Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 no.3 Pretoria mar. 2019
http://dx.doi.org/10.7196/samj.2019.v109i3.13367
RESEARCH
Evaluation of factors and patterns influencing the 30-day readmission rate at a tertiary-level hospital in a resource-constrained setting in Cape Town, South Africa
R DreyerI; A J ViljoenII
IMB ChB, BSc Hons (Clin Pharm), MMed (Int Med), FCP (SA); Department of Internal Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
IIFCP (SA); Department of Internal Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND: Factors contributing to and causes of hospital readmissions have been investigated worldwide, but very few studies have been performed in South Africa (SA) and none in the Western Cape Province
OBJECTIVES: To investigate possible preventable and non-preventable factors contributing to readmissions to the Department of Internal Medicine at Tygerberg Hospital (TBH), Cape Town, within 30 days of hospital discharge. The researchers tested a risk-stratification tool (the LACE index) to evaluate the tool's performance in the TBH system
METHODS: A retrospective analysis was conducted of all 30-day readmissions (initial hospitalisation and rehospitalisation within 30 days) to the Department of Internal Medicine at TBH for the period 1 January 2014 - 31 March 2015. Potential risk factors leading to readmission were recorded
RESULTS: A total of 11 826 admissions were recorded. Of these patients, 1 242 were readmitted within 30 days, representing a readmission rate of 10.5%. The majority of patients (66%) were readmitted within 14 days after discharge. The most important risk factor for readmission was the number of comorbidities, assessed using the Charlston score. The study also identified a large burden of potentially avoidable causes (35% of readmissions) due to system-related issues, premature discharge being the most common. Other reasons for 30-day readmission were nosocomial infection, adverse drug reactions, especially warfarin toxicity, inadequate discharge planning and physician error
CONCLUSIONS: Despite TBH being a low-resource, high-turnover system, the 30-day readmission rate was calculated at 10.5%. Global readmission rates vary from 10% to 25%, depending on the reference article/source used. We found that 35% of 30-day readmissions were potentially avoidable. Venous thromboembolism was a minor contributor to readmission but was associated with a very high mortality rate. A secondary outcome evaluated was the utility of the LACE and modified LACE (mLACE) index in the TBH environment. The risk tool performed well in the TBH population, and a high LACE and mLACE score correlated with an increased risk of 30-day readmission (p<0.001
Unplanned readmission of patients remains a significant contributor to healthcare costs worldwide. It also further exposes the patient to hospital pathogens and potential additional procedures with associated complications. Globally, readmission rates vary from 10% to 25%, depending on the criteria used.[1]
A hospital readmission occurs when a patient who has been discharged from a hospital is admitted again within a specified time interval. Readmission rates have increasingly been used as an outcome measure in health services research and as a quality benchmark for health systems.[2] These unplanned readmissions are multifactorial, and causes are both preventable and non-preventable. They can be influenced by factors inherent to the specific healthcare system and can be an important measure of a medical system's efficacy.[3]
Various risk assessment tools are available to assess whether a patient is ready for discharge, the overall risk of mortality, and the risk of 30-day readmission. These tools stratify patients into categories depending on the extent of comorbidities and include the LACE score, the LACE+ score, the PRA score (Probability of Repeated Admission), GAP (General Assessment of Preparedness) and the BOOST model.[4-6]
Approximately 73% of the population of the Western Cape Province, South Africa (SA), is dependent on public sector healthcare. This figure reflects national health demographics. Owing to socioeconomic challenges, the government is unable to provide adequately for this population, leading to inadequate hospital bed numbers, premature discharge, and poor follow-up and palliative services after discharge.
Objectives
Patients readmitted to the Department of Internal Medicine at Tygerberg Academic Hospital (TBH), Cape Town, within 30 days of discharge were assessed. Characteristics of preventable and unpreventable readmissions were compared and potentially avoidable factors were identified. We sought to identify readmissions that were potentially avoidable, defined as preventable by a change in clinical decision-making by a clinician under the current standard of care.
The performance of validated risk-stratification tools (the LACE index and modified LACE (mLACE) index, Table 1) was reviewed to assess their effectiveness in the TBH system.
