Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 no.10 Pretoria oct. 2019
http://dx.doi.org/10.7196/samj.2019.v109i10.14073
IN PRACTICE
ISSUES IN PUBLIC HEALTH
Figures of the dead: A decade of tuberculosis mortality registrations in South Africa
M LovedayI, II; Y N MzobeIII; Y PillayIV; P BarronV
IPhD; Health Systems Research Unit, South African Medical Research Council, Durban, KwaZulu-Natal, South Africa
IIPhD Centre for the AIDS Programme of Research in South Africa, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIMA; Health Systems Research Unit, South African Medical Research Council, Durban, KwaZulu-Natal, South Africa
IVPhD; National Department of Health, Pretoria, South Africa
VBCom, FFCH (SA); School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
South Africa (SA) is committed to reducing tuberculosis (TB) mortality rates in line with the World Health Organization's End TB Strategy and the Sustainable Development Goal (SDG) targets. From mortality reports released by Statistics South Africa, this study analysed reported TB mortality in SA from 2006 to 2016 to inform our understanding of TB mortality and the development of strategies needed to attain the SDG targets. TB mortality includes all deaths reported to the Department of Home Affairs with TB reported as the underlying cause of death based on the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) definition. Although TB remains the leading cause of death, TB mortality rates in SA have fallen substantially in the past decade. From 2006 to 2016, the number of deaths due to TB plummeted from 76 881 to 29 399 and the proportion of all-cause mortality due to TB more than halved from 13% to <6%. Furthermore, the profile of people dying from TB has changed, with a decrease in the proportion of children aged <15 years, adults of reproductive age (15 - 49) and women, and an increase in the proportion aged >50. This change has largely mirrored the overall pattern of deaths in SA, with large decreases in deaths in adults aged 15 - 49, especially women, thought to be because of the scale-up of the antiretroviral treatment programme for HIV. The End TB Strategy target of a 95% reduction in TB mortality by 2035 is achievable in SA. However, sustained effort in high-risk groups together with improved vital registration data are needed to ensure attainment of the target.
Although preventable and treatable, tuberculosis (TB) remains one of the top 10 causes of death worldwide, causing more deaths than HIV/AIDS.[1] In 2017, an estimated 10.0 million people developed TB disease and an estimated 1.8 million deaths were attributed to TB.[1] One of the Sustainable Development Goals (SDGs) is to end the global TB epidemic.[2] To achieve this aim, the End TB Strategy has set targets related to TB mortality, starting with a 35% reduction in TB deaths by 2020, reaching a 95% reduction by 2035.[3] Although the global TB mortality rate is declining, it is likely that many countries will fail to reach these targets and end the TB epidemic by 2035.[4]
Since the emergence of HIV in South Africa (SA), the burden of TB, together with TB mortality, has been influenced by HIV and the extent of antiretroviral therapy (ART) provision, and much of the reduction in TB-related mortality has been due to increased ART provision.[5] However, as TB mortality remains high, further investigation and understanding of who is dying of TB are needed so that we can channel our energy and resources into areas most likely to yield significant gains, enabling us to reach the targets of the End TB Strategy.
All deaths in SA are required to be notified to the Department of Home Affairs via the death certification process. Death certificates are analysed by Statistics South Africa and compiled into official annual mortality reports describing the location of deaths (province), ages and causes of death. We analysed TB-related mortality in SA over the past decade to inform our understanding of TB mortality and the development of strategies needed to end the TB epidemic by 2035.
Methods
We retrospectively analysed the 10 death reports for SA released by Statistics South Africa from 2008 to 2018 on mortality data for the period 2006 - 2016. We extracted data focused on TB as the cause of death and linked this information to place and age of death. No ethical approval for this study was necessary, as only secondary data available in the public domain were used.
In SA, all deaths are supposed to be reported to the Department of Home Affairs within 72 hours by a medical practitioner on a death notification form. In the absence of a medical practitioner, traditional leaders can complete the form. Although a new death notification form with changes in perinatal death registration was introduced in 2009, this would not have affected the classification of deaths attributed to TB. Each death notification form details the age, sex, district and International Statistical Classification of Diseases and Related Health Problems (ICD-10) code. Multidrug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis are included in the deaths attributed to TB.
