Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 n.10 Pretoria Oct. 2018
http://dx.doi.org/10.7196/samj.2018.v108i10.13280
CME
Spontaneous liver haematoma rupture associated with pre-eclampsia in a low- to middle-income country: Lessons to be learnt from maternal death assessments
J MoodleyI; N C NgeneII
IMB ChB, FCOG (SA), FRCOG, MD; Women's Health and HIV Research Group, Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIMBBS, Dip Obst (SA), Dip HIV Man (SA), MMed (Fam Med), FCOG (SA), MMed (O&G); Women's Health and HIV Research Group, Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
Spontaneous rupture of liver haematoma is a complication of pre-eclampsia (PE) that results in maternal mortality, particularly in the absence of an early diagnosis and appropriate interventions. The aim was to describe cases of maternal deaths due to spontaneous rupture of liver haematoma associated with PE to raise awareness of clinical features suggestive of the diagnosis and to make recommendations regarding a team approach in managing this complication. Maternal deaths due to PE that occurred in health facilities in South Africa between 2014 and 2016 were reviewed and cases due to spontaneous rupture of liver haematoma were analysed. Eight maternal deaths occurred owing to spontaneous rupture of liver haematoma, and in 62.5% (5/8) the diagnosis was established at caesarean delivery. The common presenting features were upper abdominal pain, haemodynamic instability including collapse and haemoperitoneum associated with PE, and haemolysis, elevated liver enzymes and low platelet count (HELLP) syndrome. Substandard care was associated with all, except 1 patient, and the principal area of concern was inability to make the diagnosis and failure to seek advice from a referral centre. Preventable factors in these maternal deaths included adherence to clinical guidelines, appropriate clinical and laboratory assessment with regard to the diagnosis of spontaneous rupture of liver haematoma, and management by a multidisciplinary team.
Spontaneous hepatic rupture is a rare but catastrophic complication of pregnancy. This adverse event is usually associated with severe pre-eclampsia (PE) and/or with haemolysis, elevated liver enzymes and low platelet count (HELLP) syndrome. The incidence of liver haematoma rupture varies between 1/45 000 and 1/225 000 pregnancies, but carries significant maternal and fetal mortality and morbidity.[1-4] Maternal mortality is high, ranging from 17% to 59%, and depends on whether the haematoma is ruptured, rapidity of diagnosis and availability of therapeutic options.[1] This condition develops in PE when there are fibrin deposits in the liver vasculature that obstruct the sinusoids and lead to ischaemia, and subsequently to haemorrhage, haematoma and possibly hepatic rupture.[5]
The diagnosis of possible subcapsular haematoma of the liver is suspected on the basis symptoms, such as epigastric pain, right upper-quadrant abdominal pain and nausea and vomiting in patients with PE and/or HELLP syndrome.[3,4] In the haemodynamically stable patient with symptoms and signs (tenderness or mass in the liver area) suspicious of a haematoma, ultrasound and/or computed tomography (CT) imaging can be used to confirm the diagnosis.[4] The diagnosis may also be made by direct visualisation of free blood in the abdominal cavity and identification of the liver lesion at the time of caesarean delivery for severe PE. In a patient presenting with haemodynamic instability and acute abdominal pain, the diagnosis is usually made during an emergency laparotomy.[5]
The current report is an analysis of cases of maternal deaths due to spontaneous rupture of the liver associated with hypertensive disorders of pregnancy in South Africa (SA). Specific issues and details of such cases are usually not included in the triennial SA Saving Mothers Report, and even when included might not be highlighted. The aim of this study, therefore, was to describe cases of spontaneous hepatic rupture due to PE and/or HELLP syndrome to raise awareness of clinical features suspicious of liver rupture and to recommend a team (obstetrician, interventional radiologist and surgeon) approach to the management of such patients.
