelines or publications that provide criteria or parameters by which the completeness or adequacy of contemporaneous clinical records (for purposes of subsequent legal investigation or proceedings) could be consistently measured.
Objectives
To investigate the standard and adequacy of note keeping by medical practitioners when assessing and managing cases of IPV with medicolegal significance. In order to do so, an attempt was made to develop a rubric by which the adequacy of notes (from a medicolegal perspective and in this clinical setting) could be appropriately and consistently assessed. It is hoped that these findings may serve to apprise clinicians of their shared responsibility in facilitating the administration of justice through accurate and appropriate medicolegal records.
Methods
Prior clearance to perform this research was obtained from the Research Ethics Committee of the Faculty of Health Sciences at the University of Pretoria (ref. no. 467/2016).
This was a prospective descriptive study conducted over a period of 18 months from 2016 to 2018. First-contact clinical notes were assessed using standardised rubrics that were developed by the study investigators, based on good clinical practice and record-keeping guidelines and prescribed recommendations from local and international medicolegal literature. The formulation of the rubrics was subjective, but necessary to set standards for appraisal of the clinical records.
A critical appraisal was undertaken, based on the standardised rubric of assessment, of the contemporaneously made 'first-contact' clinical notes, as contained in the hospital files of fatal-outcome cases of IPV. Deceased patients who had received treatment at government hospitals in the Pretoria area but who subsequently succumbed to their injuries and were then referred to the Pretoria Medico-Legal Laboratory for investigation in terms of the requirements of the Inquests Act were included in this study. Children (<18 years) and cases of suicide and accidental death, as well as cases with extremely short survival periods (no medical treatment given) and victims reported dead on arrival at the hospitals, were excluded. A prospective consecutive sampling method with individual case assessment was applied to all cases that met the above inclusion criteria.
Specific terminology and descriptors of the injuries as well as pertinent wound features were assessed using the rubrics and included, but were not limited to, location, size and shape of wounds, apparent age of wounds, probable/possible weapon(s) used, presence or absence of defence-type injuries, etc. Table 1 gives examples of the assessment rubrics.
The records of study cases were furthermore assigned a weighted score based on the comprehensiveness of the documentation, as obtained by applying the standardised assessment rubrics. Scores of 0-2 were assigned to cases with poorly documented descriptions of injuries, where no descriptions or only the location and/or size of the wounds were documented. Scores of 3 - 4 were assigned to cases with relatively comprehensive medicolegal documentation of injuries. A score of 5 was assigned to cases with accurate and complete medicolegal documentation of the injuries, based on the standardised rubrics.
The data analysed were primarily binomial in nature and results are displayed using percentages. A minimum sample size of 97 was calculated to estimate the proportions of interest with 95% confidence to an accuracy of within 10%. One hundred cases were included in the study.
The data extracted from the clinical records were electronically captured using Epi Info 7 software (Centers for Disease Control and Prevention, USA) and subsequently transferred to Excel 2016 (Microsoft, USA) for analysis.
Results
Demographic information
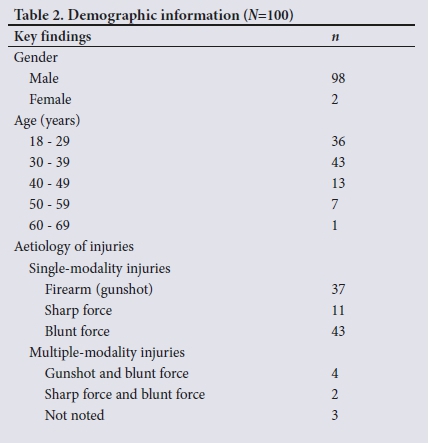
Of the study sample of 100 cases, 79% of victims were aged 18 - 39 and 21% >40 years. The gender distribution was 98% male and 2% female. Blunt-force injury accounted for 43% of cases, firearm injuries for 36% and sharp-force injury (stabbings) for 11% (Table 2).
Medicolegal information documentation
The attending clinicians documented the general body build of the patient in 11% of the 100 cases evaluated. In 20% of cases, the condition of the clothing was documented. The clothing was retained in only 3% of cases, but no further documentation of the chain of custody or specific management, from an evidentiary perspective, was recorded. The date and time of examination were recorded in 76% of cases and the name and signature of the clinician were present in 91%.
