Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 n.11 Pretoria Nov. 2018
http://dx.doi.org/10.7196/samj.2018.v108i11.12966
RESEARCH
An evaluation of the quality of discharge summaries from the general paediatric wards at Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
S SinghI; F SolomonII, III; S A MadhiIV, V; Z DangorVI, VII, VIII; S G LalaIX, X
IMMed (Paediatrics); Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMFamMed; Medical Research Council Respiratory and Meningeal Pathogens Research Unit, Faculty of Health Sciences, University of the Witwatersrand Johannesburg, South Africa
IIIMFamMed; Department of Science and Technology/National Research Foundation: Vaccine Preventable Diseases, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVPhD; Medical Research Council Respiratory and Meningeal Pathogens Research Unit, Faculty of Health Sciences, University of the Witwatersrand Johannesburg, South Africa
VPhD; Department of Science and Technology/National Research Foundation: Vaccine Preventable Diseases, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIPhD; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIIPhD; Medical Research Council Respiratory and Meningeal Pathogens Research Unit, Faculty of Health Sciences, University of the Witwatersrand Johannesburg, South Africa
VIIIPhD; Department of Science and Technology/National Research Foundation: Vaccine Preventable Diseases, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IXPhD; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
XPhD; Perinatal HIV Research Unit, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Hospital discharge summaries are deemed to be an essential part of the medical record in South Africa, but formal assessment of their quality is rarely undertaken. At Chris Hani Baragwanath Academic Hospital (CHBAH) in Johannesburg, medical admission notes (bedletters) are difficult to retrieve from the hospital archives and the discharge summary is often the only readily available medical record that documents details of the hospital admission.
OBJECTIVES. To determine the proportion of discharge summaries that were appropriately completed for children admitted to the general paediatric wards at CHBAH.
METHODS. A retrospective review of discharge summaries completed for children admitted from 1 May to 31 July 2016 was undertaken. The completeness of the following demographic and clinical variables was assessed: patient identifiers, hospital outcome, HIV infection status and anthropometric status. The documentation of correct International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) codes was assessed in children diagnosed with any form of lower respiratory tract infection (LRTI), which is the commonest diagnosis recorded in hospitalised children at CHBAH.
RESULTS. Discharge summaries were available for 1 148 (78.3%) of 1 466 children admitted during the study period. For completed discharge summaries, 80.1 - 93.3% of patient identifiers and 91.4% of patient outcomes were appropriately completed. HIV exposure was documented in 84.7% of summaries. Anthropometric parameters, including weight and length/height at admission and discharge weight, were appropriately completed in 91.4%, 70.9% and 50.0% of summaries, respectively. The ICD-10 code for children with LRTI was appropriately recorded by medical staff in 338 (67.2%) of 503 cases. ICD-10 codes and anthropometric parameters, which are important clinical parameters in the paediatric follow-up consultation, were both correctly recorded for only 21.6% of children who required follow-up clinical consultations at CHBAH.
CONCLUSIONS. Compared with similar studies, both the rate of completion and the quality of completed discharge summaries were modest in this tertiary academic teaching hospital. As discharge summaries are crucial medical documents, interventions to improve their completeness rate and quality need to be developed.
The discharge summary is an important but often overlooked medical document containing vital information pertaining to the patient's most recent stay in hospital. Various medical authorities emphasise the importance of good-quality discharge summaries.[1,3] The discharge summary is regarded as 'an essential component of the health record' by the Health Professions Council of South Africa.[4] Although there is no universally accepted discharge summary format, the most crucial components of the discharge summary are the discharge diagnosis, treatment received in hospital, results of investigations, follow-up visits, and further management plans envisaged.[5] In paediatrics, accurate anthropometric data are also recorded on the discharge summary because growth monitoring is frequently used to monitor response to an illness or disease.[6]
The availability of a discharge summary, with adequately recorded information, has demonstrable direct benefit for the patient. A recent study conducted in the USA showed that interventions to improve the discharge summary quality directly contributed to faster recovery rates and lower hospital readmission rates for cardiacfailurepatients.[7]
In South Africa (SA), the discharge summary document is of vital importance to patients and healthcare workers (both at the admitting hospital and associated referral clinics or hospitals) because it is often the only detailed record of a hospital admission. Notwithstanding the fact that the Department of Paediatrics at Chris Hani Baragwanath Academic Hospital (CHBAH) is one of the largest paediatric facilities in Africa, paediatric admission files are extremely difficult to retrieve from the CHBAH record archive, as is also the situation in many other clinical departments in SA state hospitals.[8-10]
Objectives
To determine the quality of discharge summaries that were completed for general paediatric admissions at CHBAH.