Methods
Permission was obtained from the National Department of Health to publish information from the analysis of data on maternal deaths by the National Committee on Confidential Enquiries into Maternal Deaths (NCCEMD). All institutional maternal deaths are reported to the NCCEMD, which arranges for a dyad of an obstetrician and a midwife not involved in the management to carry out an analysis of a maternal death to ascertain the primary cause of death. All cases of maternal deaths due to spontaneous rupture of the liver from PE and/ or HELLP syndrome between 2014 and 2016 were included in this study.
Results
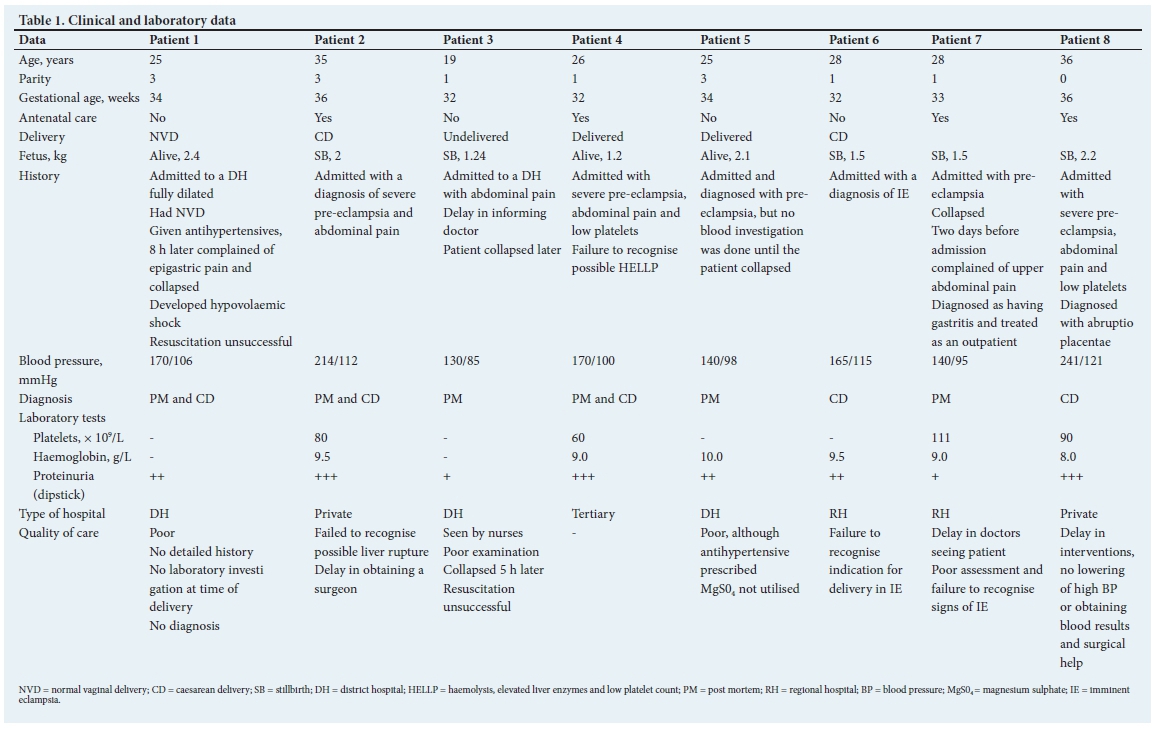
There were 8 maternal deaths, where independent assessors ascertained that the primary cause of death was rupture of a subcapsular liver haematoma. The diagnoses were confirmed at caesarean delivery, laparotomy or autopsy.[6] Table 1 shows the clinical and laboratory data of these 8 cases.