A combination of written notes and illustrated diagrams was used in 48% of cases. In 43% of cases only written descriptions were made, and in 4% only graphic illustrations of the injuries were recorded. In 5% of cases the attending clinician failed to document any injury.
The general condition of the patient was noted to be stable in 29% of cases, whereas 39% of patients were reported to be unconscious and 22% had a decreased level of consciousness. In only 2% was the patient reported to be intoxicated.
Various special investigations such as radiological, toxicological and angiographic examinations were performed on 84% of patients as part of the medical management. In 16% of cases, no special investigations were requested or performed. No requests for blood alcohol concentration (BAC) measurements or tests for illicit drugs could be found in the clinical records. The complete results are set out in Table 3.

Gunshot wounds
There were 37 cases of GSWs as a single-modality injury (Table 4). The wounds were specified as entrance or exit wounds in 22 (59.5%) of the 37 cases. Entrance GSWs were documented and described in all 22 of the specified cases and exit GSWs were noted in 8 of the 22 specified cases. In 15 (40.5%) of the 37 cases, the wounds documented by the medical practitioners in the clinical notes were not specified as being either entrance or exit wounds and were only reported as GSWs.
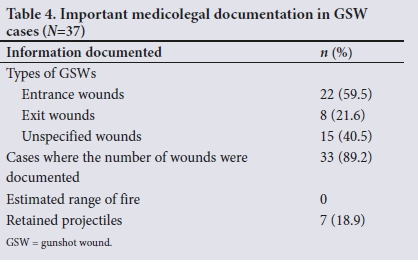
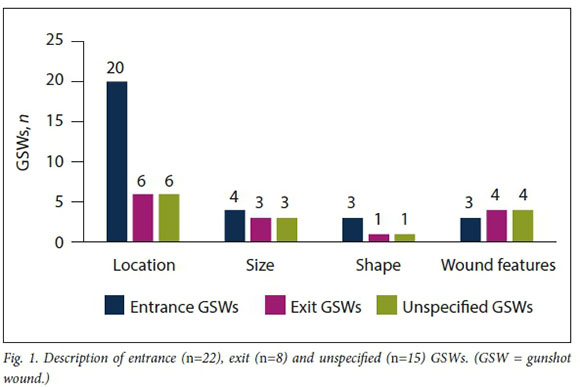
In all the cases of entrance, exit and unspecified GSWs, the locations of the wounds were the most documented descriptor used to report on the wounds (Fig. 1). No reference was made to the estimated range of fire of the GSW in any of the cases.
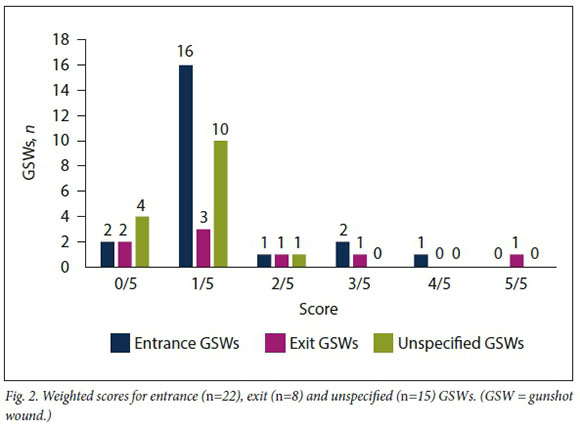
Weighted scores for the description of GSWs were assigned based on the comprehensive description of the injuries. A score of 1 - 2 was assigned for cases where only the location of the wound was described. Cases where there was accurate and comprehensive description of injuries, with specific wound features, were assigned higher weighted scores. A score of 5 was achieved where the descriptors met all the parameters set out in the assessment rubrics. The weighted scores for GSW cases are illustrated in Fig. 2.