Results
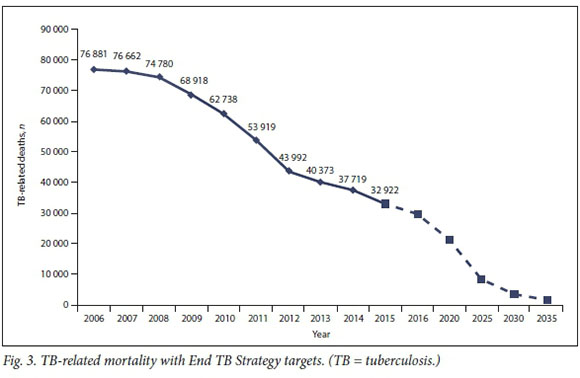
During the decade 2006 - 2016, TB was the number one cause of death in SA (Fig. 1). During this period, the number of deaths due to TB plummeted by 62% from 76 881 to 29 399. Additionally, the proportion of deaths due to TB more than halved from 13% to <6%.
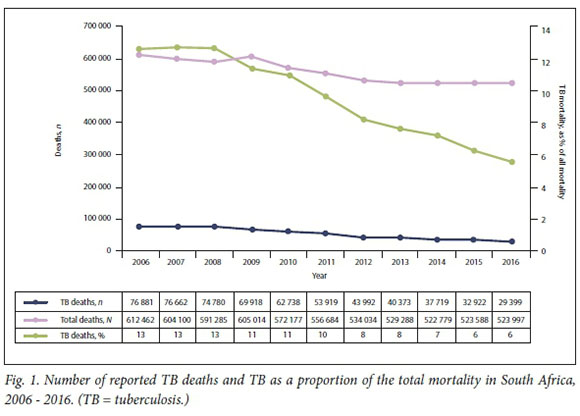
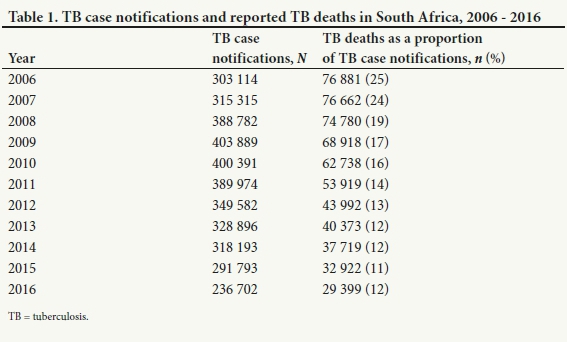
Table 1 shows the decline in TB mortality linked to the total TB caseload in SA. The decline in TB-related mortality occurred at a steeper rate than the decline in the TB case notification rate, resulting in reported TB deaths as a proportion of TB case notifications declining from 25% in 2006 to 12% in 2016.
In addition to a decline in TB-related mortality in SA, the profile of people dying from TB has changed, with the proportion of males dying from TB increasing from 55% to 62% and a corresponding decrease in the female proportion (Table 2). From 2006 to 2016, TB remained the leading cause of death in the male population. However, among females, in both 2015 and 2016 diabetes mellitus and cerebrovascular accidents overtook TB as the leading cause of death.
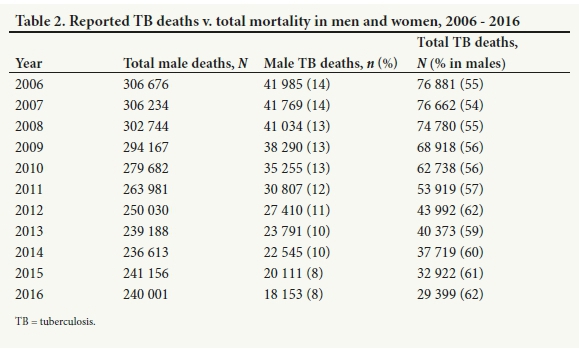
Fig. 2 and Table 3 show the changes in the age of death of people dying from TB. The number of children aged <15 years dying from TB dropped considerably over the period 2006 - 2016, and the proportion of total reported TB deaths in this age group more than halved from 3.4% to 1.5%. Fig. 2 clearly illustrates the precipitous decline in
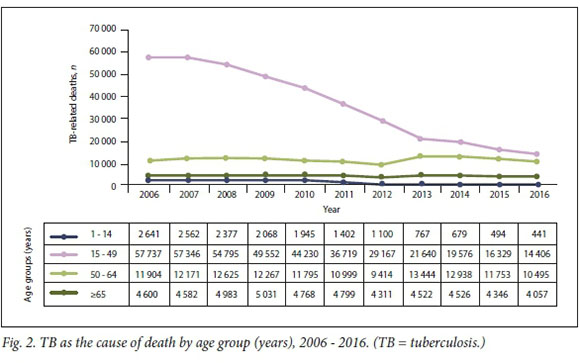
the number of younger adults aged 15 - 49 dying from TB, with the proportion of total reported TB deaths dropping from >70% to less than half. The proportion of total deaths in the 50 - 64 age group and in people aged >65 has increased for two reasons: (i) there has been a decrease in the number of TB deaths in people aged <50 years; and (ii) the number of TB deaths in those aged >50 has been relatively static.
