Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 n.6 Pretoria Jun. 2019
http://dx.doi.org/10.7196/samj.2019.v109i6.14002
IN PRACTICE
CLINICAL ALERT
Rational use of the fluoroquinolones
G A RichardsI; A J BrinkII; C FeldmanIII
IMB BCh, PhD, FCP (SA), FRCP; Department of Critical Care, Charlotte Maxeke Johannesburg Academic Hospital and Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB ChB, MMed (Clin Micro); Department of Medical Microbiology, Faculty of Health Sciences, University of Cape Town, South Africa
IIIMB BCh, DSc, FCP (SA), FRCP; Department of Internal Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
The systemic fluoroquinolones (FQs) have recently been reported to be associated with significant side-effects in susceptible individuals. This has prompted the Food and Drug Administration (FDA) in the USA and the European Medicines Agency (EMA) to issue warnings regarding their use. The FQs should not be used for common bacterial infections, such as urinary tract infections, travellers' diarrhoea and upper and lower respiratory tract infections, unless it is not possible to use another oral agent. There are situations, however, in which these agents are not only effective, but their benefit outweighs the risk. These include the management of conditions such as acute prostatitis, typhoid fever, prosthetic joint infections, multidrug-resistant tuberculosis, certain hospital-acquired infections and situations where the organism is susceptible to FQs, which could then be administered orally. Alternatively, the patient would have to be admitted to hospital for parenteral therapy.
The systemic fluoroquinolones (FQs) have been used for >30 years for a variety of infectious conditions, and have been among the most widely prescribed antibiotics globally. In the USA, 32.5 million prescriptions for oral FQs were issued in 2015, representing 101 prescriptions/ 1 000 population, and of these, ciprofloxacin comprised 20.3 million or 63 prescriptions/1 000 population.[1] In the hospital setting, ~3.8 million patients billed for an injectable FQ in 2011.[2]
During this time, these drugs were lifesaving in many instances, but were also associated with significant adverse effects, including peripheral neuropathy, photosensitivity, prolonged QT interval, hypoglycaemia and tendon rupture. The Food and Drug Administration (FDA) in the USA and the European Medicines Agency (EMA) have highlighted these and other adverse effects and have suggested that, where possible, alternative agents should be used.[3,4]
New adverse events and warnings
More recently, these warnings have been extended to include a potential risk for aortic dissection, with an increased risk from a baseline of 9/100 000 to 300/100 000, and a recommendation that the FQs should be avoided in patients at risk of an aortic aneurysm, including the elderly and those with peripheral vascular disease, uncontrolled hypertension, vasculitic syndromes and diseases such as Marfan's and Ehlers-Danlos syndromes.[5-
The EMA has also extended a warning of potential tendon rupture to include tendinitis, myalgia, muscle weakness, arthralgia and joint swelling, and also warned of a syndrome that includes peripheral neuropathy, psychosis, anxiety, insomnia, depression, hallucinations, suicidal thoughts, confusion and impairment of vision, hearing, smell and taste.[6,7] Older patients, those with renal dysfunction, transplant recipients and those receiving concomitant corticosteroids are at higher risk of side-effects. According to the FDA and EMA, FQs 'can be associated with prolonged (up to months or years) serious, disabling and potentially irreversible drug reactions affecting several, sometimes multiple, systems, organ classes and senses'.[6] The overall condition has been termed 'fluoroquinolone-associated disability syndrome' (FADS).[7] The existence of the entire constellation of FADS relies on patient testimony and does not as yet have a recognised pathogenetic mechanism. Therefore, the actual incidence of FADS is not known. With regard to tendon rupture, tendinitis and aortic aneurysm, FQs display a high affinity for connective tissue, particularly in cartilage and bone. In an evaluation of the incidence in >11000 patients, rates for tendinitis of 2.4 /10 000 prescriptions, and for tendon rupture of 1.2/10 000 prescriptions, have been reported.[8]
Mechanisms of harm
There are many proposed mechanisms for these adverse events, which include ischaemia, degradation of the tendon matrix and an alteration of tenocyte activity.[9- FQs, and in particular ciprofloxacin, also enhance matrix metalloproteinase expression in tendon tissue and reduce collagen synthesis by inhibition of tenocyte proliferation.[10,11- A very recent and important publication has shown that ciprofloxacin inhibits mitochondrial topoisomerase 2-beta, which regulates supercoiling of mitochondrial DNA. This results in accumulation of positively supercoiled DNA, which causes transcription and replication initiation failure with depletion of mitochondrial DNA copy number.[12- This effect might be caused by oxidative damage, which FQs induce in various cell types.[13,14- This blocks cellular proliferation and differentiation and may provide a reason for the prolonged effects seen in some patients.