Methods
A retrospective descriptive analysis of all patients readmitted to the Department of Internal Medicine at TBH within 30 days of discharge from 1 January 2014 to 31 March 2015 was done. A period of 14 months was used to increase the number of cases and augment the validity of the study.
Data were captured and potential contributing factors were assessed. These were grouped into five categories indicating the reason for readmission, as follows: (i) discharge-related factors (premature discharge or inadequate discharge planning); (ii) disease progression; (iii) patient-related factors (non-adherence, poor social support); (iv) adverse events (healthcare-associated infections, thromboembolic diseases, physician errors, adverse drug reactions (ADRs)); and (v) system-related failure (lack of access to information or counselling). Since readmissions may be multifactorial, depending on whether the reviewing physician considered the factor a major contributor, more than one factor could be documented. Once the contributing factors had been assessed, readmitted cases were grouped into readmissions that were potentially preventable or unpreventable.
Patient demographics were assessed in terms of comorbidity prevalence, prevalence of HIV, length of stay (LoS), days since discharge, causes for readmission within 30 days, and whether admissions were potentially avoidable (deemed preventable) v. deemed not to be preventable.
Inclusion and exclusion criteria
All adult patients admitted to the Department of Internal Medicine and living in the TBH district health system (DHS) drainage area were assessed. To prevent selection bias, patients living outside the TBH DHS area were excluded from the study. This was because TBH acts as both a primary and a referral hospital, so patients living in an area served by a referring hospital may primarily be readmitted to their local hospital. For this reason, their inclusion could have caused lost records and bias. Patients admitted for delivery and for elective procedures such as transplants, chemotherapy and surgical procedures were also excluded.
Data collection
Using the TBH electronic patient management system, the records of patients readmitted within 30 days were identified and perused and a database indicating the reasons for admission, comorbidities and potential avoidable and unavoidable risk factors was created. Causes of readmission were clearly defined.
Finally, the medical records of all readmissions deemed preventable were reviewed to determine how the readmission might have been prevented, and the results were tabulated. This method of assessment was developed to indicate preventability based on independent review by the researchers.
Ethical considerations
The study was approved by the Health Research Ethics Committee at Stellenbosch University and TBH (ref. no. S15/07/157). All patient identification was removed for the purposes of confidentiality.
Statistical analysis
SPSS Statistics for Windows, version 24.0 (IBM, USA) was used to analyse the data. Descriptive comparisons of three patient groups (Table 2) involved reporting of frequency counts and group percentages for categorical variables. Pearson's χ2 test was applied to assess associations between the LACE and mLACE score categories and the three groups of patients. A p-value <0.05 was considered statistically significant.
Results
A total of 11 826 medical admissions were recorded during the study period. Of these patients, 1 242 were readmitted within a 30-day period, giving a readmission rate of 10.5%. The 1 242 patients were then divided into two categories, namely patients who lived in the TBH DHS drainage area and those who did not. A total of 472 patients readmitted within 30 days lived in the designated area. Of these, 7 were excluded owing to missing medical records.
The records of the remaining 465 patients were scrutinised to determine whether the two admissions (index admission and readmission) were related or unrelated. After analysing the readmission diagnoses and attempting to find a causal relationship between the two admissions, 13% (n=59) of readmissions were classified as unrelated and the remaining 87% (n=406) as related, according to the predefined criteria listed in Table 2. A third group (the control group) was obtained by drawing a random sample of patients without a 30-day readmission for the same time period (Table 2).
The gender distribution was similar in the three groups. In both readmitted groups, the majority of patients (>71.5%) were aged <65 years. It is cause for concern that 39% of patients in the related readmissions group and 40% in the unrelated readmissions group were aged <50 years.
The prevalence of patient comorbidities in the related readmissions group was significantly higher than in the control group. However, there was a significantly higher prevalence of respiratory diseases in the control group. This could be because they were randomly assigned as participants in the study and were therefore not matched for demographics beforehand.