Blunt-force injuries
There was a total of 43 blunt-force injury cases in the study (Table 5). The specific type of blunt-force injury was documented in 39 (90.7%) of these. Lacerations were the most prevalent single type of injury (12/39, 27.9%). Multiple types of blunt-force injury (with combinations of blunt-force trauma) accounted for 24 (55.8%) of the total number of blunt-force injury cases. The type of weapon used to inflict the injuries was documented in 8 cases (18.6%), and defence-type injuries were docume nted in 5 (11.6%).
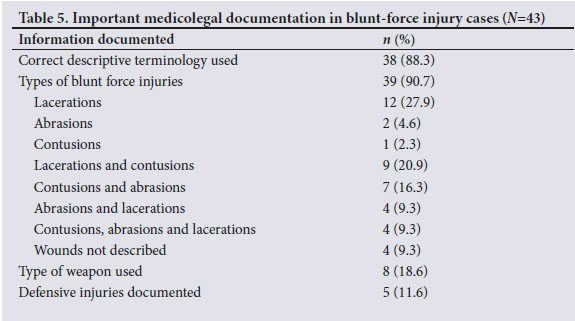
Assessment of the description of the blunt-force injuries (Fig. 3) revealed the location of the wound(s) to be the feature most frequently described. Size only was documented in 15 cases (51.7%) with lacerations, 6 (28.6%) with contusions and 4 (23.5%) with abrasions. The estimated age of the wounds was not documented in any of the cases. The shapes and specific wound features unique to lacerations were described in only 4 (13.8%) of the 29 cases. Specific wound features unique to contusions and abrasions were documented in even fewer cases.
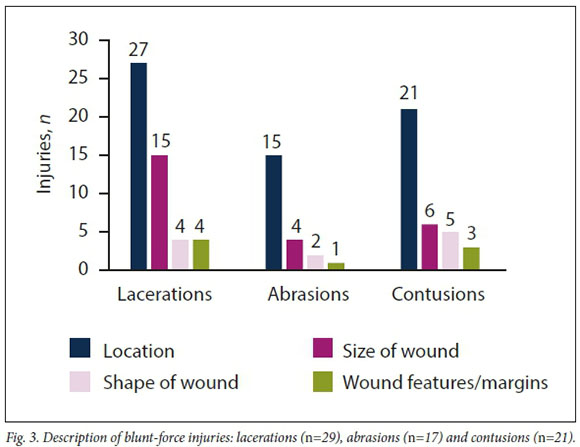
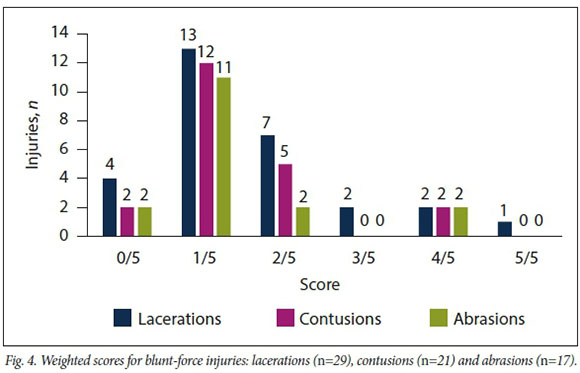
Weighted scores for blunt-force injuries are illustrated in Fig. 4. Only 1 of the cases managed to achieve a weighted score of 5/5. The majority of the cases achieved a score of 1/5 for only documenting the location of the injuries without any further description.
Sharp-force injuries
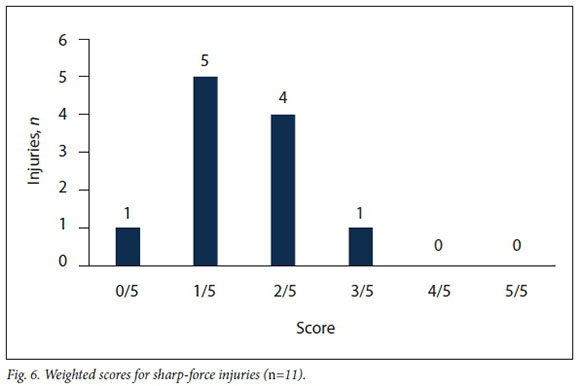
There were ii cases of single-modality sharp-force injuries in the study sample (Fig. 5). The specific type of sharp-force injury was documented in 9 of the ii cases, 8 of which were reported as stab wounds and i as a slash wound. No comment was made on the shape of wounds, and the most reported descriptor was their location. The sizes of stab wounds were documented in 5 (45.5%) of the ii cases. The depths of the wounds were reported in 2 cases (i8.i%), and in only i case did the practitioner comment on the estimated age of the wound.
