Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.109 n.1 Pretoria Jan. 2019
http://dx.doi.org/10.7196/samj.2019.v109i1.13061
RESEARCH
Transitions between lifetime alcohol use, regular use and remission: Results from the 2004 South African Stress and Health Survey
N Harker BurnhamsI, II; C BharatIII; D R WilliamsIV; D J SteinV, VI; B MyersVII
IPhD; Alcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Cape Town, South Africa
IIPhD; School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IIIBSc Hons; National Drug and Alcohol Research Centre, University of New South Wales, Sydney, Australia
IVPhD; Harvard TH. Chan School of Public Health, Harvard University, Boston, USA
VMB ChB, PhD; South African Medical Research Council Risk and Resilience in Mental Disorders Unit, Department of Psychiatry, Faculty of Health Sciences, University of Cape Town, South Africa
VIMB ChB, PhD; Department of Psychiatry, Faculty of Health Sciences, University of Cape Town, South Africa
VIIPhD; Alcohol, Tobacco and Other Drug Research Unit, South African Medical Research Council, Cape Town, South Africa
ABSTRACT
BACKGROUND. Hazardous alcohol consumption presents a serious threat to the health and wellbeing of all people and is linked to chronic and acute health problems.
OBJECTIVES. To: (i) estimate the prevalence of alcohol use disorders and remission from alcohol abuse and dependence in the South African (SA) population; and (ii) determine whether age of onset, education, sex and level of cohort alcohol use are associated with commencement of use, regularity of use, and transitions to and remission from more harmful levels of use.
METHODS. The study was a nationally representative sample of 4 315 individuals aged >18 years. In a multistage, area probability sample of adults, data were collected from 4 311 alcohol users using the World Mental Health Survey Initiative version of the Composite International Diagnostic Interview version 3.0. All analyses were carried out using SAS version 9.4.
RESULTS. Of the respondents, 40.6% indicated lifetime use of alcohol, 35.3% reported regular use, and 8.8% met diagnostic criteria for alcohol abuse and 2.7% for alcohol dependence. The prevalence of remission from lifetime abuse without dependence was 55.9%. The median age of onset of alcohol use was 20 years, with transition from use to regular use occurring within ~1-3 years. The results suggest that males, students (compared with those who had completed a high level of education) and greater alcohol use in the respondent's birth cohort were all associated with increased odds of commencing alcohol use. For transitions from use to regular use, increased odds were associated with males, greater birth cohort alcohol use, low education and later (>21 years) onset of first alcohol use.
CONCLUSIONS. Our findings suggest that cohort alcohol use is associated with transition to commencement of use and from use to regular use in the general SA population. The study further highlighted the need for interventions among males and university students, given that hazardous alcohol consumption seems to be the most prevalent public health issue encountered by university students and males.
Hazardous alcohol consumption, defined as the regular average consumption of 20 - 40 g of alcohol a day for women and 40 - 60 g a day for men,[1]remains a major problem in low- and middle-income countries (LMICs) and is a major contributor to the burden of disease. Hazardous alcohol consumption presents a serious threat to the health and wellbeing of all people and is causally linked to chronic and acute health problems, in particular cancer, cardiovascular diseases, digestive tract conditions, accidents and violence, [2]as well as infectious diseases such as HIV and AIDS, hepatitis A and tuberculosis.[3,4]
The most recent Global Burden of Disease Study[5] estimated alcohol to be the seventh leading risk factor in 2016 in terms of disability-adjusted life-years (DALYs). Alcohol use was estimated to have caused approximately 99.2 million DALYs (95% confidence interval (CI) 88.3 - 111.2 million), accounting for 4.2% (95% CI 3.7 -4.6) of total DALYs, a larger share of total burden than previously reported.[5] In sub-Saharan Africa alone, alcohol was responsible for 6.4% of all deaths and 4.7% of all DALYs lost in 2012.[6]This represents a higher number of deaths and DALYs than previously reported by the World Health Organization (WHO) (3.3% of all deaths and 2.4% of DALYs).[7] South Africa (SA) has very high rates of hazardous alcohol consumption among drinkers, with rates of hazardous drinking appearing to be on the rise.[8] For example, in a cross-sectional analysis, researchers found an increase in the proportion of drinkers reporting binge drinking, an indicator of hazardous alcohol consumption, from 9.8% in 2005 to 13.2% in 2012.[9]