Comorbidities included chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis and post-tuberculosis (TB) structural lung disease. The latter could be explained by the high TB burden in the Western Cape. Hypertension, diabetes, renal impairment and cardiovascular system diseases other than those listed above were the most common comorbidities among patients with a 30-day readmission. Smoking and alcohol use were similar in the three groups, in all of which their prevalence was high. No illicit substances were investigated.
In both the readmitted groups, most patients (66%) were readmitted within 14 days from the index admission.
On categorising causes of readmission, it was evident that almost 40% of patients were readmitted due to progression of their disease. This is an unavoidable cause, especially with chronic deteriorating diseases such as COPD and congestive cardiac failure (CCF).
The most prevalent diseases in the index admission that led to related readmission were cardiac failure, infections, COPD, cancer and cerebrovascular accidents (CVAs). Of the 406 patients with a related readmission, 246 (61%) were readmitted a second time. In this group the diagnoses in the second admission were similar to those in the first, except for ADRs, the rate of which was much higher.
In the unrelated admissions group, infections were the most common initial presenting diagnosis, followed by minor complaints, cardiac failure and CVAs. The most common readmission diagnoses in this group were TB, renal failure, overdoses and CVAs. CVAs were more prevalent in the control group than in the two readmissions groups.
The control group had a much higher prevalence of infections than the two readmissions groups. This makes sense given the fact that infections, once diagnosed and treated, should strictly speaking not lead to readmission. The rate of TB was also higher in the control group than in the other two groups. However, TB was the sixth most common diagnosis leading to readmission, possibly reflecting the chronic nature of this disease.
There was no marked difference in LoS between the readmitted patients and those in the control group. However, patients diagnosed with certain conditions such as CCF and COPD, which frequently led to readmission, tended to have a relatively short LoS compared with the control group (median 3 days v. 4 days). Other chronic conditions such as liver disease and renal disease had a LoS of >5 days, and for connective tissue diseases LoS was up to 12 days.
When evaluating potentially avoidable causes for 30-day readmission, the biggest contributor was premature discharge (10%), followed by inadequate discharge planning (7%), physician-related errors (5%) and ADRs and nosocomial infections (4%).
We identified 33 ADRs, of which 19 were deemed potentially avoidable. Seventeen of these patients had warfarin toxicity. It was perturbing that 6 of these 17 patients presented with warfarin toxicity at both the index admission and the readmission. One patient had a recorded international normalised ratio >4.5 on the day of discharge. The records did not specify whether this result was acted on by the discharging clinician.
In the study, non-compliance and socioeconomic factors were classified as unavoidable, as they are factors that physicians may struggle to change. Although education is imperative to minimise the risk of non-compliance, this responsibility remains the patient's.
Non-compliance was responsible for almost 10% of readmissions, and lack of social support for 6%. A potential caveat regarding the non-compliance rate is the fact that most patients are discharged from hospital with a 1-month supply of chronic medication. If the readmission period had been longer, the non-compliance rate might have been higher, but further research in this area needs to be done.
Challenges surrounding palliative care and social support should be brought to the attention of the relevant department, which could attempt to address these socioeconomic issues.
On assessing the performance of the risk scores in the population studied, there was a strong association between readmission and severity score for both the LACE (p<0.001 and mLACE indices (p<0.001), indicating that both LACE and mLACE may be useful tools in risk stratification of the TBH population.
There was a clear trend towards a higher LACE score (>10 -see Table 1) in the readmitted groups, with 59% of the related readmissions presenting a high risk (score >10) v. only 35% of the control group.
We studied the prevalence of HIV in all the groups. A cause for concern is that there was a very low uptake of HIV screening. In 91.4% (n=371) of all related readmissions, a HIV test was not done at either of the admissions. This fact was validated through reviewing all databases, including medical and National Health Laboratory Service records and referral letters. Given the high prevalence of HIV in SA, this issue needs urgent attention.
Discussion
Reducing hospital readmissions is a focus of healthcare systems worldwide in efforts to improve efficiency. Readmission rates are considered an important measure of a health system's effectiveness, as they can be influenced by many factors inherent to the specific system.[1,7] The worldwide readmission rate varies from 10% to 25%, depending on the country studied.