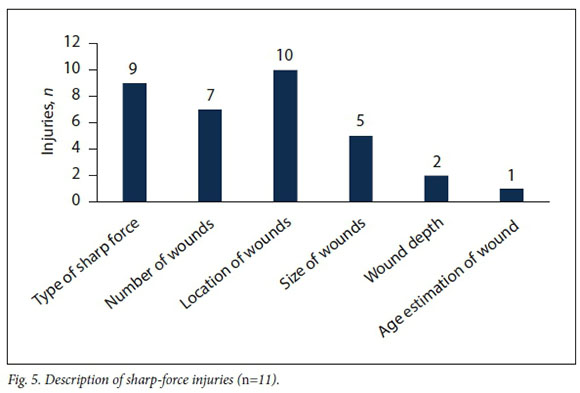
In y (6S.6%) of the ii cases of sharp-force trauma, associated injuries were documented in the clinical records, including S cases of vascular injuries, S cases of pneumothoraces and i case of bowel extrusion. The type of weapon used to inflict the injuries was documented in 2 (i8.i%) of the ii cases of sharp-force injuries, and no mention was made of defensive injuries in any of the reported cases.
Little attention was given to the description of the wounds in cases of sharp-force trauma, with the highest weighted score for this category of injury being S/5 (Fig. 6).
Combination injuries
Of 6 cases of multiple-modality injuries, 4 were combined GSWs and blunt-force injuries and 2 combined sharp-force and blunt-force injuries. The documentation of these cases was similar to those of single-modality injuries. In most cases the location was the only documented descriptor, with occasional mention of the size of the wound.
Discussion
Emergency medical centres are often very busy and complex environments where multidisciplinary teams work under great pressure to manage critically ill or injured patients´[16]It is perhaps understandable that in this setting there may be relatively poor contemporaneous recording of clinical findings (from a medicolegal perspective).[16] However, in a society unduly burdened by violence, and perhaps also with suboptimal investigative work by police and prosecutorial agencies, the importance of meticulous examination and recording of injuries in victims of IPV cannot be overemphasised.[1'11'14'1719'31'32] Indeed, it is within the remit of the attending medical practitioner to do more than simply record the injuries accurately; he or she should manage the case overall from the perspective of identifying, collecting and disposing of evidentiary material for purposes of legal processes (including trace evidence and blood sample collection from victims, disposal of clothing in cases of assault and 'hit-and-run' traffic accidents, and safeguarding of projectiles - to mention but some of the associated responsibilities).[14]
Although the primary duty of the clinician is to attend to the medical needs of the patient/victim, it can be argued that such duties seldom preclude the concurrent discharge of responsibilities from a medico-legal perspective. The latter in most cases essentially requires presence of mind and a few extra minutes for appropriate documentation. Recording the necessary information could be facilitated by protocol-driven and templated reports/forms, generally available in emergency room settings. As clinicians, our duty to the victim and his or her relatives - and to society in general -demands that we do not neglect this aspect of our professional service.![11, 4]
The study investigators set out to test the hypothesis that medical practitioners are not adequately documenting (initial) findings in cases with medicolegal significance. Based on the criteria and rubric(s) for assessment (as developed by the investigators), we submit that this study has shown that there is suboptimal medicolegal documentation in cases of IPV in terms of failure to report on the nature of injuries (size, shape, location, etc.) and to identify and/or collect appropriate evidence (such as condition of clothing, samples for DNA, BAC, retained projectiles and other trace evidence). In this study, using the rubrics referred to, these aspects were appropriately documented and/ or collected in fewer than 20% of cases.
The use of alcohol is strongly associated with IPV.[12] However, this study showed that despite medical practitioners documenting in the clinical record in 22% of cases that the patient had a decreased level of consciousness, no specific clinical findings or parameters were recorded to substantiate or explain this and no tests were requested to establish the BAC or to seek evidence of the presence of other drugs/substances. In only 2% of cases was it recorded that the patient appeared intoxicated, but once again there were no specific clinical notes to validate such observation.