Together, these findings highlight the need for interventions to prevent transitions from non-hazardous alcohol use to hazardous patterns of consumption, and from hazardous alcohol use to the more severe form of alcohol use disorders (AUDs). In order to identify population-specific points of intervention for preventing progression to more harmful levels of use, context-specific information on the aetiology and the progression and remission trajectories of AUDs is needed. [7] There has been some research in this area that has focused on understanding the transition from use to dependence[7] or abuse to dependence,[10] but this has almost always been conducted in high-income settings with vulnerable population subgroups[11,12] rather than in the general population. There is a dearth of research emanating from LMICs, where socioeconomic contexts differ from those of high-income countries and where the alcohol environment is changing and increases in the alcohol-attributable burden of disease are inevitable.[6]
Although several SA studies have provided population- and community-level data on patterns of alcohol consumption,[13,15] these studies have not reported on the progression from non-problematic alcohol use to AUDs or the impact that cohort alcohol use has on transitioning through stages of alcohol use and AUDs. Estimating the risk and correlates of transitioning from alcohol use to dependence in this context will not only contribute to existing literature on the trajectories of use but will also provide information about the aetiology and the trajectories of alcohol use in SA. This is of importance, given the high levels of heavy episodic drinking among drinkers in SA[7] and the need to identify interventions that could work towards addressing or alleviating the burden.
Objectives
This study attempted to address this gap by analysing data from the South African Stress and Health Survey, collected as part of the WHO'S World Mental Health Survey Initiative. While previous publications from this initiative have addressed the prevalence of AUDs,[10,11] we aimed to estimate the prevalence of use, regular use, AUDs and remission from AUDs in the SA population. A further objective was to investigate whether age of onset, education, sex and level of cohort alcohol use are associated with commencement of alcohol use, regularity of use, and transitions to and remission from more harmful levels of use.
Methods
Sample
The South African Stress and Health Survey recruited a nationally representative sample of 4 315 individuals aged >18 years. As reported in an earlier article,[10] the study was a multistage, random area probability sample of adults resident in SA. Sampled residences were stratified into 10 diverse housing categories. Within each of these strata, 600 households were listed from maps, census data or aerial photographs. A probability sample of households was selected and screened to determine eligibility. A single adult respondent from each selected dwelling was drawn randomly using the Kish method Surveys were administered by trained field interviewers, in person and in the home language of the participant during prescheduled appointments. As reported on in an earlier article, [12]field interviewers made up to three attempts to contact each respondent, and the overall response rate was 85.5%.
All recruitment, consent and field procedures were approved by the human subjects committees of the University of Michigan and Harvard Medical School. A single project assurance of compliance was obtained from the Medical University of South Africa (ethics ref. no. #S-017210-01), which was also approved by the National Institute of Mental Health.
Excluding four respondents who did not provide any response to alcohol use questions, the total sample included 4 311 respondents with an overall response rate of 87.1%.
Assessment of alcohol use and use disorders
Data were collected using the World Mental Health Survey Initiative version of the Composite International Diagnostic Interview version 3.0 (WMH-CIDI 3.0).[13] This interview has been used in household surveys in at least 28 countries including SA, and has undergone extensive methodological development and testing. The instrument collects diagnostic information on a broad range of mental disorders and information on risk factors, impact, patterns and treatment of mental disorders.
The WMH-CIDI produces diagnostic information according to the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV).[14]Diagnoses were derived using standard WMH-CIDI diagnostic algorithms and lifetime DSM-IV diagnoses are used in the current report.
Age of onset and speed of transition between stages of alcohol use were evaluated. These stages were 'use' (first time drinking a standard alcoholic drink), 'regular use' (first time consuming 12 or more drinks in a year), DSM-IV abuse without prior dependence and DSM-IV dependence. We also assessed remission from dependence and from abuse without dependence, where remission was defined as the absence of all disorder-related symptoms for >12 months prior to the interview.