Methods
A retrospective review of discharge summaries completed for children admitted to the general paediatric wards from 1 May to 31 July 2016 was undertaken. In the Department of Paediatrics at CHBAH, each discharge summary is completed by hand, in triplicate, using a carbon-paper pro forma template; one copy of the summary is filed in the patient-retained outpatient file and the second in the hospital archive, while the third is sent for capture into an electronic database maintained by the Respiratory and Meningeal Pathogens Research Unit (RMPRU). The summaries are most often completed by interns, and occasionally by medical students, medical officers and registrars. The paper-based discharge summary was designed by clinicians to capture clinical information pertinent to this setting.
Through active monitoring of the ward admission registers maintained by the nursing staff, the RMPRU is able to track all admissions to the general paediatric wards. Discharge summaries collected by RMPRU staff are then cross-checked with the ward admission registers, which record the name of the patient and his or her age, gender, hospital number, date of admission, and date of discharge or death. This allows for missing, inaccurate or unfinished summaries to be completed or corrected by the RMPRU staff. Two physicians at the RMPRU also verify the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) against the code written by the doctor on the discharge summary and the preliminary admission diagnosis written in the nursing admission register. This system provides an opportunity to assess whether information is appropriately recorded on the discharge summary form. For missing discharge summaries, the RMPRU staff extract available information from the admission registry, which includes the age of the child, diagnosis at time of admission and outcome of the hospitalisation. This allows for the electronic capture of all admissions to the general paediatric wards at CHBAH.
On discharge summaries completed by the hospital staff, we determined whether information was appropriately completed/ recorded in the following fields: (i) patient identifiers (first name, surname, gender, hospital number, and dates of birth, admission, and discharge or death); (ii) outcome of hospitalisation; (iii) details of doctor completing the summary (name, signature and date of completion of summary); (iv) HIV status (HIV exposure, and CD4+ and viral load results for infected children); (v) anthropometric status (admission weight and length/height, presence of nutritional oedema, and discharge weight); (vi) ICD-10 codes for children diagnosed with any form of lower respiratory tract infection (LRTI) (e.g. bronchopneumonia, bronchiolitis, lobar pneumonia, etc.); (.vit) follow-up requirement (at CHBAH and/or other health facility); and (viii) reasons for follow-up at CHBAH. Criteria used to deem a field appropriately completed were defined prior to the analysis. Briefly, for domains requiring alpha characters (for example, first name and surname), fields that were not filled in or were illegible or indecipherable (i.e. not clear enough to be read by at least two of three observers) were regarded as missing or incomplete. For domains requiring numerical characters (such as hospital numbers, dates and anthropometric measurements), fields that were not filled in or were illegible or indecipherable were regarded as missing or incomplete. Hospital numbers were regarded as incomplete if a single digit was missing and anthropometric measurements were regarded as incomplete if not recorded to the first decimal point. For ICD-10 codes, we deemed any code representative of any form of LRTI (generally codes from J09 to J22) to be appropriately recorded if the written diagnosis was compatible with any form of LRTI and verified by RMPRU physicians.
Data analysis
All the study variables, as defined in the data collection sheet, are categorical (or nominal) variables. Frequency distributions were reported for all the study objectives. Potential relationships between categorical variables were analysed using contingency tables (either Fisher's exact test or the X2 test).
Ethical clearance
The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand (ref. no. M160920).
Results
During the 3-month study period, the admission registers showed that 1 466 children were admitted to the general paediatric wards at CHBAH. Of these, 1 148 (78.3%) had a discharge summary available for entry into the database. This indicated that 21.7% of discharge summaries were either not completed or misfiled before capture into the database. We therefore determined whether information was appropriately recorded in 1 148 records (Table 1), i.e. summaries completed solely by the RMPRU staff were not analysed. For patient identifiers and outcomes, 80.0 - 93.3% and 91.4% of fields, respectively, were appropriately recorded by the doctor completing the discharge summary. It was rare for the doctor to leave the patient name and surname domains blank (0.1%), but indecipherable or illegible handwriting accounted for 8.4% of instances where the name domains were not appropriately recorded.