In this study, the use of photography was not documented in any of the cases. Photography can be an extremely useful and valuable tool or method of recording findings in this setting[33-34] Although there may be some additional considerations pertaining to the use of photography in a clinical environment, the Criminal Procedure Act No. 51 of 1977t35] empowers healthcare workers to record evidence in cases where such legal proceedings may be anticipated.!351
In a cross-sectional descriptive study by Fouche et al.[25]based on electronic questionnaires sent to 150 junior doctors throughout SA, 93% of the respondents confirmed that they had treated victims of IPV as community service medical officers. The majority of these participants confidently reported being able to accurately identify blunt-force injuries, but only 54% reported routinely documenting the shape of the wounds, while 38% claimed that they always measured the size of the wounds. In contrast, the present study did not rely on retrospective self-assessment provided by doctors, but attempted to objectively assess the contemporaneous clinical notes. Our results differ substantially from those reported by Fouche' et al.[25]with notably less contemporaneous documentation of these wound features than in the latter study.
The primary purpose of examining and carefully documenting injuries is perhaps to establish the degree or severity of the injury, which assists the doctor in predicting the clinical outcome, and to optimise medical care.[25 31-36]Samuel Farr, author of Elements of Medical Jurisprudence (1788), is quoted as having said, 'There is a kind of medical knowledge which is not so much concerned with the cure of disease as the detection of error and the conviction of guilt.'[37] In the medicolegal/forensic setting, the examination of injuries and wounds will assist the clinician, and later the court, in establishing - among other things - when the injury was sustained (the age of the wound) and what the causative agent or mechanism may have been (blunt force, sharp force, firearm, etc.).!1719-1-311 Clearly, the clinical and medicolegal assessments should preferably take place concurrently.!24] Our study revealed that medical practitioners are not routinely documenting the estimated age of wounds or the presence of specific patterns or features of injury, such as defence type or possible self-inflicted injury.
Whether a particular GSW represents an entrance or exit wound may have great bearing on the legal outcome of a case. However, distinguishing between entrance and exit GSWs can be challenging.[38] A number of factors may impact on or alter the appearance of GSWs, including the type of weapon used, the anatomical location of the wound, the position of the victim at the time of injury, the range from which the victim was shot, and the presence or absence of intermediary objects/targets [32-38] It is therefore vital that the attending clinician should not simply state that a particular (gunshot) wound was an entrance' or exit' wound, but explicitly record the specific features of the wound that were used to assess/categorise it in this way, in order to validate the practitioner's assessment should a subsequent technical query be raised. The results of the present study showed that very little attention was given to the (description of) morphological features of GSWs. The location of the GSW was described in 90.9% of cases, but only very occasionally were features such as size, abrasion collar, smudge ring, soot deposition, etc. recorded. In 7 cases (18.9% of GSW cases) the presence of retained projectiles was recorded - but no record was made of whether the projectile was left in situ or retrieved, or (if removed from the victim) how it was disposed of. The probable type of firearm and/or features of the projectile were not documented in any of the cases. Projectiles (or even fragments thereof) may constitute critically important evidence in criminal proceedings, and these evidentiary items should therefore be treated with the utmost care by healthcare workers, with due regard for preservation of integrity of the item, and secure and accurate packaging and labelling - and for the chain of custody considerations and instructions.[11,14,31l
In cases of IPV, the body of the victim is technically a 'crime scene' and should be treated as such by healthcare workers. The responsibilities of emergency medical staff (paramedics), trauma centre doctors and nurse practitioners in identifying, recording and preserving evidentiary material in this setting (including items such as clothing, projectiles, fluid deposits, etc.) cannot be over-emphasised.!11,14,321 Prescribed and standardised protocols to ensure efficient practice in this regard should be in place in all trauma centres.