To minimise respondent burden, questions regarding AUDs were asked of all respondents who, in the year they drank most, drank alcohol on at least one day per week, or at least three standard (10 g) alcoholic drinks per drinking day. Alcohol dependence questions were only asked of persons with a history of alcohol abuse. However as abuse and dependence are independent diagnoses, this leads to an underestimation of dependence. In an effort to address this issue, dependence cases were imputed among non-abusing lifetime users; the details of the methodology of this imputation are presented elsewhere.[15]
Data analysis
All analyses were carried out using SAS version 9.4 (SAS Institute, USA). Estimates of lifetime prevalence came from PROC SURVEYFREQ and discrete-time models from PROC SURVEYLOGISTIC, both of which account for the complex survey design, including weighting, clustering and stratification. Life-table (actuarial) estimates of the survival functions for age of onset and remission were produced using the SAS PROC LIFETEST procedure and are reported as weighted prevalence.
Discrete-time survival models were used to investigate the association of cohort use with transitions between stages of alcohol involvement, with person-year as the unit of analysis and a logistic link function. We defined the cohort use variable to represent, at any given age, the level of alcohol use in an individual's birth and sex cohort. An individual's birth cohort was based on their year of birth ±5 years, which created 11-year wide cohorts by sex, centered on year of birth. The cohort widths were reduced for those aged <22 years at age of interview to as closely as possible ensure symmetry around birth year while maintaining an arbitrary minimum of 50 respondents in each sex-specific cohort. Cohorts were top-coded from age >65. The cohort use variable modelled the estimated proportion of people (/10) in the individual's birth and sex cohort who had used alcohol by the prior person-year. Linearity of the log-odds of the cohort use variable were investigated.
Other covariates included in these models were sex, time-varying educational level (student, low, low/medium, medium/high or high) and person-year age groupings (use, regular use and use disorder transitions used <14, 15 - 17, 18 - 20, 21 -24, 25 -29 and >30 categories; remission models used ¿18, 19 - 20, 21 - 22, 23 - 24, 25 - 29, 30 - 39 and >40 categories). Age of commencing alcohol use was included in all models except transition to commencing use and was defined as early (< 17 years), mid (18 - 20 years) or late (>21 years) tertiles. The remission from alcohol abuse model also adjusted for years since onset of abuse and speed to transition from use to abuse, defined as early (0 - 2 years), mid (3 - 6 years) or late (>7 years) tertiles. Odds ratios (ORs) and 95% confidence intervals (CIs) are presented and significance tests are evaluated using 0.05-level two-sided tests.
Results
Prevalence of alcohol stages
Of the total sample, 40.6% (95% CI 38.3 -42.9) of respondents indicated having used alcohol in their lifetime, 35.3% (95% CI 33.2 - 37.5) reported using alcohol regularly, and 8.8% (95% CI 7.4 - 10.1) met diagnostic criteria for alcohol abuse and 2.7% (95% CI 2.0 - 3.5) diagnostic criteria for alcohol dependence.
Among lifetime users, a large proportion reported having used alcohol regularly at some point (87%; 95% CI 85.3 - 88.7), one in five (21.6%; 95% CI 18.8 - 24.4) met diagnostic criteria for lifetime alcohol abuse, and a smaller proportion (6.7%; CI 5.0 -8.5) met criteria for lifetime dependence. The prevalence of remission among lifetime abuse without dependence cases was 55.9% (95% CI 49.0 - 62.7) Additionally, 52.8% (95% CI 39.5 - 66.1) of respondents with lifetime alcohol dependence reported having remitted by the time of the survey.