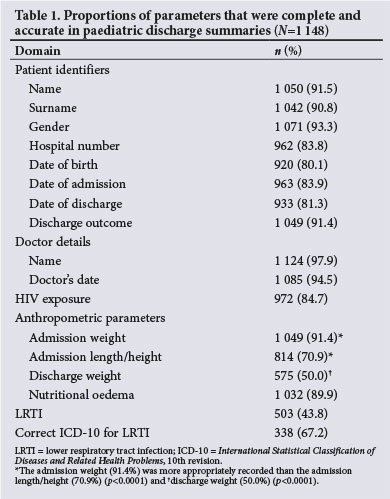
The HIV exposure of the admitted children was documented for 84.7% of cases, including 58 (5.4%) who were HIV-infected. Among HIV-infected children, 89.7% had CD4+ lymphocyte counts and 87.9% HIV viral load measurements completed. The anthropometric parameters were appropriately documented in 50.0 - 91.4% of summaries. The admission weight (91.4%) was more appropriately recorded than the admission length/height (70.9%) (p<0.0001) and discharge weight (50.0%) (p<0.0001). The ICD-10 code for children with LRTI was appropriately recorded in 338 of 503 cases (67.2%).
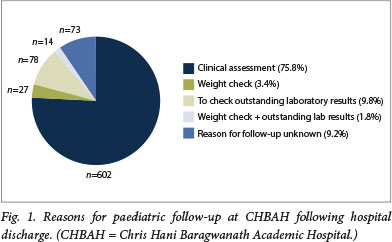
Requirement for follow-up (either at CHBAH or at another health facility) was appropriately completed for 1 065 (92.8%) of the 1 148 summaries. For the 794 children who required follow-up at CHBAH, the reason for follow-up was stated in 721 (90.1%) (Fig. 1). The main reasons for follow-up were clinical assessment (75.8%), evaluation of outstanding laboratory results (9.8%) and repeat anthropometric measurement (usually a check for weight gain) (5.2%).
We further compared the rates of appropriately completed discharge summary fields by month to determine whether discharge summary quality improved as interns spent more time in the Department of Paediatrics; the same group of interns was assessed during the study period. Although there were statistical differences in some parameters, we did not consider these to be of major clinical relevance because the quality of summaries did not consistently improve with time.
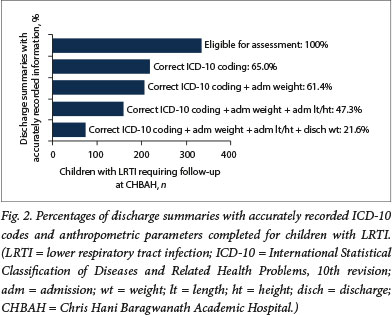
The effects of discharge summary quality on follow-up visits
For the 334 children with an LRTI diagnosis and who required further follow-up at CHBAH, we determined whether both their ICD-10 code and anthropometric fields (since these are critically important clinical parameters) were appropriately recorded on the summary. Incomplete or inappropriately recorded discharge weights (/1=178, 53.3%) and ICD-10 codes (n=117, 35.0%) were the commonest domains that were poorly recorded. Overall, only 72 (21.6%) of 334 children with LRTI had both ICD-10 codes and anthropometric parameters appropriately completed (Fig. 2).
Discussion
In the present study, we found that discharge summaries were only completed for approximately four of every five children admitted to the general paediatric wards at a national tertiary academic hospital. This is of concern, because discharge summaries are often the only record of a hospital admission that can be accessed readily. Furthermore, the rate of completed discharge summaries compares unfavourably with settings in Australia and the USA, [11,12] where >99% of discharge summaries are completed. To our knowledge, the completion rate of discharge summaries in SA state hospitals is not known, but the poor rate of retrieval of hospital records (-39% in district hospitals [8]) and acknowledgement of poor hospital record management systems [9,10] make it likely that missing discharge summaries are an important problem in SA.
Noting that section 10 of the National Health Act No. 61 of 2003 [13] states, in part, that All healthcare providers must supply patients with discharge reports. At the bare minimum these should contain the following information: the health service rendered, the patient's prognosis and the need for follow-up treatment,' we find that the completion rate of discharge summaries and the documentation of important medical information were much lower than desired. Based on findings from a prospective US-based study which showed that measures to improve the discharge summary quality resulted in lower hospital readmission rates,[7] we speculate that poorly completed discharge summaries compromise further clinical care and/or result in further unnecessary healthcare visits and/or costs in our setting.