The results of this study may be limited by the adequacy and appropriateness of the assessment criteria and rubrics used to evaluate the clinical records, the latter having been designed by the study investigators as novel appraisal tools. Attempts were made to base these rubrics and criteria on accepted and established good clinical practice guidelines, the J88 form and medicolegal literature. It may be argued that the rubrics are inappropriately detailed. It would be a worthwhile exercise for other researchers and clinicians to participate in and contribute towards the development of standardised assessment tools by which the adequacy of clinical records (from a medicolegal perspective) could be consistently judged. Such a 'tool' or guideline could be of great value in civil or criminal legal proceedings in general.
It may be argued that medical students do not adequately realise the gravity and importance of these medicolegal obligations -possibly because they are not 'gatekeepers' of these functions during their training. It is only when they serve as interns or community service doctors, where they are deployed 'at the coalface', that the full scope and nature of their responsibilities may dawn on them. Greater emphasis on these issues during undergraduate training may help to equip doctors better with the awareness and skills to competently perform medicolegal examinations, complete medicolegal documentation, adequately preserve evidence and document medicolegal findings.
It is recommended that protocols for the management of medicolegal cases and the handling of forensic evidence should be developed and implemented at hospital emergency rooms and trauma centres.[14]
Many doctors who are deployed in hospital trauma centres are relatively young and may serve at these centres in a transient or temporary capacity, which would suggest that they may be relatively inexperienced in the clinical forensic context. Moreover, court proceedings may take years to come to fruition, which may greatly complicate the task of investigating officers and prosecutors of later tracing and contacting doctors who may have been involved in such cases. By that time the attending clinician has probably all but forgotten the specific case - another reason why the initial clinical notes should be meticulous and comprehensive.
Medical practitioners should keep in mind that for every fatal outcome of IPV there are an estimated further 20 - 40 victims who sustain injuries, seek medical treatment and survive.[12] Cases with a fatal outcome are therefore the proverbial tip of the iceberg. Although fatal cases may subsequently come under the jurisdiction and scrutiny of dedicated forensic medical practitioners, the vast majority of IPV cases will not involve individuals with such specific training - with the legal process and society largely being dependent on the clinician who first attended to the patient.
Conclusions
SA has one of the highest rates of IPV in the world, which places an immense burden on the healthcare and judicial systems.[2,3,9,11,13,39]
Doctors - and healthcare workers in general in SA - should be aware of their shared responsibility in supporting the justice system in cases of medicolegal significance such as IPV.[1,11,21-24]
This study focused on a small subset of the population, i.e. cases of IPV with a fatal outcome where medicolegal postmortem examinations were subsequently conducted on the bodies of the deceased. The results suggest that there is poor recording of, or attention given to, matters of medicolegal significance in the setting of initial clinical contact, as assessed by review of the medical records. Further studies are needed to assess the validity of the rubrics used by the study investigators as well as the impact of poor record keeping and inadequate medicolegal documentation in non-fatal cases of IPV with actual or anticipated future legal proceedings.
Greater emphasis on undergraduate training may be required to make medical practitioners aware of their shared responsibility in competently performing medicolegal examinations and completing medicolegal documents. The cases in this study were all of a serious nature, with (probably) predictable fatal outcomes, yet the medicolegal aspects of the cases were poorly documented. The question arises: are less serious injuries perhaps even more poorly documented?
Declaration. This publication was a requirement for DPL's MMed (Path) (Forens) degree.
Acknowledgements. The authors thank Prof. Piet Becker for statistical assistance.
Author contributions. DPL: primary study investigator/researcher, design, manuscript preparation, editing, administration, statistical analysis and interpretation; GS: study supervisor, manuscript preparation, editing.
Funding. None.
Conflicts of interest. None.