Discussion
This report of an analysis of 8 maternal deaths that were attributed to rupture of a liver haematoma reveals that all cases were associated with severe PE and most probably HELLP. This confirms previous findings that PE and HELLP are the underlying causes of liver rupture in pregnancy.[4,5] All patients in the current study had hypertension and proteinuria, again confirming previous reports.[4]
Our report is important because in certain cases, such as patient 1 (Table 1), health professionals providing initial care did not suspect liver rupture in a setting of complaints of epigastric pain, nausea and vomiting, and abdominal pain associated with PE. In another case (patient 7), the patient presented in the third trimester with epigastric pain and mild elevations of blood pressure and was treated for gastritis. Furthermore, standard blood investigations were not done or, if blood samples were sent to the laboratory, results were not obtained timeously. The maternity care clinical guidelines published by the National Department of Health,[7] and distributed to all hospitals in SA, strongly recommend that appropriate blood investigations for cases of hypertensive disorders of pregnancy (especially those with symptoms and signs suggestive of complications) should be performed at the time of diagnosis. Furthermore, the results of these investigations, including liver enzymes and platelet counts, should be retrieved and interpreted expeditiously. The findings of this report indicate that these guidelines were not followed in patients 1, 3 and 7 (Table 1), who collapsed after delivery; liver function investigations and full blood counts were not done or the results were not obtained in time. Although not all patients had severe hypertension on admission, close monitoring of blood pressure levels was not commenced, and 7 patients admitted to the district hospital and regional hospital were not seen immediately by a doctor. Blood pressure levels may fluctuate widely in pregnancy and in the immediate post-delivery period. It is therefore recommended that all patients with a diagnosis of severe PE must be monitored in a high-care bed or a bed specifically allocated for this emergency for at least 24 hours, and all appropriate observations and blood investigations must be carried out in good time. Such patients should immediately be attended to by experienced medical practitioners. Patients 1, 3 and 5 were managed in district hospitals and although they were admitted as emergency cases, actions taken by the admitting healthcare professionals were poor and delays in interventions occurred because doctors did not respond in time. It is vital that such patients are seen by medical doctors within 10 minutes and advice obtained from specialists regarding patient referral to higher levels of healthcare or their continuing management. Understandably, this recommendation may be challenging to put into practice, given that the attending doctor may be busy with another patient. Therefore, each health facility must have advanced plans on how to 'red flag' and respond to such an emergency. The SA maternity care guidelines clearly state that women with severe PE should have high blood pressure lowered judiciously and magnesium sulphate administered, and that such measures can be initiated by the first health responder, including professional nurses.
The current audit highlights that in patients with severe PE (patients 2, 4 and 8), who complain of epigastric pain (especially pain radiating to the shoulders), a subcapsular haematoma must be suspected. In SA, facilities for confirming the diagnosis of a ruptured liver are not always available, especially in rural areas. Ditisheim and Sibai[1] suggest that ultrasound and/or CT may be used in so-called stable patients with abdominal pain. CT scans might be difficult to obtain, especially in emergency situations in SA, but mobile or bedside ultrasound scanning should be available in most highvolume regional and tertiary hospitals. None of the patients in this report had undergone ultrasound investigations. Nevertheless, in settings without bedside or mobile ultrasound equipment, a fetal tachycardia should alert a health professional of the possibility of intra-abdominal bleeding in the presence of upper abdominal pain and abdominal tenderness.[1] More importantly, if one suspects intra-abdominal bleeding in pregnancy associated with severe PE, HELLP or abruptio placentae, a team management approach involving obstetricians, surgeons (experienced in liver surgery), intensive care unit specialists and probably an interventionist radiologist must be strongly considered. In SA, such a recommendation may not always be practicable. Therefore, it is important to reach accord on referral indicators and pathways, and to establish an emergency call centre within a health district to obtain expert advice on a 24-hour basis.
There are two principles in the treatment of subcapsular liver haematoma, i.e. conservative, which includes hepatic artery embolisa-tion, and surgery, which includes abdominal packing, hepatectomy and/or a combination of these procedures.[1-3] More recently, liver transplantation has been reported,[1,3,8-11] but such management may not be readily available in SA in the near future.