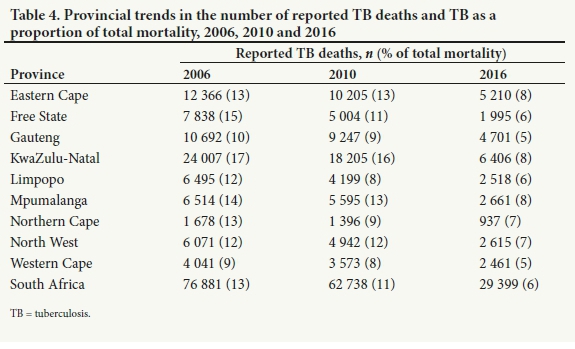
The proportion of deaths attributed to TB in each province varied. Table 4 shows that in all provinc es the number and proportion of reported TB deaths decreased from 2006 to 2016. In Free State and KwaZulu-Natal, the proportion of reported TB deaths more than halved over the decade reviewed. For all provinces, TB was the leading cause of death during this period, except in 2016 in the Western Cape, Gauteng and Limpopo.
In Fig. 3, the decline in TB mortality from 2006 to 2016 is plotted with a solid line. The dotted line from 2016 to 2035 is the projected decline needed to achieve the targets of the End TB Strategy from 2020 to 2035. Given the steady and encouraging decline in TB-related mortality over the past decade, this figure suggests that it is possible for SA to reach the End TB Strategy targets, but a sustained and continued decline in TB-related mortality is necessary.
Discussion
TB has consistently been the leading cause of death in SA over the past two decades. From 1997 TB deaths increased, peaking in 2006 with 76 881 deaths (13% of total mortality). The number of deaths due to TB then steadily declined to 29 399 (6% of total mortality) in 2016. Reducing TB deaths to meet the End TB Strategy mortality target of a 95% reduction in TB mortality (from 2015) by 2035 is within our reach, but will require ongoing focus and effort.
From 1997 to 2006 there was a steady rise in reported TB-related mortality that can be attributed to migration, high levels of patients co-infected with TB and HIV, and the increasing burden of drug-resistant TB (DR-TB).[6-9] However, for a number of possible reasons, TB-related mortality started to decline in 2006 (Fig. 3 and Table 1). The first of these reasons is the intensified ART roll-out for adults, which resulted in marked declines in both HIV/AIDS and TB mortality after 2006.[10,11] According to National Department of Health data, in 2004 an estimated 47 500 people were on ART, compared with >2 million in 2012.[12,13] The evolving clinical eligibility criteria for TB patients co-infected with HIV increased access to ART and probably contributed substantially to the declines in TB-related mortality in the 15 - 44-year age group. [14 Secondly, sustained effort by the TB programme has contributed to a decrease in the number of people becoming infected with TB, improved treatment outcomes, and decreased TB-related mortality.[15] In SA, 53% of people living with HIV are on isoniazid preventive therapy, 39% of the total number of people globally started on preventive therapy, including 32 104 children.!1! Thirdly, increased integration of TB and HIV services at a primary care level together with political attention, civil society mobilisation around TB and HIV, and the launch of a national HIV/ TB campaign in 2011 have helped reduce deaths from TB.[16
However, there are still some groups of people who are at increased risk of TB-related mortality. The first group is patients with DR-TB. Until recently, mortality in patients with DR-TB was much higher than in patients with drug-susceptible TB.[17,18] In 2014 and 2015, the mortality rate of patients treated for TB was 8.4%, compared with 23% for patients treated for DR-TB.[19,20] For patients with DR-TB, the hope is that the new and repurposed drugs and new regimens that have recently been introduced in SA will continue to reduce mortality as they become increasingly accessible.[21] To capitalise on these advances, healthcare workers need to ensure that treatment algorithms are followed carefully and patients are fully informed about the importance of treatment adherence to ensure treatment success and reduce mortality.