References
1. Müller K, Saayman G. Clinical forensic medicine: Completing the form J88 - what to do and what not to do. S Afr Fam Pract 2003;45(8):39-43. [ Links ]
2. World Health Organization. Global Status Report on Violence Prevention 2014. Geneva: WHO, 2002. http://www.who.int/viole^e_injury_prevention/violence/status_report/2014/report/report/en/ (accessed 30 January 2019). [ Links ]
3. Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The World Report on Violence and Health. Lancet 2002;360(9339):1083-1088. https://doi.org/10.1016/s0140-6736(02)11133-0 [ Links ]
4. Norman R, Schneider M, Bradshaw D, et al Interpersonal violence: An important risk factor for disease and injury in South Africa. Popul Health Metr 2010;8:32. https://doi.org/10.1186/1478-7954-8-32 [ Links ]
5. Statistics South Africa. Mortality and causes of death in South Africa, 2016: Findings from death notification. Statistical release P0309.3. Pretoria: Stats SA, 2018. http://www.statssa.gov.za/publications/P03093/P030932016.pdf (accessed 30 January 2019). [ Links ]
6. South African Police Service. Crime Statistics 2017/2018. Pretoria: SAPS Corporate Communications, 2018. https://www.saps.gov.za/services/long_version_presentation_april_to_march_2017_2018.pdf (accessed 30 January 2019). [ Links ]
7. Matzopoulos R, Prinsloo M, Pillay-van Wyk V, et al Injury-related mortality in South Africa: A retrospective descriptive study of postmortem investigations. Bull World Health Organ 2015;93(5):303-313. https://doi.org/10.2471/blt.14.145771 [ Links ]
8. Prinsloo M, Bradshaw D, Joubert J, Matzopoulos R, Groenewald P. South Africa's vital statistics are currently not suitable for monitoring progress towards injury and violence Sustainable Development Goals. S Afr Med J 2017;107(6):470-471. https://doi.org/10.7196/SAMJ.2017.v107i6.12464 [ Links ]
9. Bola S, Dash I, Naidoo M, Aldous C. Interpersonal violence: Quantifying the burden of injury in a South African trauma centre. Emerg Med J 2016;33(3):208-212. https://doi.org/10.1136/emermed-2014-204160 [ Links ]
10. Makanga P, Schuurman N, Randall E. Community perceptions of risk factors for interpersonal violence in townships in Cape Town, South Africa: A focus group study. Glob Public Health 2017;12(10):1254-1268. https://doi.org/10.1080/17441692.2015.1123751 [ Links ]
11. Müller K, Saayman G. Forensic science in medicine: What every doctor in SA should know. S Afr Fam Pract 2003;45(6):11-15. [ Links ]
12. Saimen A, Gordon G, Govender I. Non-fatal injuries of interpersonal violence at the Leratong Provincial Hospital, South Africa. S Afr Fam Pract 2016;58(3):80-86. https://doi.org/10.1080/20786190.2016.1167311 [ Links ]
13. Lewis C, Wood D. Interpersonal violence as a major contributor towards the skewed burden of trauma in KwaZulu-Natal, South Africa. S Afr Med J 2015;105(10):827-830. https://doi.org/10.7196/SAMJnew.8380 [ Links ]
14. Vellema J. Forensic evidence in clinical settings. CME 2006;24(2):64-67. [ Links ]
15. Mann R, Williams J. Standards in medical record keeping. Clin Med 2003;3(4):329-332. https://doi.org/10.7861/clinmedicine.3-4-329 [ Links ]
16. Twaij A, Carballido FC, Maryosh J, Pucher PH. Results of a simple intervention to improve documentation quality in major trauma. Eur J Emerg Med 2015;22(2):117-20. https://doi.org/10.1097/mej.0000000000000129 [ Links ]
17. Stark M. Clinical Forensic Medicine: A Physician's Guide. 2nd ed. Totowa, NJ: Humana Press Inc., 2005. [ Links ]
18. Hussien AS, Imam MA, Elsherbiny M, Ellahee N. Introducing a proforma to improve clinical care in trauma surgery. Br J Hosp Med 2015;76(8):472-474. https://doi.org/10.12968/hmed.2015.76.8.472 [ Links ]
19. Mason JK, Purdue BN. Pathology of Trauma. 3rd ed London: Arnold Publishers, 2000. [ Links ]