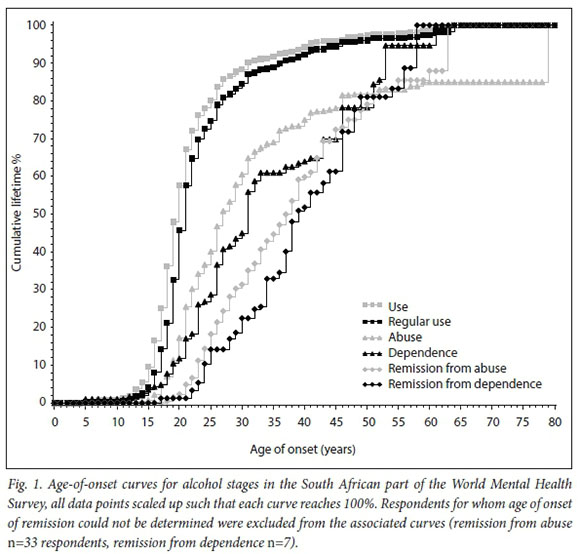
Age of onset distributions
Fig. 1 shows the cumulative age-of-onset curves for alcohol use, regular use, abuse and dependence as well as remission from abuse and dependence. Onset of use and regular use were closely aligned, with the median age of onset of use at 20 years and that of regular use at 21 years. Onset of abuse and dependence occurred at a later life stage, median ages being 27 years and 31 years, respectively. Remission largely occurred (75th percentile) by age 47 for abuse and age 48 for dependence.
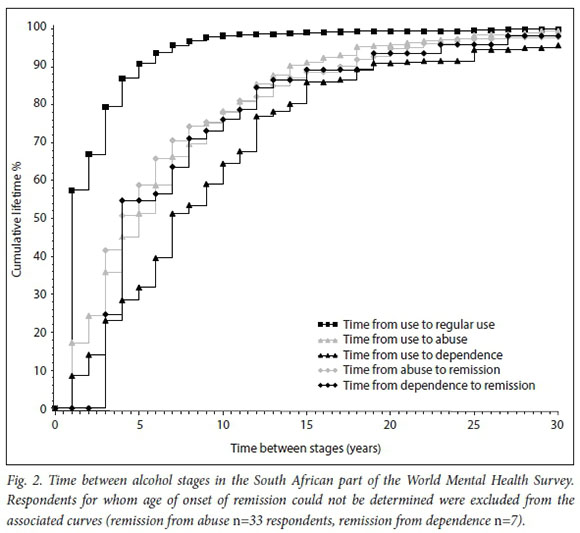
Time to transition across stages of alcohol use
Fig. 2 shows the cumulative curves of time for transitioning between stages of alcohol use. Onset of regular alcohol use largely occurred (75th percentile) within 2 - 3 years of first use; in fact, within a year of first using alcohol, more than half of users transitioned to regular use. Almost a quarter (24.3%) of alcohol abuse cases developed within 2 years of first alcohol use, while it took twice as long (4 years) for the same proportion of dependence cases to develop. Time to remission was similar between abuse and dependence cases, with more than half of all remission cases transitioning out of the disorder doing so within 4 years of its onset.
Associations between covariates and transitions between alcohol stages
Table 1 summarises the multivariate results from investigating associations between covariates and transitions of involvement with alcohol. The transitions considered include from abstinence to first-ever use; from use to regular use, use to abuse, and use to dependence; and from regular use to both abuse and dependence. The findings suggest that the odds of men transitioning were significantly greater than for women, both in commencing use (OR 2.58, 95% CI 2.13 - 3.14) and transitioning from use to regular use (OR 1.35, 95% CI 1.04 - 1.77). Cohort use was also found to be significantly associated with these transitions such that, for every 10% increase of people in any age-sex cohort having commenced use by the previous person-year, there was a 12% and 14% increase in the adjusted odds of commencing use (OR 1.12, 95% CI 1.03 - 1.22) and transitioning to regular use (OR 1.14, 95% CI 1.01 - 1.29), respectively.
With regard to educational level, compared with respondents who had attained a high level of education, higher odds of transitioning were observed among students for commencing use (OR 1.68, 95% CI 1.17 -2.41), and among persons with a low level of education for transitioning from use to regular use (OR 1.77, 95% CI 1.04-3.01).
The results further suggest that an individual's age of commencing use was significantly associated with transitions from use to regular use, where those who had commenced alcohol use later in life (>21 years) were at higher odds of transitioning to regular drinking compared with those who had commenced use earlier. We observed no significant associations of gender, cohort use, education or age of onset of use with transitions from use to use disorders, or from regular use to use disorders.