A second group of people who are more likely to die of TB are pregnant women. In 2011, it was estimated that worldwide 216 500 pregnant women developed TB, with the greatest burden in Africa.[22] In 2014, it was estimated that TB was responsible for 480 000 deaths among women of child-bearing age.[22] In SA, TB was responsible for 11% of maternal deaths between 2014 and 2016, and it is still the most common non-pregnancy-related infection responsible for maternal mortality.[23] Not only do biological changes in pregnancy double the risk of pregnant women developing TB compared with non-pregnant women,[24,25] but maternal TB has serious health consequences for both mothers and infants, and pregnancy-associated TB can be associated with mortality of up to 40% if untreated.[25] Moreover, the risk of maternal mortality increases dramatically in women co-infected with TB and HIV,[26] and neonates born to these women also have vastly increased morbidity and mortality.[25,27] Routine screening for TB, and immediate commencement of treatment if TB is diagnosed, is important at all antenatal visits. In addition, all newborns of mothers with TB must be screened for TB according to national protocols.
Thirdly, men are more likely to die of TB than women. A number of studies have documented the substantial contribution of TB to the gender disparity in adult mortality, as TB and HIV preventive, diagnostic and treatment programmes have lower coverage of men.[28,29] As proportionally more women engage with HIV services (women have higher HIV diagnosis and ART coverage rates,[30] and lower attrition and mortality rates after initiating ART),[31] they have lower mortality rates from HIV-associated causes, including TB. The faster uptake of life-saving HIV treatment among women led to more rapid declines in HIV-related mortality in women than in men.[5,32] The gender disparity in TB mortality signals the need to improve efforts to target men with preventive, diagnostic and curative health services.
Fourthly, the rise of non-communicable diseases in SA, particularly diabetes, and the interaction of TB with diabetes and HIV increase the risk of TB infection and the chance of poor treatment outcomes, including death. Integrating the control programmes for these three diseases could help prevent TB among people with HIV and diabetes and reduce the mortality and morbidity associated with all three diseases.
Study limitations
Limitations of the data are that our analyses were based on the mortality and cause-of-death reports for SA released by
Statistics South Africa. Vital registration data are used as the basis of these reports, the quality of which is affected by late or incomplete registrations, and ill-defined or misclassified causes of death.'331 Although data completeness and accuracy improved from 2006 to 2016, and by 2016, 96% of the data were complete and 86.8% were accurate, many HIV deaths may have been misclassified as TB owing to reluctance of medical doctors to report HIV on the death certificate or because they did not know the HIV status of the deceased.[33,34] Furthermore, the percentage of deaths classified as due to ill-defined causes during the study period ranged between 12% and 14%, higher than the internationally recommended standard of >10%.[35] Continued improvement of cause-of-death information will increase our understanding of the burden of disease and facilitate monitoring progress towards regional, national and international targets.[10,34]
A further limitation of the vital registration data is that some TB-related deaths may not have been reported as such because postmortem results were not available at the time the death notification form was completed. Furthermore, although there are new diagnostic tests for TB, these still have limited sensitivity.
Conclusions
Reported TB mortality rates in SA have fallen substantially in the past decade, and the End TB Strategy target of a 95% reduction in TB mortality by 2035 is achievable. Besides the strategies for groups of people at risk of mortality described above, implementation of better diagnostics, novel drugs and improved treatment regimens is needed, together with better means of delivery and consistent implementation of all the basic components of a robust TB programme. However, as we have known for centuries, TB is a disease of the poor and we need to address the social determinants that are sustaining it. 'The SDGs are interconnected and health goals will only be achieved if the other SDGs are met too.[35]
Declaration. None.
Acknowledgements. None.
Author contributions. PB and ML conceptualised and designed the study. YNM collected the data. ML, PB and YNM analysed the data, drafted the initial manuscript and revised the manuscript. YP critically reviewed the manuscript. All authors approved the final manuscript as submitted.
Funding. The work was funded by the South African Medical Research Council, the National Research Foundation, and a United Way Worldwide grant made possible by the Lilly Foundation on behalf of the Lilly MDR-TB Partnership. The funders had no role in study design, in the collection, analysis, and interpretation of data, in the writing of the report or in the decision to submit the paper for publication. All researchers were independent of funders and sponsors.
Conflicts of interest. None.