20. Saukko P, Knight B. Knight's Forensic Pathology. 4th ed. Boca Raton, Fla.: CRC Press, 2016. [ Links ]
21. Schwar T, Loubser J, Olivier J. The Forensic ABC in Medical Practice: A Practical Guide. Durban: Haum Educational Publishers, 1988. [ Links ]
22. Jina R, Kotze JM. Improving the recording of clinical medicolegal findings in South Africa. S Afr Med J 2016;106(9):872-873. https://doi.org/10.7196/SAMJ.2016.v106i9.11081 [ Links ]
23. Kotze JM, Brits H, Botes BA Part 1: Medico-legal documentation: South African Police Services forms, Department of Justice forms and patient information. S Afr Fam Pract 2014;56(5):16-22. [ Links ]
24. Kotze JM, Brits H, Botes BA. Part 2: Medico-legal documentation: Practical completion of pages 1 and 4 of the J88 form. S Afr Fam Pract 2014;56(6):32-37. [ Links ]
25. Fouche L, Bezuidenhout J, Liebenberg C, Adefuye AO. Practice of community-service doctors in the assessment and medico-legal documentation of common physical assault cases. S Afr Fam Pract 2018;60(1):21-25. https://doi.org/10.1080/20786190.2017.1364014 [ Links ]
26. South Africa. National Health Act No. 61 of 2003. https://www.gov.za/sites/default/files/gcis_document/201409/a61-03.pdf (accessed 31 January 2019). [ Links ]
27. South Africa. Health Professions Act No. 56 of 1974. https://www.hpcsa.co.za/Uploads/editor/UserFiles/downloads/legislations/acts/health_professions_ct_56_1974.pdf (accessed 31 January 2019). [ Links ]
28. Carpenter I, Ram MB, Croft GP, Williams JG. Medical records and record-keeping standards. Clin Med 2007;7(4):328-331. https://doi.org/10.7861/clinmedicine.7-4-328 [ Links ]
29. Galappathie N, Jethwa K, Andonovska B. An audit of basic record keeping standards: Lessons learnt from the Royal College of Physicians. Med Sci Law 2008;48(2): 155-158. https://doi.org/10.1258/rsmmsl.48.2.155 [ Links ]
30. Health Professions Council of South Africa. Guidelines for Good Practice in the Health Care Professions: Guidelines on the Keeping of Patient Records. Pretoria: HPCSA, 2016. https://www.hpcsa.co.za/Uploads/editor/UserFiles/downloads/conduct_ethics/Booklet%209.pdf (accessed 31 January 2019). [ Links ]
31. Ohshima T. Forensic wound examination. Forensic Sci Int 2000; 113(1-3): 153-164. https://doiorg/10.1016/s0379-0738(00)00269-3 [ Links ]
32. Saayman G. Gunshot wounds: Medico-legal perspectives. CME 2006;24(3):131-136. [ Links ]
33. Bhangoo P, Maconochie I, Batrick N, Henry E. Clinicians taking pictures - a survey of current practice in emergency departments and proposed recommendations of best practice. Emerg Med J 2005;22(11):761-765. https://doi.org/10.1136/errj.2004.016972 [ Links ]
34. Lenshan G, Pasqualone GA. The importance of forensic photography in the emergency department. J Emerg Nurs 1995;21(6):566-567. https://doi.org/10.1016/s0099-1767(05)80282-x [ Links ]
35. South Africa. Criminal Procedure Act No. 51 of 1977. https://www.gov.za/sites/default/files/gcis_document/201503/act-51-1977s.pdf (accessed 31 January 2019). [ Links ]
36. Sharma BR. The injury scale - a valuable tool for forensic documentation of trauma. J Clin Forensic Med 2005;12(1):21-28. https://doiorg/10.1016/j.jcfm2004.08.002 [ Links ]
37. Farr S. Elements of Medical Jurisprudence. London: T Becket, 1788. https://openlibrary.org/books/OL24243650M/Elements_of_medical_jurisprudence (accessed 30 January 2019). [ Links ]
38. DiMaio VJ. Gunshot Wounds: Practical Aspects of Firearms, Ballistics, and Forensic Techniques. 2nd ed New York: CRC Press, 1999. [ Links ]
39. South African Police Service. An analysis of the national crime statistics: Addendum to the Annual Report 2013/14. http://www.saps.gov.za/about/stratframework/annual_report/2013_2014/crime_statreport_2014_part1.pdf (accessed 30 January 2019) [ Links ]
 Correspondence:
Correspondence:
D P Loots
donovan.loots@up.ac.za
Accepted 9 April 2019.