Whatever the aetiology and incidence of these conditions, EMA and FDA reports have led to considerable confusion among the general public and healthcare practitioners as to when it would be appropriate to use these agents.
Is there any place for the fluoroquinolones?
Whereas it is relatively easy to decide which patients should not receive FQs, does this mean that we should abandon these agents as a class? The FQs should not be used to treat mild or moderate bacterial infections unless other antibacterial agents commonly recommended for these infections cannot be used. Conditions that should not be treated with a FQ (or any antibiotic) include viral infections, the common cold, influenza, acute bronchitis and pharyngotonsillitis (unless <16 years of age and streptococcus is suspected, and even in that case one can wait until results of a rapid test for group A streptococcus are available, and if antibiotics are indicated, a number of other more narrow-spectrum antibiotics are as effective).[15]
Travellers' diarrhoea
Similarly, diarrhoea not associated with fever, bloody stools or other signs of systemic sepsis (i.e. those caused by shigella, campylobacter, Clostridium difficile, and protozoal infections) does not benefit from any antibiotic, including metronidazole, even in the immunocompromised host. Antibiotics - FQs in particular - should be avoided in this setting, as they are ineffective and predispose to colonisation of the gut by resistant organisms.[16] Most cases of travellers' diarrhoea are caused by enterotoxigenic Escherichia coli (ETEC), occur in the first week of travel, are usually mild (<6 stools/ day) and do not disrupt normal activities. Most cases last 3 - 5 days and resolve without treatment. When the diarrhoea is associated with additional symptoms, as indicated above, and with interruption of normal activities, it is classed as moderate to severe and may need to be treated with an antibiotic. FQs have been the traditional agents used in this setting; however, several systematic reviews that compared antibiotics, e.g. FQs, azithromycin, and rifaximin v. placebo, showed consistent shortening of duration of diarrhoea from 3 days to 1.5 days with the use of all these antibiotics. If an antibiotic is used, it is best to avoid a FQ and preferably use azithromycin for only 1 - 3 days.[17,18]
Salmonella infections (typhi and paratyphi)
Whereas empiric treatment is based on regional susceptibility, FQs are considered by many experts to be the drug of choice for susceptible isolates; it is still reasonable to use these agents in this setting.[19,20] However, with regard to empiric therapy, 1 in 7 isolates of Salmonella typhi in SA is resistant to FQs, whereas 100% are susceptible to azithromycin, which may be an appropriate initial choice.[21] Thereafter, antibiogram-directed therapy is vital. Other alternatives include third-generation cephalosporins; however, extended-spectrum beta-lactamase production, which renders these organisms resistant to ceftriaxone, is an increasing problem in both typhoid and paratyphoid infections. If the organism is sensitive to both ceftriaxone and FQs, patients improve more rapidly with the latter; however, the combination of ceftriaxone and azithromycin leads to more rapid resolution than ceftriaxone alone and may be an effective option.[221 Treatment is for 2 weeks with either agent.