References
1. World Health Organization. Global Tuberculosis Report 2018. WHO/HTM/TB/2018.20. Geneva: WHO, 2018. [ Links ]
2. World Health Organization. Health in 2015: From MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals. Geneva: WHO, 2015. [ Links ]
3. World Health Organization. The End TB Strategy: Global Strategy and Targets for Tuberculosis Prevention, Care and Control after 2015. Geneva: WHO, 2015. [ Links ]
4. Global Burden of Disease Collaborators. Global, regional, and national burden of tuberculosis, 1990 - 2016: Results from the Global Burden of Diseases, Injuries, and Risk Factors 2016 Study. Lancet Infect Dis 2018;18(12):1329-1349. https://doi.org/10.1016/S1473-3099(18)30625-X [ Links ]
5. Reniers G, Blom S, Lieber J, et al. Tuberculosis mortality and the male survival deficit in rural South Africa: An observational community cohort study. PLoS One 2017;12(10):e0185692. https://doi.org/10.1371/journal.pone.0185692 [ Links ]
6. Bocquier P, Collinson M, Clark S, et al. Ubiquitous burden: The contribution of migration to AIDS and tuberculosis mortality in rural South Africa. Etude Popul Afr 2014;28(1):691-701. https://doi.org/10.1016/S0140-6736(09)60916-8 [ Links ]
7. Abdool Karim S, Churchyard G, Abdool Karim Q, Lawn S. HIV infection and tuberculosis in South Africa: An urgent need to escalate the public health response. Lancet 2009;374(9693):921-933. https://doi.org/10.1016/S0140-6736(09)60916-8 [ Links ]
8. Mukadi Y, Maher D, Harries A. Tuberculosis case fatality rates in high HIV prevalence populations in sub-Saharan Africa. AIDS 2001;15(2):143-152. https://doi.org/10.1097/00002030-200101260-00002 [ Links ]
9. Gandhi N, Andrews J, Brust J, et al. Risk factors for mortality among MDR- and XDR-TB patients in a high HIV prevalence setting. Int J Tuberc Lung Dis 2012;16(1):90-97. https://doi.org/10.5588/ijtld.11.0153 [ Links ]
10. Pillay-van Wyk V, Msemburi W, Laubscher R, et al. Mortality trends and differentials in South Africa from 1997 to 2012: Second National Burden of Disease Study. Lancet Glob Health 2016;4(9):e642-e653. https://doi.org/10.1016/S2214-109X(16)30113-9 [ Links ]
11. Larson E, O'Bra H, Brown J, Mbengashe T, Klausner J. Supporting the massive scale-up of anttiretroviral therapy: The evolution of PEPFAR-supported treatment facilities in South Africa, 2005 - 2009. BMC Public Health 2012;12:173. https://doi.org/10.1186/1471-2458-12-173 [ Links ]
12. Pillay Y, Mametja D, Mbengashe T, et al. Joint Review of HIV, TB and PMTCT Programmes in South Africa: Main Report April 2014. Pretoria: National Department of Health, 2014. [ Links ]
13. Johnson L. Access to antiretroviral treatment in South Africa, 2004 - 2011. South Afr J HIV Med 2012;13(1):22-27. https://doi.org/10.4102/sajhivmed.v13i1.156 [ Links ]
14. Fox M, Sannec I, Conradie F, et al. Initiating patients on anttiretroviral therapy at CD4 cell counts above 200 cells/|il is associated with improved treatment outcomes in South Africa. AIDS 2010;24(13):2041-2050. https://doi.org/10.1097/QAD.0b013e32833c703e [ Links ]
15. Churchyard G, Mametja L, Mvusi L, et al Tuberculosis control in South Africa: Successes, challenges and recommendations. S Afr Med J 2014;104(3 Suppl 1):244-248. https://doi.org/10.7196/SAMJ.7689 [ Links ]
16. Heunis J, Kigozi N, Chikobvu P, et al. Risk factors for mortality during TB treatment: A 10-year electronic record review in a South African province. BMC Public Health 2017;17:38. https://doi.org/10.1186/s12889-016-3972-2 [ Links ]
17. Hughes J, Osman M. Diagnosis and management of drug-resistant tuberculosis in South African adults. S Afr Med J 2014;104(12):894-900. https://doi.org/10.7196/SAMJ.9097 [ Links ]
18. Van der Walt MM, Lancaster J, Shean K. Tuberculosis case fatality and other causes of death among multtidrug-resistant tuberculosis patients in a high HIV prevalence setting, 2000 - 2008, South Africa. PLoS One 2016;11(3):e0144249. https://doi.org/10.1371/journalpone.0144249 [ Links ]