Table 2 shows the results from investigating associations of covariates with remission from alcohol abuse without dependence. Gender was significantly associated with remission from abuse, such that men were less likely than women to remit (OR 0.20, 95% CI 0.06 - 0.71). With regard to cohort use, the results suggest that with every 10% increase in prevalence of use among an individual's age-sex cohort, the odds of remitting from alcohol abuse increase by 64% in the subsequent person-year (OR 1.64; p=0.007). No other significant findings emerged from the analysis. An insufficient number of cases meant that the transition to remission from dependence could not be investigated.
Discussion
To our knowledge, this is the first study to examine the transition from alcohol use to dependence. While the study also sought to examine remission from alcohol-related disorders, data were limited in that remission from dependence could not be investigated, but remission from alcohol abuse without dependence is presented. Nonetheless, this study contributes to estimating the prevalence of AUDs and rates of remission from alcohol abuse without dependence. Furthermore, it provides useful insights into some of the sociodemographic and contextual factors associated with transition to and from more harmful levels of use.
Overall, lifetime use of alcohol among South Africans was 40.6%, which is in keeping with findings from the most recent South African Demographic and Health Survey.[16]Our findings that 21.7% of users in the sample met criteria for abuse and 6.7% met criteria for dependence are also in keeping with what we know about rates of abuse and dependence from other parts of the world. [17]While only a small proportion of individuals who use addictive substances develop dependence,[17] the burden associated with alcohol abuse and dependence should not be underestimated. Concerted efforts are needed to ensure that people at risk of transitioning to more harmful levels of alcohol use are identified and provided with interventions to prevent this transition.
Our results suggest several potential targets for interventions to prevent transition to harmful levels of alcohol use. First, in this nationally representative sample, participants generally started drinking regularly in their early 20s, with a smaller proportion starting during adolescence. This finding is in keeping with studies from other countries that also reported that regular alcohol use often begins in the early to mid-20s.[17,18]Our finding of quick transitions from use to regular use (the majority within 2 years of initial use) suggests that interventions to delay the initiation of alcohol use further and prevent transition to problematic alcohol consumption should target younger age cohorts. Evidence suggests that these interventions should be multi-pronged and include community-based efforts[19] to limit alcohol sales to minors, enforce underage drinking laws and stop advertising campaigns targeting young people, together with family, school and university prevention initiatives and referral to alcohol risk-reduction interventions if indicated.[6,20,21]Our findings that cohort alcohol use was associated with transition to commencement of use and transition from use to regular use suggest that peer influences from direct associations such as friends and family may be instrumental in the onset of use and subsequent transitioning and are therefore an important target for these prevention programmes.
We further found that transitioning from regular alcohol use to alcohol abuse and from abuse to alcohol dependence occurs later in life, generally in the late 40s. As our findings show, it takes people an average of 5 years to transition from regular use to abuse and 7 years to transition from use to dependence. This is not surprising given findings from other studies that transitioning from use to dependence takes longer for alcohol than for other drugs.[22,23]In addition, local studies have shown that patients receiving treatment for alcohol abuse or dependence are substantially older than individuals who have other primary substances of abuse.[24] Given the length of time it takes people to transition to more harmful levels of alcohol use, there is a sizeable window of opportunity to identify regular users of alcohol via screening and provide them with brief interventions to help them reduce their risk of progressing to abuse or dependence. There is a large body of evidence[25] to support the effectiveness of screening, brief interventions and referral to treatment (SBIRT) for alcohol-related problems, with these interventions being suitable for a range of settings such as emergency room settings,[26] workplace settings[27] and primary healthcare settings.[28]
In keeping with previous findings,[16,29] our results suggest that being male and being a student were associated with the onset of alcohol use. This is of concern, since a systematic review conducted in 2016 confirms that hazardous alcohol consumption continues to be the most prevalent public health issue encountered by university students.[30] Consequently, this highlights the need for interventions among university students given that excessive alcohol consumption during young adulthood is associated not only with an increased risk of alcohol-related problems in adulthood, but also with lower academic achievement,[30,31] unsafe sex[31,32] and injury.[33] It istherefore evident that there is a need for prevention strategies that focus on beliefs and expectations among university students about alcohol[32] to further enable university institutions to implement evidence-based interventions that target risky drinking practices. It is also evident that men are less likely to remit from abuse of alcohol.