It may not be surprising that hepatic embolisation was not considered in most of the cases reported, as such techniques may not be available in all regional and tertiary hospitals in SA. However, in patient 4, who was managed at the tertiary hospital, this procedure was carried out, but failed. It appears that hepatic artery embolisation should be considered in cases of suspected subcapsular haematoma or in combination with surgery, including 'packing of the liver'. This, despite the fact that embolisation might be associated with complications, such as liver necrosis.[2,3,12-14] Recent reports show that most liver haematomas from adult blunt injuries are treated successfully with hepatic artery embolisation.[14] Selective arterial embolisation has also been reported to improve outcomes of hepatic rupture from PE.[11]
In patients 2, 4 and 8 (abruptio placentae), subcapsular haematoma was not considered and the diagnosis of liver rupture was made at the time of caesarean delivery. Patients 2 and 8 (Table 1) were in private-sector hospitals and 1 patient was in a tertiary hospital. All 3 cases illustrate major issues associated with acute liver rupture, i.e. blood transfusion with packed red blood cells, platelet transfusion, fresh frozen plasma and cryoprecipitate infusion, but there were delays in obtaining surgical help. One patient received 14 U of packed red cells, a 5-hour operation and a repeat laparotomy. A high index of suspicion and advance management plans prior to surgery may reduce maternal mortality and morbidity.
Surgery for rupture of a subcapsular liver haematoma involves packing of the liver; this surgical technique has been described previously.[5] In patients 2, 4, 6 and 8, in whom rupture of the liver was diagnosed at caesarean delivery, suturing of liver lacerations and liver packing were performed; in only 1 case (patient 4) was embolisation attempted. These patients also had re-laparotomies for repacking of the liver haematoma.
In only 1 case did the assessors find that there was no suboptimal care (patient 4). This was a case of severe PE and abruptio placentae, and a cardiotocographic fetal heart rate abnormality warranted a caesarean delivery. After delivery of the fetus and placenta, atonicity of the uterus led to haemorrhage; compression sutures were inserted and uterine artery ligation was performed. On further examination, a ruptured liver was found and the haemorrhage could not be stopped, despite liver packing. The assessors considered the management appropriate. In the other 7 cases, assessors thought that the care was suboptimal.
One of the drawbacks of this report is that it did not review near-miss cases associated with subcapsular haematoma. Such a near-miss case in SA has been previously reported.[5]
Our general comments on the quality of care is that there was poor care in view of missing details in history, delays in management and failure to follow standard management protocols. Management of patients 1, 3, 5 and 7 illustrates that thorough and competent assessment of all pregnant women is necessary for problem recognition. From a review of these cases, it is strongly suggested that subcapsular haematoma and/or liver rupture should be considered and managed as follows:
-
Consider the diagnosis of liver haematoma in a patient with a diagnosis of severe PE and/or HELLP with symptoms and signs of epigastric pain radiating to the upper arm and shoulders, upper abdominal distension and haemodynamic instability. In the above-mentioned situation, strongly consider bedside ultrasound scanning to confirm subcapsular haematoma or its rupture.
-
Ensure that a laparotomy is done by a surgical team comprised of an experienced obstetrician and general surgeon experienced in liver surgery, and consider embolisation of the hepatic artery before or after surgery where subcapsular haematoma is suspected.
-
Ensure that all patients with severe PE and epigastric pain be observed in a high-care setting, liver function tests and platelet counts be performed and the results are obtained expeditiously within 30 minutes - 1 hour. Most complications of severe PE and HELLP syndrome can be avoided if these conditions are detected timeously. Antihypertensive therapy and magnesium sulphate should be prescribed appropriately, and delivery offered to all women with severe PE at 34 weeks' gestation or earlier, together with a prescription for antenatal steroids for fetal lung maturity and magnesium sulphate for fetal neuroprotection.
The abovementioned recommendations are shown diagrammatically in Fig. 1. In the presence of coagulopathy, suturing of the liver may provoke more bleeding; therefore, a judicious decision has to be made by the lead surgeon concerning the appropriateness of such an intervention. Notably, we have previously recorded success with hepatic packing.[5] The description of this technique is freely available online at https://doi.org/10.4103/1119-3077.151074.