Readmission can pose such a problem that some healthcare funders have introduced penalties to providers when rates are above a specified threshold.[3] This is done both to reduce costs and to improve health outcomes, as hospitals will be encouraged to provide better care to avoid readmissions.
Vashi et al.[8] found that although the readmission rate in their cohort was only 14.7%, another 9.7% of patients were what they called 'treat-and-release visits' who visited the emergency department within 30 days of being discharged and were treated there. These cases obviously impact on hospital resources and should therefore also be considered.[8,9]
Factors associated with an increased risk of readmission
Factors associated with an increased risk of hospital readmission include unavoidable sociodemographic circumstances such as age, gender, ethnicity, living conditions and specific diagnoses. Other risk factors are poor overall health and functional disability, as well as previous admissions within the past 6 months.
Some factors that increase readmissions are modifiable. These include organisational factors such as LoS, method of referral and discharge destination. A 2016 review[10] listed additional factors such as major surgery, discharging patients too soon, quantity of medication at discharge, failure to relay crucial information to the outpatient setting, and whether or not patients have a regular healthcare provider.[10]
Despite being a resource-limited setting with very high bed pressure and a high turnover rate, TBH has a 30-day readmission rate of 10.5%, which appears to be on a par with rates reported elsewhere (10 - 20%).[1,11]
Demographics. Age has been shown to be an independent risk factor for 30-day readmission regardless of the quality of medical care provided, probably owing to multiple comorbidities in the elderly patient population. In one study of individuals aged >50 years, 42% of admissions were due to chronic cardiorespiratory illnesses. In the study by Vashi et al.,[8]many readmissions were judged to be potentially preventable, mainly through improved education.[8,12] The present study showed a trend towards older patients being readmitted, with 15% aged >75 years, compared with 7% in the control group. Significantly, however, 71.5% of patients who were readmitted were aged <65 years.
Days since discharge. In the present study, 41% of patients in the related readmissions group were readmitted within 7 days of being discharged, and in both the readmitted groups 60% were readmitted within 14 days. These figures indicate that a high proportion of patients were either not fit for discharge or developed an adverse event necessitating readmission.
Length of stay. There was no marked difference between the readmitted patients and those in the control group, with median stays of 4 days in all three groups. In the two readmitted groups, patients with certain conditions such as CCF and COPD, which commonly led to readmission, tended to have a short LoS compared with some chronic conditions such as liver disease, renal disease and connective tissue diseases, which had a mean LoS of 5 - 12 days. Short LoS in conditions that carry significant morbidity could be because high bed pressure led to premature discharge - a leading cause for potentially avoidable readmission.
Diagnoses leading to readmission. As reported elsewhere, CCF and COPD are commonly associated with readmission.[3] In the present study the most common diagnosis leading to readmission was CCF, followed by infections, COPD, cancer and CVAs.
Appropriateness of discharge. Analysis by Auerbach and Kripalani[10] and Kripalani et al.[11] revealed that only 12 - 34% of discharge summaries reached aftercare providers by the time of the first post-hospitalisation appointment. In addition, discharge documentation was often inaccurate and lacked important information such as noting additional workup indicated after discharge.
Adverse events. Therapeutic errors are a major contributor to preventable readmission. One study showed that ~20% of patients were readmitted as a result of therapeutic errors.[13] Despite this, not all patients with treatment errors (preventable adverse effect of care) present to healthcare facilities. The figure could even be higher than that given above. Approximately 60% of such adverse events were determined to be potentially preventable.[13] In a 2014 review by Schoonover et al.,[14] 41 - 94% of patients had at least one medication discrepancy at different points in transition, and 29 - 38% of those discrepancies had the potential to cause harm.
Information is limited on the burden of serious ADRs in sub-Saharan Africa, which has high prevalences of HIV infection and TB. In a study in four SA hospitals[15] the most common ADRs were renal impairment, hypoglycaemia, liver injury and haemorrhage; 45% of these were considered to be preventable. Various drugs were implicated, including warfarin. In the present study, 33 ADRs were identified, of which 19 were deemed potentially avoidable. Of these, 17 (nearly 90%) were due to warfarin toxicity. Still more perturbing was the fact that 6 of these 17 patients presented with warfarin toxicity at both their index and 30-day admissions.