Lower respiratory tract infections
With regard to community-acquired pneumonia, FQs, particularly moxifloxacin or levofloxacin, have been recommended as alternatives to beta-lactams (BLs), especially in the case of severe allergy. It is recommended that they should only be used as a last resort, where no other agent is available.[23]
With regard to acute exacerbations of chronic obstructive pulmonary disease, only patients with a C-reactive protein of >40 mg/L, those who have all three of the following symptoms, i.e. increased sputum volume, purulence and dyspnoea, or two of these features, where one is increased sputum purulence, should receive an antibiotic. When an antibiotic is deemed necessary, appropriate therapy should usually consist of a BL, inclusive of amoxicillin, cefuroxime or cefpodoxime, a combination of a BL and a BL inhibitor or a macrolide, where pneumococcal resistance to macrolides is low. For hospitalised patients with the risk of pseudomonas or other more-resistant organisms, antipseudomonal agents, such as piperacillin-tazobactam or cefepime, may be considered. It is recommended that these patients have a sputum culture performed, and that the antibiotic choice be based, where possible, on the results.[24]
With regard to bronchiectasis, where the patient is not considered ill enough to require hospital admission, and the cultured organism is a pseudomonas or one of the Enterobacteriaceae sensitive to ciprofloxacin but resistant to other oral antibiotics, the FQs could be considered.
Urinary tract infections and prostatitis
With regard to urinary tract infections, it is reasonable to use an oral FQ where resistance dictates that the alternative would be to admit the patient to hospital to use a parenteral agent, such as a carbapenem. It is important, however, that microscopy and culture of urine be performed to optimise therapy and that the prescription be based on sensitivities.
Acute bacterial prostatitis, as opposed to chronic prostatitis (which is usually not bacterial in origin), is due to E. coli in 58 - 88% of cases, Proteus species in 3 - 6%, other enterobacterales, i.e. Klebsiella, Enterobacter and Serratia species in 3 - 11%, Pseudomonas aeruginosa in 3 - 7% and occasionally Staphylococcus aureus and streptococcal or enterococcal infection.[25-27] Although there are no comparative trials evaluating optimal antimicrobial therapy, FQs are a reasonable choice, provided that the organism is sensitive and that the alternative would be the need to admit the patient to hospital for parenteral therapy. Ciprofloxacin attains a ~2-fold higher concentration in the prostate than in the plasma, and levofloxacin a ~3-fold higher concentration. More recently, high-dose oral fosfomycin has been recommended as an effective outpatient therapy. An oral regimen of 3 g daily for 1 week, followed by 3 g every second day for a total treatment duration of 6 - 12 weeks or 3 g every second or third day for 6 weeks, appears to be effective.[28-30] This has recently been confirmed to be extremely effective in a prospective observational study of 44 patients, where the majority of organisms were FQ resistant. Cure was achieved in 82% at end of treatment (EOT) and in 80% and 73% at 3 and 6 months, respectively. Microbiological eradication was achieved in 86% and 77% at EOT and 6 months, respectively.[31] The longer course was reserved for patients with prostatic calcification.
Other agents that penetrate prostatic fluid and would be effective if the organism is sensitive are the macrolides, trimethoprim-sulfamethoxazole (TMP/SMX) and doxycycline.[27,32] If the organism is resistant to these agents, admission is required for intravenous therapy with antibiotics, such as ertapenem, tigecycline or ceftriaxone, the latter particularly in the case of Neisseria gonorrhoeae. Community-acquired enterococcal infections can be treated with amoxicillin, and staphylococcal infections with oral cloxacillin or intravenous (IV) cefazolin (1 g IV every 8 hours). If there are risk factors, or a history of methicillin-resistant S. aureus, vancomycin or linezolid may be administered.
Prosthetic joint infections and osteomyelitis
The FQs are useful in the management of prosthetic joint infection (PJIs) if the offending organism is susceptible. Management is primarily surgical and a 2-stage arthroplasty is most commonly employed. Antibiotic therapy is most frequently administered for 6 weeks, initially for 2 weeks with parenteral therapy and thereafter for 4 weeks with oral therapy.[33] Oral ciprofloxacin is often effective against many Gram-negative pathogens and has also been used successfully with rifampicin for staphylococcal infections in an IV to oral switch if the organism is susceptible.[34] However, other oral anti-staphylococcal agents that might be effective are TMP/SMX and clindamycin. Oral linezolid has limited use, given the toxicity that occurs after 14 days of therapy.
A very recent study showed that oral therapies, including the FQs, were effective in treating osteomyelitis.[35] Depending on susceptibility, a FQ would be acceptable if it decreased the duration of IV therapy and allowed earlier discharge of patients. Patients would have to be observed closely for adverse events, given the long duration of use.