19. Vanleeuw L, Loveday M. Tuberculosis. In: Massyn N, Peer N, English R, Padarath A, Barron P, Day C, eds. District Health Barometer 2015/16. Durban: Health Systems Trust, 2016. [ Links ]
20. Vanleeuw L, Mzobe Y, Loveday M. Tuberculosis. In: Massyn N, Padarath A, Peer, N, Day C, eds. District Health Barometer 2016/17. Durban: Health Systems Trust, 2017. [ Links ]
21. Schnippel K, Ndjeka N, Maartens G, et al. Effect of bedaquiline on mortality in South African patients with drug-resistant tuberculosis: A retrospective cohort study. Lancet Respir Med 2018;6(9):699-706. https://doi.org/10.1016/S2213-2600(18)30235-2 [ Links ]
22. Sugarman J, Colvin C, Moran A, Oxlade O. Tuberculosis in pregnancy: An estimate of the global burden of disease. Lancet Glob Health 2014;2(12):e710-e716. https://doi.org/10.1016/S2214-109X(14)70330-4 [ Links ]
23. National Department of Health, South Africa. Saving Mothers 2014 - 2016: Seventh Report on the Confidential Enquiries into Maternal Deaths in South Africa. Short report. Pretoria: NDoH, 2017. https://www.sasog.co.za/Content/Docs/Saving_Mothers.pdf (accessed 2 April 2019). [ Links ]
24. Zenner D, Kruijshaar M, Andrews N, et al. Risk of tuberculosis in pregnancy: A national, primary care based cohort and self-controlled case series study. Am J Respir Crit Care Med 2012;185(7):779-784. https://doi.org/10.1164/rccm.201106-1083OC [ Links ]
25. Mathad JS, Gupta A. Tuberculosis in pregnant and postpartum women: Epidemiology, management, and research gaps. Clin Infect Dis 2012;55(11):1532-1549. https://doi.org/10.1093/cid/cis732 [ Links ]
26. Zumla A, Bates M, Mwaba P. The neglected global burden of tuberculosis in pregnancy. Lancet Glob Health 2014;2(12):e675-e676. https://doi.org/10.1016/S2214-109X(14)70338-9 [ Links ]
27. Ribeiro P, Jacobsen K, Mathers C, et al. Priorities for women's health from the Global Burden of Disease study. Int J Gynaecol Obstet 2008;102(1):82-90. https://doi.org/10.1016/j.ijgo.2008.01.025 [ Links ]
28. Neyrolles O, Quintana-Murci L. Sexual inequality in tuberculosis. PLoS Med 2009;6(12):e1000199. https://doi.org/10.1371/journal.pmed.1000199 [ Links ]
29. Horton KC, MacPherson P, Houben R, et al. Sex differences in tuberculosis burden and notifications in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med 2016;13(9):e1002119. https://doi.org/10.1371/journal.pmed.1002119 [ Links ]
30. Druyts E, Dybul M, Kanters S, et al. Male sex and the risk of mortality among individuals enrolled in antiretroviral therapy programs in Africa: A systematic review and metaanalysis. AIDS 2013;27(3):417-442. https://doi.org/10.1097/QAD.0b013e328359b89b [ Links ]
31. Cornell M, Schomaker M, Garone DB, et al. Gender differences in survival among adult patients starting antiretroviral therapy in South Africa: A multicentre cohort study. PLoS Med 2012;9(9):e1001304. https://doi.org/10.1371/journal.pmed.1001304 [ Links ]
32. Bor J, Rosen S, Chimbindi N, et al. Mass HIV treatment and sex disparities in life expectancy: Demographic surveillance in rural South Africa. PLoS Med 2015;12(11):e1001905. https://doi.org/10.1371/journal.pmed.1001905 [ Links ]
33. Statistics South Africa. Mortality and Causes of Death in South Africa, 2016: Findings from Death Notification. Pretoria: Stats SA, 2016. [ Links ]
34. Joubert J, Rao C, Bradshaw D, Vos T, Lopez AD. Evaluating the quality of national mortality statistics from civil registration in South Africa, 1997 - 2007. PLoS One 2013;8(5):e64592. https://doi.org/10.1371/journal.pone.0064592 [ Links ]
35. Grobusch M, Kapata N. Global burden of tuberculosis: Where we are and what to do. Lancet Infect Dis 2018;18(12):1291-1293. https://doi.org/10.1016/S1473-3099(18)30654-6 [ Links ]
 Correspondence:
Correspondence:
M Loveday
marian.loveday@mrc.ac.za
Accepted 26 July 2019