This is similar to studies conducted by Lopez-Quintero et al [34] They ascribe this finding to women experiencing worse physical, mental and social consequences of substance use, including alcohol, than men, which may lead to increased motivation to stop using.[34] Research conducted by Khan et al.[35] found that men were more likely to remit later in life, while women remitted at slightly younger ages. The researchers attributed this to the fact that women who use alcohol heavily may experience more psychosocial consequences of their heavy use, such as marital problems or emotional problems, that prompt earlier remittance.
In addition, we noted higher odds of transitioning from use to regular use for persons with low educational attainment. A study by Crum et al.[36] found that the risk of alcohol disorders was greater for those who dropped out of high school. Similarly, other studies have found poor educational attainment[37] and dropping out of school[38] to be significant predictors for alcohol use. Attention should be focused on identifying such groups that are at increased risk of developing alcohol-related problems, particularly in the SA context, where most young people are socially disadvantaged and poor, thus compounding the problem.
Study limitations
While this study provides useful insights, it should be interpreted with caution, considering limitations common to most large-scale surveys. First, information on use of alcohol was based on self-report data, which may have resulted in some under- or over-reporting. Second, the data are cross-sectional and while the modelling conducted takes into account the time-varying nature of certain variables, we cannot attribute relationships as direct causal pathways. The study may also be subject to recall bias, since the longer the time interval between the event and assessment, the higher the probability of incorrect recall. Additionally, the rates of remission reported in this study are surprisingly high. Further research to confirm these findings and determine all factors or drivers associated with remission is therefore encouraged. It may also be worthwhile to examine transition patterns on other more recent data sources from SA, such as data from the South African Demographic and Health Survey
Conclusions
Our findings suggest that cohort alcohol use is associated with transition to commencement of use and from use to regular use in the general SA population. As such, it contributes to estimating the prevalence of AUDs and rates of remission from these disorders. The study further highlighted the need for interventions among males and university students given that excessive alcohol consumption during young adulthood and peer influence may be an important target for these prevention programmes. While the study highlights the importance of early interventions such as screening, brief intervention, and referral to treatment (SBIRT) interventions,[26] further research examining rates of remission reported in this study is encouraged.
Declaration. None.
Acknowledgements. The WMH Survey (South African part) was carried out in conjunction with the WHO World Mental Health Survey Initiative supported bythe National Institute of Mental Health (ROI MH070884), the lohn D and Catherine T MacArthur Foundation, the Pfizer Foundation the US Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical Inc., GlaxoSmithKline and Bristol-Myers Squibb. We thank the staff of the WMH Data Collection and Data Analysis Coordination centres for assistance with instrumentation and fieldwork, and consultation on data analysis. None of the funders had any role in the design of the study, analysis, interpretation of results or preparation of this article. A complete list of all within-country and cross-national WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/
Author contributions. NHB and BM contributed to the writing of the article. DJS and DRW were involved in the study design and study implementation and contributed to the writing of the article. CB analysed all the data from this study.
Funding. The SA authors NHB, BM and DJS are supported by the South African Medical Research Council. The analysis work was supported by an Australian National Health and Medical Research Council project grant (no. 1081984). This study was supported by grant MH59575 from the National Institute of Mental Health and the National Institute of Drug Abuse.
Conflicts of interest. None.