Intensive care unit-acquired infections
Intensive care unit (ICU) use of the FQs has been limited because of the potential for this class of drugs to cause collateral damage, i.e. enhance the emergence of resistance in organisms for which the antibiotic was not originally intended.[36] However, FQs are used as carbapenem-sparing agents for extended-spectrum beta-lactamase producers if they are sensitive, and along with TMP/SMX are also valuable for the treatment of organisms such as Stenotrophomonas maltophilia and Burkholderia cepacia.[37,38]
Meningococcal prophylaxis
Meningococcal infections are potentially fatal and easily transmissible. Prophylaxis is warranted for close contacts and for exposed healthcare workers. A single dose of ciprofloxacin 500 mg was the recommended protocol; however, as it is not known if duration of therapy is necessarily the determinant of toxicity, and because ciprofloxacin resistance has been reported, it may be wise to use an alternative regimen. This consists of rifampicin 600 mg twice daily for 2 days or a single dose of ceftriaxone IV.[39-41] This regimen might not always be practical if all the children in a classroom need prophylaxis. Paediatric doses differ from those for adults.
Mycobacterial infections
Another indication for FQ use is the management of Mycobacterium avium intracellulare infections; however, FQs have generally been relegated to second-line therapy, as outcomes are inferior to macrolide-based regimens, specifically clarithromycin or azithromycin, along with ethambutol, and rifamycins (rifampicin, rifabutin), with or without aminoglycosides in more severe infections.[42,43]
The new World Health Organization guidelines for the management of multidrug-resistant Mycobacterium tuberculosis include levofloxacin/moxifloxacin, linezolid and bedaquiline in their category A agents, i.e. those that should be used first.[44] Thereafter, the recommendation is to use agents in categories B or C if those in the preceding category cannot be used. It is unlikely that this recommendation would be withdrawn, given the potential toxicities of the other agents and the high mortality of patients with the disease.
Fluoroquinolone use in situations of beta-lactam allergy
When considering an alternative agent to BL, it should be recognised that BL allergy is exceedingly rare and, where an allergy to penicillin exists, there is little cross-reactivity between the second- and third-generation cephalosporins. Unless the patient has developed a severe reaction inclusive of urticaria or anaphylaxis (type 1 reaction), or severe non-IgE-mediated reactions, such as Stevens-Johnson syndrome/toxic epidermal necrolysis, drug-induced hypersensitivity syndrome, drug reaction with eosinophilia and systemic symptoms (DRESS syndrome), renal failure, cytopenias, serum sickness or any other life-threatening reaction, the first- and second-generation cephalosporins can be considered safe.[45] It is, however, probably necessary to perform allergy testing more frequently than is currently done, as most patients who believe they are allergic to BL are probably not.[46]
Conclusions
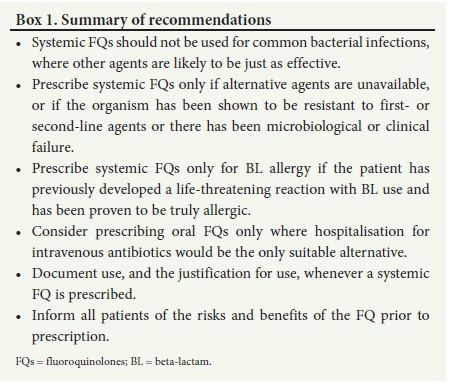
The overall aim is to reduce the use of FQs, probably also as topical agents, as there is emerging evidence that they may also be harmful when used in this manner.[47] However, as mentioned above, there is a role for these agents in certain circumstances, both in the community and in hospital. It is nevertheless important to be aware that prescription of FQs may have significant unwanted consequences and it is therefore important to consider carefully the circumstances where use would be rational.
A summary of recommendations is given in Box 1.
Declaration. None.
Acknowledgements. None.
Author contributions. GAR wrote the manuscript, with input from CF and AJB.
Funding. None.
Conflicts of interest. GAR has received honoraria from MSD, AstraZeneca, Fresenius, Pfizer, Ranbaxy, Cipla, Adcock Ingram, Dr Reddy, Astellas and Novartis. AJB has received honoraria from MSD and Pfizer. CF has received honoraria from Abbott, AstraZeneca, Cipla, Inova Pharma, MSD, Novartis and Pfizer.