Study limitations
A major limitation of the present study is that we were unable to verify the accuracy of the information in the discharge summary against a gold standard' because retrieval of archived hospital records at CHBAH (currently and at the time of the study) is very difficult. Nonetheless, we assessed the quality of the discharge summary because it is often the only readily available record of a hospital admission. We chose parameters such as patient identifiers and ICD-10 codes because the patient identifiers could be verified by checking against the nursing admission register and ICD-10 codes undergo verification at the RMPRU, which address some of the weaknesses of not having the admission notes available. Had we compared the contents of the discharge summary against the actual admission notes, it is likely that the percentage of discharge summaries containing appropriately recorded diagnostic information would be lower.
It is possible that completed discharge summaries were misfiled or lost before reaching the RMPRU database, but we believe that this is highly unlikely - the more probable explanation is that discharge summaries were not completed in the first instance. We speculate that the main reason for the relatively low rate of completion is that discharge summaries require timeous preparation: the intern needs to complete the summary by the time the child leaves the ward.[14] Factors that aggravate this situation - for example, when the discharge is performed in haste to lessen the pressure on occupied hospital beds (the study period coincided with the period when hospital admission rates were at their highest, and there is a relatively high patient load at CHBAH) - may have contributed to the low completion rates.[14]
Recommendations
There are several documented methods to improve discharge summary quality: educational training,[15,17]the use of electronically generated discharge summaries, [12] the provision of incentives, [18] and having more senior doctors complete the discharge summary.[5] The feasibility of using these methods to improve discharge summary quality should be assessed, not only for the patient's benefit [19] but also because good-quality discharge summaries contribute essential information that is used for public health system operations in SA. For example, ICD-10 codes require accurate recording because hospitals will require accurate diagnostic codes when purchasing services from the proposed National Health Authority (as envisaged in the proposed National Health Insurance).[20]
In SA state hospitals, we propose that improvement of discharge summary quality be prioritised as part of an urgent upgrade of hospital record systems because this is a feasible intervention that is likely to improve clinical care,[7] health system planning and research output. Consideration should therefore be given to establishing teams in the health facility that are dedicated to controlling the quality of the discharge summary and ensuring that ICD-10 coding is done in a standardised manner to provide more robust data.
Conclusions
In summary, although we cannot extrapolate our results to other institutions, the poor quality of completed discharge summaries is concerning; CHBAH is a central academic hospital, and it is likely that the quality of discharge summaries may be worse in other state hospitals. Discharge summary quality assessments should be carried out regularly, and further studies are needed to assess the effect of interventions to improve discharge summary quality and the impact of good-quality discharge summaries on patient health and health system functions in SA.
Declaration. This publication is a result of the work done by SS for her MMed degree in Paediatrics.
Acknowledgements. None.
Author contributions. Substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work: SS, FS, SAM, ZD, SGL; drafting the work: SS, SGL; revising the work critically for important intellectual content: FS, SAM, ZD; final approval of the version to be published: SS, FS, SAM, ZD, SGL.