References
1. Babor TF, Longabaugh R, Zweben A, et ab Issues In the definition and measurement of drinking outcomes In alcoholism treatment research. J Stud Alcohol Suppl 19943uppl 12-.101-111. https://doi.org/10.15288/jsas.l994.sl2.101 [ Links ]
2. Parry CD, Patra J, Rehm J. Alcohol consumption and non-communicable diseases. Epidemiology and policy implications. Addiction 2011,106(10).1718-1724. https://doi.org/10.1111/j.l360-0443.2011.03605.x [ Links ]
3. Schneider M, Norman R, Parry C, Bradshaw D, Pluddemann A, South African Comparative Risk Assessment Collaborating Group. Estimating the burden of disease attributable to alcohol use in South Africa in 2000. S Afr Med J 2007;97(8 Pt 2):664-672. [ Links ]
4. Ferreira-Borges C, Rehm J, Dias S, Babor T, Parry CD. The impact of alcohol consumption on African people in 2012. An analysis of burden of disease. Trop Med Int Health 2016,21(1).52-60. http://doi.org/10.1111/tmi.l2618 [ Links ]
5. GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990 - 2016? A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017,390(10100).1345-1422. https://doi.org/10.1016/S0140-6736(17)32366-8 [ Links ]
6. Ferreira-Borges C, Dias S, Babor T, Esser MB, Parry CD. Alcohol and public health in Africa. Can we prevent alcohol-related harm from increasing? Addiction 2015,110(9).1373-1379. https://doi.org/10.1111/add.12916 [ Links ]
7. World Health Organization. Global Status Report on Alcohol and Health. Geneva. WHO, 2014. [ Links ]
8. Ferreira-Borges C, Parry C, Babor T. Harmful use of alcohol. A shadow over sub-Saharan Africa in need of workable solutions. Int J Environ Res Public Health 2017,14(4).346-358. https://doi.org/10.3390/ijerph14040346 [ Links ]
9. Probst C, Simbayi L, Parry C, Shuper P, Rehm J. Alcohol use, socioeconomic status and risk of HTV infections. AIDS Behav 2017,21(7).1926-1937. https://doi.org/10.1007/sl0461-017-1758-x [ Links ]
10. Williams D, Herman A, Kessler R, et al. The South Africa Stress and Health Study. Rationale and design. Metab BrainDis 2004,19(1/2).135-147. https://doi.org/10.1023/B.MEBR.0000027424.86587.74 [ Links ]
11. Williams DR Herman A, Stein DJ, et al. Twelve-month mental disorders in South Africa. Prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychol Med 2008,38(2).211-220. https://doi.org/10.1017/S0033291707001420 [ Links ]
12. Gass JD, Stein DJ, Williams DR, Seedat S. Intimate partner violence, health behaviours, and chronic physical illness among South African women. S Afr Med J 2010,100(9).582-585. [ Links ]
13. Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13(2):93-121. [ Links ]
14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. -Technical Revision. Washington, DC APA, 2000. [ Links ]
15. Lago L, Glantz MD, Kessler RC, et al. Substance dependence among those without symptoms of substance abuse in the World Mental Health Survey. Int J Methods Psychiatr Res 2017,26(3). https://doi.org/10.1002/mpr.1557 [ Links ]
16. Statistics South Africa. South African Demographic and Health Survey 2016. Key Indicators. Pretoria South Africa, and Rockville, MD, USA, 2017. [ Links ]
17. Lopez-Quintero C, de los Cobos JP, Hasin DS, et al. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine. Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend 2011,115(1-2).120-130. https://doi.org/10.1016/j.drugalcdep.2010.11.004 [ Links ]
18. Schuckit MA. Alcohol-use disorders. Lancet 2009,373(9662).492-501. https://doi.org/10.1016/S0140-6736(09)60009-X [ Links ]
19. Fagan AA, Hawkins JD, Catalano RF. Engaging communities to prevent underage drinking Alcohol Res Health 2011,34(2).167-174. [ Links ]
20. Parry C, Harker Burnhams N, London L. A total ban on alcohol advertising. Presenting the public health case. S Afr Med J 2012,102(7).602-604. [ Links ]
21. Paschall MJ, Antin T, Ringwalt CL, Saltz RF. Effects of AlcoholEdu for college on alcohol-related problems among freshme« A randomized multicampus trial J Stud Alcohol Drugs 2011,72(4):642-650. [ Links ]
22. Anthony J, Warner L, Kessler R Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants. Basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol 1994,2(3).244-268. http://psycnet.apa.org/doi/10.1037/1064-1297.2.3.244 [ Links ]