References
1. Centers for Disease Control. Outpatient antibiotic prescriptions - United States, 2015. https://www.cdc.gov/antibiotic-use/community/pdfs/Annual-Report-2015.p (accessed 15 February 2019). [ Links ]
2. Food and Drug Administration Drug Safety Communication. FDA updates warnings for oral and injectable fluoroquinolone antibiotics due to disabling side effects. https://www.fda.gov/Drugs/DrugSafety/ucm511530.htm (accessed 15 February 2019). [ Links ]
3. Food and Drug Administration Drug Safety Communication. FDA requires label changes to warn of risk for possibly permanent nerve damage from antibacterial fluoroquinolone drugs taken by mouth or by injection. http://waybackarchive-it.org/7993/20170112031629/http://www.fda.gov/Drugs/DrugSafety/ucm365050.htm (accessed 15 February 2019). [ Links ]
4. Food and Drug Administration. FDA reinforces safety information about serious low blood sugar levels and mental health side effects with fluoroquinolone antibiotics; requires label changes. https://www.fda.gov/Drugs/DrugSafety/ucm611032.htm (accessed 15 February 2019). [ Links ]
5. Food and Drug Administration. FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients. https://www.fda.gov/Drugs/DrugSafety/ucm628753.htm (accessed 15 February 2019). [ Links ]
6. European Medicines Agency. Quinolone- and fluoroquinolone-containing medicinal products. 2018. https://www.ema.europa.eu/en/medicines/human/referrals/quinolone-fluoroquinolone-containing-medicinal-products (accessed 18 February 2019). [ Links ]
7. European Medicines Agency. Summary of the EMA public hearing on quinolone and fluoroquinolone antibiotics: Public hearing held on 13 June 2018. https://www.ema.europa.eu/documents/report/summary-ema-public-hearing-quinolone-fluoroquinolone-antibiotics_en.pdf (accessed 15 February 2019). [ Links ]
8. Wilton LV, Pearce GL, Mann RD. A comparison of ciprofloxacin, norfloxacin, ofloxacin, azithromycin, and cefixime examined by observational cohort studies. Br J Clin Pharmacol 1996;41(4):277-284. [ Links ]
9. Childs SG. Pathogenesis of tendon rupture secondary to fluoroquinolone therapy. Orthop Nurs 2007;26(3):175-182. [ Links ]
10. Vyas H, Krishnaswamy G. Imaging in clinical medicine: Quinolone-associated rupture of the Achilles tendon. N Engl J Med 2007;357(20):2067. [ Links ]
11. Corps AN, Curry VA, Harrall RL, Dutt D, Hazleman L, Riley GP. Ciprofloxacin reduces the stimulation of prostaglandin E(2) output by interleukin-1beta in human tendon-derived cells. Rheumatology (Oxford) 2003;42(11):1306-1310. https://doi.org/10.1093/rheumatology/keg372 [ Links ]
12. Hangas A, Aasumets K, Kekalainen NJ, et al Ciprofloxacin impairs mitochondrial DNA replication initiation through inhibition of topoisomerase 2. Nucleic Acids Res 2018;46(18):9625-9636. https://doi.org/10.1093/nar/gky793 [ Links ]
13. Dogan Z, Cetin A, Elibol E, Vardi N, Turkoz Y. Effects of ciprofloxacin and quercetin on fetal brain development: A biochemical and histopathological study. J Matern Fetal Neonatal Med 2019;32(11):1783-1791. https://doi.org/10.1080/14767058.2017.1418222 [ Links ]
14. Pouzaud F, Dutot M, Martin C, Debray M, Warnet JM, Rat P. Age-dependent effects on redox status, oxidative stress, mitochondrial activity and toxicity induced by fluoroquinolones on primary cultures of rabbit tendon cells. Comp Biochem Physiol C Toxicol Pharmacol 2006;143(2):232-241. [ Links ]