Nosocomial infections. A total of 33 patients presented with infections at readmission. Although all were initially managed as nosocomial infections, only 14 of these infectious diagnoses were eventually attributed to nosocomial causes.
Physician-related errors. Physician errors (incorrect diagnosis and direct errors) were responsible for 5% of readmissions, which is a high figure. However, the literature shows that a training institution is a risk factor, as treatment of patients by junior staff members could lead to diagnostic errors. This factor probably contributed to the 5% of readmissions at TBH that were due to potentially avoidable errors and highlights the fact that supervising consultants should be constantly vigilant. Close supervision of junior staff is crucial.
Thromboembolic events. These usually occur within 7 days of hospital discharge, in the form of deep-vein thrombosis or pulmonary embolism. With the advent of anticoagulation for prophylaxis they can easily be prevented. In the present study they accounted for very few readmissions (<2%) but were associated with a significant mortality rate (70%). We recommend increased awareness and commitment to preventive strategies. The well-known Padua and Caprini risk assessment could be used in this situation.[16,17]
Risk-stratification tools
There are various risk assessment tools available to gauge whether a patient is ready for discharge, the overall risk of mortality, and the risk of 30-day readmission. These tools stratify patients into categories depending on the extent of comorbidities and include the LACE score, LACE+ score, PRA score (Probability of Repeated Admission), GAP (General Assessment of Preparedness) score and BOOST model.
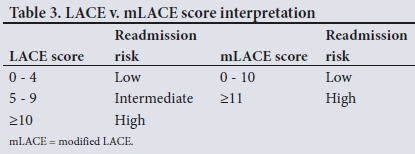
The LACE score incorporates four parameters: length of stay of the index admission (L), acuity of the admission (A), comorbidities, incorporating the Charlston comorbidity index (C), and number of emergency department visits in the past 6 months (E) (Table 1).[4,18] A LACE score of >10 provides a good threshold to differentiate between patients with low/medium and high risk of readmission, while an mLACE a score of >11 identifies the high-risk patient (Table 3). High-risk patients are 2.6 times more likely to be readmitted than those at low risk.[5,6,18]
The LACE tool has been validated to correlate well with the risk of 30-day readmission. According to Au et al.,'4-use of this model exhibited a 20.5% net reclassification improvement over the Charlston score alone.
In the present study, both the Charlston co-morbidity scores and the LACE scores were higher for the readmitted groups than for the control group. The LACE score was high in 59% of the patients who were readmitted v. only 35% of the control group. This was statistically significant, with a strong association between readmission and both the LACE and mLACE scores (p<0.001 for both, χ2 test).
Conclusions and recommendations
The 30-day readmission rate in the TBH Department of Internal Medicine was calculated at 10.5%. This is an acceptable rate and compares favourably with published international rates of 10 - 20%.
Many patients were readmitted within the first 14 days, which is probably an indication of unresolved issues from their initial admission.
Venous thromboembolism contributed to few readmissions but had a high mortality rate (70%). Implementation of preventive strategies is urgently needed.
There was an even spread of chronic medical conditions across all age groups and our figures reflect a relatively young population with multiple comorbidities, not only due to the HIV/TB pandemic but also to non-communicable diseases such as cardiovascular conditions. In this regard, lifestyle and education need to be addressed at a national level.
There was a low rate of HIV testing in all groups, and we recommend increased uptake of HIV counselling and testing, in line with National Department of Health policy.
The above strategies, which can potentially decrease the 30-day readmission rate and ultimately improve patient care and limit costs related to readmissions, will require resources to be channelled into the areas identified.
Declaration. None.
Acknowledgements. The authors thank the study subjects, their colleagues who assisted with the study, and TBH management for allowing them to perform the study.
Author contributions. Both authors made significant contributions. RD and BV contributed to the design and conception of the study and to acquisition, analysis and interpretation of data. RD drafted the article, which was subsequently critically reviewed by BV.
Funding. None.
Conflicts of interest. None.