Funding. SAM is funded in part by the Department of Science and Technology/National Research Foundation: South African Research Chair Initiative in Vaccine Preventable Diseases and the Medical Research Council of South Africa. Thefunders had no role in study design data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest. None
References
1. Snow V, Beck D, Budnitz T, et aL Transitions of Care Consensus Policy Statement. American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med 2009,4(6). 364-370. https://doi.org/10.1002/jhm.510 [ Links ]
2. Scottish Intercollegiate Guidelines Network (SIGN). The SIGN discharge document (SIGN publication no 128). Edinburgh. SIGN, June 2012. http://www.sign.ac.uk/assets/signl28.pdf (accessed 30 March 2017). [ Links ]
3. Health and Social Care Information Centre, Academy of Medical Royal Colleges. Standards for the clinical structure and content of patient records. 2013. http://www.aomrc.org.uk/reports-guidance/standards-for-the-clinical-structure-and-content-of-paUent-records-0713/ (accessed 30 March 2017). [ Links ]
4. Health Professions Council of South Africa. Guidelines for Good Practice in the Health Care Professions. Guidelines on the Keeping of Patient Records. Booklet 14. Pretoria. HPCSA, 2008 [ Links ]
5. Wimsett J, Harper A, Jones P. Review article. Components of a good quality discharge summary. A systematic review Emerg Med Australas 2014,26(5):430-438. http://doi.org/10.111/1742-6723.12285 [ Links ]
6. Schroeder DG, Brown KH. Nutritional status as a predictor of child survival. Summarizing the association and quantifying its global impact. Bull World Health Organ 1994,72(4):569-579. http://www.who.int/iris/handle/10665/53348 (accessed 8 October 2018). [ Links ]
7. Salim Al-Damluji M, Dzara K, Hodshon B, et al. Association of discharge summary quality with readmission risk for patients hospitalized with heart failure exacerbation. Circ Cardiovasc Qual Outcomes 2015,8(1).109-111. https://doi.org/10.1161/CIRCOUTCOMES.114.001476 [ Links ]
8. Wegner L, Rhoda A. Missing medical records. An obstacle to archival survey - research in a rural community in South Africa. S Afr J Physiother 2013:69(2).15-17. https://doi.org/10.4102/sajp.v6912.24 [ Links ]
9. Marutha NS, Ngoepe M. The role of medical records in the provision of public healthcare services in the Limpopo province of South Africa. S Afr J Inf Manage 2017,19(1).a873. http://doj.org/10.4102/sajim.v19il.873 [ Links ]
10. Katuu S. Managing records in South African public health care institutions. A critical analysis. PhD thesis. Pretoria. University of South Africa, 2015. http://uir.unisa.acza/handle/10500/19058 (accessed 2 October 2017). [ Links ]
11. Horwitz LI, Jenq GY, Brewster UC, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med 2013;8(8):436-443. https://doi.org/10.1002/jhm.2021 [ Links ]
12. Lehnbom EC, Raban MZ, Walter SR Richardson K, Westbrook JI. Do electronic discharge summaries contain more complete medication information? A retrospective analysis of paper versus electronic discharge summaries. HIM J 2014,43(3).4-12. https://doi.org/10.1177/183335831404300301 [ Links ]
13. South Africa. National Health Act No. 61 of 2003. https://wwwup.ac.2a/media/shared/12/ZP_Files/health-actzpl22778.pdf (accessed 30 March 2017). [ Links ]
14. Colt MH, Katz JT, McMahon GT. The effect of workload reduction on the quality of residents'discharge summaries. J Gen Intern Med 2011;26(1):28-32. https://doi.org/10.1007/s11606-010-1465-2 [ Links ]
15. Unnewehr M, Schaaf B, Marev R, Fitch J, Friederichs H. Optimj2jng the quality of hospital discharge summaries - a systematic review and practical tools. Postgrad Med 2015,127(6).630-639. https://doi.org/10.1080/00325481.2015.1054256 [ Links ]
16. Key-Solle M, Paulk E, Bradford K, Skinner AC, Lewis MC, Shomaker K. Improving the quality of discharge communication with an educational intervention. Pediatrics 2010,126(4).734-739. https://doi.org/10.1542/peds.2010-0884 [ Links ]
17. Axon RN, Penney FT, Kyle TR, et al. A hospital discharge summary quality improvement program featuring indivi dual and team-based feedback and academic detailing Am J Med Sei 2014,347(6):472-477. https://doi.org/10.1097/MAJ.0000000000000171 [ Links ]
18. Tan B, Mulo B, Skinner M. Discharge documentation improvement project. A pilot study Intern Med J 2015 s45(12).1280-1285. https://doi.org/10.1111/imj.12895 [ Links ]
19. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med 2003,138(3).161-167. https://doi.org/10.7326/0003-4819-138-3-200302040-00007 [ Links ]
20. Dyers RE, Evans J, Ward GA, du Plooy S, Mahomed H. Are central hospitals ready for National Health Insurance? ICD coding quality from an electronic patient discharge record for clinicians. S Afr Med J 2016-,106(2).181-185. https://doi.org/10.7196/SAMJ.2016.v106j2.10079 [ Links ]
 Correspondence:
Correspondence:
S G Lala
sanjay.lala@wits.ac.za
Accepted 16 May 2018