15. Brink AJ, van Wyk J, Moodley, et al. The role of appropriate diagnostic testing in acute respiratory tract infections: An antibiotic stewardship strategy to minimise diagnostic uncertainty in primary care. S Afr Med J 2016;106(6):554-561. https://doi.org/10.7196/SAMJ.2016.v106i6.10857 [ Links ]
16. Kantele A, Mero S, Kirveskari J, Laaveri T. Fluoroquinolone antibiotic users select fluoroquinolone-resistant ESBL-producing Enterobacteriaceae (ESBL-PE). Data of a prospective traveller study. Travel Med Infect Dis 2017;16:23e30. https://doi.org/10.1016/j.tmaid.2017.01.003 [ Links ]
17. Barrett J, Brown M. Clinical review: Travellers' diarrhoea. BMJ 2016;353:i1937. https://doi.org/10.1136/bmj.i1937 [ Links ]
18. Steffen R, Hill DR, duPont HL. Traveler's diarrhea: A clinical review. JAMA 2015;313(1):71-80. https://doi.org/10.1001/jama.2014.17006 [ Links ]
19. Humphries RM, Fang FC, Aarestrup FM, Hindler JA. In vitro susceptibility testing of fluoroquinolone activity against Salmonella: Recent changes to CLSI standards. N Engl J Med 2007;357(20):2067. [ Links ]
20. Crump JA, Mintz ED. Global trends in typhoid and paratyphoid fever. Clin Infect Dis 2010; 50(20):241-246. [ Links ]
21. GERMS-SA Annual Report 2017. http://www.nicd.ac.za/wp-content/uploads/2018/08/GERMS-SA-AR-2017-final.pdf (accessed 22 February 2019). [ Links ]
22. Meltzer E, Stienlauf S, Leshem E, et al. A large outbreak of Salmonella paratyphi A infection among Israeli travelers to Nepal. Clin Infect Dis 2014;58(3):359-364. https://doi.org/10.1093/cid/cit723 [ Links ]
23. Boyles TH, Brink A, Calligaro GL, et al. South African guideline for the management of community-acquired pneumonia in adults. J Thorac Dis 2017;9(6):1469-1502. https://doi.org/10.21037/jtd.2017.05.31 [ Links ]
24. Feldman C, Richards GA. Appropriate antibiotic management of bacterial lower respiratory tract infections. F1000Res 2018;7: pii:F1000 Faculty Rev-1121. https://doi.org/10.12688/f1000research.14226.1 [ Links ]
25. Millán-Rodríguez F, Palou J, Bujons-Tur A, et al. Acute bacterial prostatitis: Two different subcategories according to a previous manipulation of the lower urinary tract. World J Urol 2006;24(1):45-50. https://doi.org/10.1007/s00345-005-0040-4 [ Links ]
26. Etienne M, Chavanet P, Sibert L, et al. Acute bacterial prostatitis: Heterogeneity in diagnostic criteria and management. Retrospective multicentric analysis of 371 patients diagnosed with acute prostatitis. BMC Infect Dis 2008;8:12. https://doi.org/10.1186/1471-2334-8-12 [ Links ]
27. Lipsky BA, Byren I, Hoey CT. Treatment of bacterial prostatitis. Clin Infect Dis 2010;50(12):1641. https://doi.org/10.1086/652861 [ Links ]
28. Los-Arcos I, Pigrau C, Rodríguez-Pardo D, et al. Long-term fosfomycin-tromethamine oral therapy for difficult-to-treat chronic bacterial prostatitis. Antimicrob Agents Chemother 2016;60(3):1854-1858. https://doi.org/10.1128/AAC.02611-15 [ Links ]
29. Zhanel GG, Zhanel MA, Karlowsky JA. Oral fosfomycin for the treatment of acute and chronic bacterial prostatitis caused by multidrug-resistant Escherichia coli. Can J Infect Dis Med Microbiol 2018;30:404813. https://doi.org/10.1155/2018/1404813 [ Links ]
30. Zhanel GG, Zhanel MA, Karlowsky JA. Intravenous fosfomycin: An assessment of its potential for use in the treatment of systemic infections in Canada. Can J Infect Dis Med Microbiol 2018;2018:12039. https://doi.org/10.1155/2018/8912039 [ Links ]