REFERENCES
1. García-Pérez L, Linertová R, Lorenzo-Riera A, Vázquez-Díaz JR, Duque-González B, Sarría-Santamera A. Risk factors for hospital readmissions in elderly patients: A systematic review. QJM 2011;104(8):639-651. https://doi.org/10.1093/qjmed/hcr070 [ Links ]
2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-forservice program. N Engl J Med 2009;360(14):1418-1428. https://doi.org/10.1056/NEJMsa0803563 [ Links ]
3. Donze J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: Retrospective cohort study. BMJ 2013;347:f7171. https://doi.org/10.1136/bmj.f7171 [ Links ]
4. Au AG, McAlister FA, Bakal JA, Ezekowitz J, Kaul P, van Walraven C. Predicting the risk of unplanned readmission or death within 30 days of discharge after a heart failure hospitalization Am Heart J 2012;164(3):365-372. https://doi.org/10.1016/j.ahj.2012.06.010 [ Links ]
5. Damery S, Combes G. Evaluating the predictive strength of the LACE index in identifying patients at high risk of hospital readmission following an inpatient episode: A retrospective cohort study. BMJ Open 2017;7(7). https://doi.org/10.1136/bmjopen-2017-016921 [ Links ]
6. El Morr C, Ginsburg L, Nam S, Woollard S. Assessing the performance of a modified LACE index (LACE-rt) to predict unplanned readmission after discharge in a community teaching hospital. Interact J Med Res 2017;6(1):e2. https://doi.org/10.2196/ijmr.7183 [ Links ]
7. Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 2010;303(17):1716-1722. https://doi.org/10.1001/jama.2010.533 [ Links ]
8. Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA 2013;309(4):364-371. https://doi.org/10.1001/jama.2012.216219 [ Links ]
9. Kamerow D. Reassessing hospital readmission penalties. BMJ 2013;346:f1043. https://doi.org/10.1136/bmj.f1043 [ Links ]
10. Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med 2016;176(4):484-493. https://doi.org/10.1001/jamainternmed.2015.7863 [ Links ]
11. Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission: Current strategies and future directions. Annu Rev Med 2014;65 (1):471-485. https://doi.org/10.1146/annurev-med-022613-090415 [ Links ]
12. Stanley A, Graham N, Parrish A. A review of internal medicine re-admissions in a peri-urban South African hospital. S Afr Med J 2008;98(4):291-294. [ Links ]
13. Forster AJ, Shojania KG, van Walraven C. Improving patient safety: Moving beyond the 'hype' of medical errors. CMAJ 2005;173(8):893-894. https://doi.org/10.1503/cmaj.1041582 [ Links ]
14. Schoonover H, Corbett CF, Weeks DL, Willson MN, Setter SM. Predicting potential postdischarge adverse drug events and 30-day unplanned hospital readmissions from medication regimen complexity. J Patient Saf 2014;10(4):186-191. https://doi.org/10.1097/PTS.0000000000000067 [ Links ]
15. Mouton JP, Njuguna C, Kramer N, et al. Adverse drug reactions causing admission to medical wards: A cross-sectional survey at 4 hospitals in South Africa. Medicine (Baltimore) 2016;95(19):e3437. https://doi.org/10.1097/MD.0000000000003437 [ Links ]
16. Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility: A randomized trial. Ann Intern Med 2010;153(1):8-18. https://doi.org/10.7326/0003-4819-153-1-201007060-00004 [ Links ]
17. Obi AT, Pannucci CJ, Nackashi A, et al. Validation of the Caprini venous thromboembolism risk assessment model in critically ill surgical patients. JAMA Surg 2015;150(10):941-948. https://doi.org/10.1001/jamasurg.2015.1841 [ Links ]
18. Van Walraven C, Wong J, Forster AJ. LACE+ index: Extension of a validated index to predict early death or urgent readmission after hospital discharge using administrative data. Open Med 2012;6(3):e80-e90. [ Links ]
 Correspondence:
Correspondence:
R Dreyer
rdreyerinc@gmail.com
Accepted 8 August 2018