Acknowledgements. National Committee on Confidential Enquiries into Maternal Deaths (NCCEMD) in South Africa.
Author contributions. JM: conceived the study, and collected and analysed the data. JM and NCN: drafted, revised and approved the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Ditisheim A, Sibai BM. Diagnosis and management of HELLP syndrome complicated by liver hematoma. Clin Obstet Gynecol 2017;60(1):190-197. https://doi.org/10.1097/GRF.0000000000000253 [ Links ]
2. Guntupalli SR, Steingrub J. Hepatic disease and pregnancy: An overview of diagnosis and management. Crit Care Med 2005;33(10 Suppl.):S332-S339. [ Links ]
3. Grand'Maison S, Sauvé N, Weber F, Dagenais M, Durand M, Mahone M. Hepatic rupture in hemolysis, elevated liver enzymes, low platelets syndrome. Obstet Gynecol 2012;119(3):617-625. https://doi.org/10.1097/AOG.0b013e318245c283 [ Links ]
4. Millan CA, Forero JC. Right hepatectomy after spontaneous hepatic rupture in a patient with preeclampsia: A case report. Int J Surg Case Rep 2017;39:250-252. https://doi.org/10.1016/j.ijscr.2017.07.057 [ Links ]
5. Ngene NC, Amin N, Moodley J. Ruptured subcapsular hematoma of the liver due to pre-eclampsia presenting as interstitial pregnancy and the role of intra-abdominal packing. Niger J Clin Pract 2015;18(2):300-303. https://doi.org/10.4103/1119-3077.151074 [ Links ]
6. Ngene NC, Moodley J. Assigning appropriate primary cause of death and indication for medical procedures. Med Hypotheses 2015;85(1):79-81. https://doi.org/10.1016/j.mehy.2015.04.002 [ Links ]
7. National Department of Health. Guidelines for maternity care in South Africa: A manual for clinics, community health centres and district hospitals. 2015. https://www.health-e.org.za/wp-content/uploads/2015/11/Maternal-Care-Guidelines-2015_FINAL-2L7.15.pdf (accessed 12 March 2018). [ Links ]
8. Erhard J, Lange R, Niebel W, et al. Acute liver necrosis in the HELLP syndrome: Successful outcome after orthotopic liver transplantation. A case report. Transpl Int 1993;6(3):179-181. [ Links ]
9. Zarrinpar A, Farmer DG, Ghobrial RM, et al. Liver transplantation for HELLP syndrome. Am Surg 2007;73(10):1013-1016. [ Links ]
10. Varotti G, Andorno E, Valente U. Liver transplantation for spontaneous hepatic rupture associated with HELLP syndrome. Int J Gynaecol Obstet 2010;111(1):84-85. https://doi.org/10.1016/j.ijgo.2010.05.010 [ Links ]
11. Vigil-De Gracia P, Ortega-Paz L. Pre-eclampsia/eclampsia and hepatic rupture. Int J Gynaecol Obstet 2012;118(3):186-189. https://doi.org/10.1016/j.ijgo.2012.03.042 [ Links ]
12. Zeirideen R, Kadir RA. Spontaneous postpartum hepatic rupture. J Obstet Gynaecol 2009;29(2):155. https://doi.org/10.1080/01443610802633874 [ Links ]
13. Araujo AC, Leao MD, Nobrega MH, et al. Characteristics and treatment of hepatic rupture caused by HELLP syndrome. Am J Obstet Gynecol 2006;195(1):129-133. https://doi.org/10.1016/j.ajog.2006.01.016 [ Links ]
14. Kozar RA, Moore FA, Moore EE, et al. Western Trauma Association critical decisions in trauma: Nonoperative management of adult blunt hepatic trauma. J Trauma 2009;67(6):1144-1149. https://doi.org/10.1097/TA.0b013e3181ba361f [ Links ]
 Correspondence:
Correspondence:
J Moodley
jmog@ukzn.ac.za
Accepted 2 April 2018