31. Karaiskos I, Galani L, Sakka V, et al. Oral fosfomycin for the treatment of chronic bacterial prostatitis. J Antimicrob Chemother 2019;pii:dkz015. https://doi.org/10.1093/jac/dkz015 (epub ahead of print). [ Links ]
32. Church DL. Prostatitis. Infect Dis Antimicrob Agent http://www.antimicrobe.org/e53.asp (accessed 15 February 2019). [ Links ]
33. Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet 2016;387(10016):386-394. https://doi.org/10.1016/S0140-6736(14)61798-0 [ Links ]
34. Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE, and the Foreign-Body Infection (FBI) Study Group. Role of rifampin for treatment of orthopedic implant-related staphylococcal infections: A randomized controlled trial. JAMA 1998;279(19):1537-1541. [ Links ]
35. Li HK, Rombach I, Zambellas R, et al. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med 2019;380(5):425-436. https://doi.org/10.1056/NEJMoa1710926 [ Links ]
36. Paterson DL. 'Collateral damage' from cephalosporin or quinolone antibiotic therapy. Clin Infect Dis 2004;15(38)(Suppl 4):S341-S345. [ Links ]
37. Wang YL, Scipione MR, Dubrovskaya Y, Papadopoulos J. Monotherapy with fluoroquinolone or trimethoprim-sulfamethoxazole for treatment of Stenotrophomonas maltophilia infection. Antimicrob Agents Chemother 2014;58(1):176-182. https://doi.org/10.1128/AAC.01324-13 [ Links ]
38. Pegues DA. Burkholderia cepacia complex. Antimicrobe. http://www.antimicrobe.org/b19.asp (accessed 15 February 2019). [ Links ]
39. Centers for Disease Control and Prevention (CDC). Emergence of fluoroquinolone-resistant Neisseria meningitidis - Minnesota and North Dakota, 2007 - 2008. MMWR Morb Mortal Wkly Rep 2008;57(7):173-175. [ Links ]
40. Cohn AC, MacNeil JR, Clark TA, et al. Prevention and control of meningococcal disease: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62(RR-2):1-28. [ Links ]
41. Schwartz B, Al-Tobaiqi A, Al-Ruwais A, et al. Comparative efficacy of ceftriaxone and rifampicin in eradicating pharyngeal carriage of group A Neisseria meningitidis. Lancet 1988;1(8597):1239-1242. [ Links ]
42. Deshpande D, Gumbo T. Pharmacokinetic/pharmacodynamic-based treatment of disseminated Mycobacterium avium. Future Microbiol 2011;6(4):433-439. https://doi.org/10.2217/fmb.11.25 [ Links ]
43. Kasperbauer SH, Daley CL. Diagnosis and treatment of infections due to Mycobacterium avium complex. Semin Respir Crit Care Med 2008;29(5):569-576. https://doi.org/10.1055/s-0028-1085708 [ Links ]
44. World Health Organization. Rapid communication: Key changes to treatment of multidrug- and rifampicin-resistant tuberculosis (MDR/RR-TB). https://www.who.int/tb/publications/2018/WHO_RapidCommunicationMDRTB.pdf (accessed 25 February 2019). [ Links ]
45. Vaisman A, McCready J, Hicks S, Powis J. Optimizing preoperative prophylaxis in patients with reported b-lactam allergy: A novel extension of antimicrobial stewardship. J Antimicrob Chemother 2017;72(9):2657-2660. https://doi.org/10.1093/jac/dkx171 [ Links ]
46. Macy E, Vyles D. Who needs penicillin allergy testing? Ann Allergy Asthma Immunol 2018;121(5):523-529. https://doi.org/10.1016/j.anai.2018.07.041 [ Links ]
47. Wang X, Winterstein AG, Alrwisan A, Antonelli PJ. Risk for tympanic membrane perforation after quinolone ear drops for acute otitis externa. Clin Infect Dis 2019;pii:ciz345. https://doi.org/10.1093/cid/ciz345 (epub ahead of print). [ Links ]
 Correspondence:
Correspondence:
G A Richards
guy.richards@wits.ac.za
Accepted 7 March 2019