23. Behrendt S, Wittchen H, Hofler M, Lieb R Beesdo K. Transitions from first substance use to substance use disorders in adolescence. Is early onset associated with a rapid escalation? Drug Alcohol Depend 2009-,99(1-3).68-78. https://doi.org/10.1016/j.drugalcdep.2008.06.014 [ Links ]
24. Dada S, Harker Burnhams N, Erasmus J, et al. Monitoring alcohol, tobacco and other drug use trends in South Africa. July 1996 - December 2016. SACENDU. Update 2017. http://www.mrc.ac.za/sites/default/files/attachments/2017-07-27/SACENDUupdatejUNE2017.pdf (accessed 26 November 2018). [ Links ]
25. Reho K, Agley J, DeSalle M, Gassman RA. Are we there yet? A review of screening, brief intervention, and referral to treatment (SBIRT) implementation fidelity tools and proficiency checklists. J Prim Prev 2016-,37(4).377-388. https://doi.org/10.1007/sl0935-016-0431-x [ Links ]
26. Myers B, Stein DJ, Mtukushe B, Sorsdahl K. Feasibility and acceptability of screening and brief interventions to address alcohol and other drug use among patients presenting for emergency services in Cape Town, South Africa. Adv Prev Med 2012,2012.569153. https://doi.org/10.1155/2012/569153 [ Links ]
27. Harker Burnhams N, Parry C. Ble state of interventions to address substance-related disorders in South African workplaces. Implications for research, policy, and practice. S Afr J Psychol 2015p45(4).l-13. https://doi.org/10.1177%2F0081246315583792 [ Links ]
28. Babor TE, Higgins-Biddle J, Dauser D, Higgins P, Burleson JA. Alcohol screening and brief intervention in primary care settings. Implementation models and predictors. J Stud Alcohol 2005,66(3>361-368. https://doi.org/10.15288/jsa.2005.66.361 [ Links ]
29. Bello B, Moultrie H, Somji A, Chersich MF, Watts C, Delany-Moretlwe S. Alcohol use and sexual risk behaviour among men and women in inner-city Johannesburg, South Africa. BMC Public Health 2017,17(Suppl 3):548. https://doi.org/10.1186/sl2889-017-4350-4 [ Links ]
30. Mota N, Alvarez-Gil R, Corral M, et al. Risky alcohol use and heavy episodic drinking among Spanish university students. A two-year follow-up. Gac Sanit 2010;24(5>.372-377. https://doi.org/10.1016/j.gaceta.2010.02.013 [ Links ]
31. Du Preez R, Pentz C, Lategan B. Why students drink A study of South African university students drinking behaviour. S Afr J Higher Educ 2016-,30(2).73-93. https://doi.org/10.20853/30-2-582 [ Links ]
32. Moure-Rodriguez L, Pineiro M, Corral Varela M, Rodriguez-Holguin S, Cadaveira F, Caamano-Isorna E Identifying predictors and prevalence of alcohol consumption among university students-. Nine years offollow-up. PLoS One 2016Ul(ll).e0165514. https://doi.org/10.1371/journal.pone.0165514 [ Links ]
33. Caamano-Isorna F, Moure-Rodriguez L, Doallo S, Corral M, Rodriguez Holguin S, Cadaveira E Heavy episodic drinking and alcohol-related injuries. An open cohort study among college students. Accid Anal Prev 2017,100.23-29. https://doi.org/10.1016/j.aap.2016.12.012 [ Links ]
34. Lopez-Quintero C, Hasin DS, de Los Cobos JP, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction 2011,106(3).657-669. https://doi.org/10.1111/J.1360-0443.2010.03194.X [ Links ]
35. Khan S, Okuda M, Hasin DS, et al. Gender differences in lifetime alcohol dependence. Results from the national epidemiologic survey on alcohol and related conditions. Alcohol Clin Exp Res 2013,37(10>.1696-1705. https://doi.org/10.1111/acer.l2158 [ Links ]
36. Crum RM, Anthony JC Educational level and risk for alcohol abuse and dependence. Differences by race-ethnicity. Ethn Dis 2000,10(1).39-52. [ Links ]
37. Brook JS, Morojele NK, Pähl K, Brook DW Predictors of drug use among South African adolescents. J Adolesc Health 2006,38(1).26-34. https://doi.org/10.1016/j.jadohealth.2004.08.004 [ Links ]
38. Townsend L, Flisher AJ, King G. A systematic review of the relationship between high school dropout and substance use. Clin Child Fam Psychol Rev 2007,10(4).295-317. https://doi.org/10.1007/sl0567-007-0023-7 [ Links ]
 Correspondence:
Correspondence:
N Harker Burnhams
nadine.harker&mrc.ac.za
Accepted 11 June 2018














