Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 no.9 Pretoria Set. 2018
http://dx.doi.org/10.7196/samj.2018.v108i9.13070
RESEARCH
Compulsory community service for doctors in South Africa: A 15-year review
S J ReidI; J PeacockeII; S KornikIII; G WolvaardtIV
IMB ChB, MFamMed, PhD; Primary Health Care Directorate, Faculty of Health Sciences, University of Cape Town, South Africa
IIBSc (Med), MSc (Med); Africa Health Placements, Johannesburg, South Africa
IIIBBusSci, BComm Hons, MCom, CA (SA); Africa Health Placements, Johannesburg, South Africa
IVMB ChB, MMed, FCP (SA); Foundation for Professional Development, Pretoria, South Africa
ABSTRACT
BACKGROUND. Compulsory community service (CS) for health professionals for 12 months was introduced in South Africa (SA) in 1998, starting with medical practitioners. Up to 2014, a total of 17 413 newly qualified doctors and ~44 000 health professionals had completed their year of service in public health facilities around the country. While a number of studies have described the experience and effects of CS qualitatively, none has looked at the programme longitudinally.
OBJECTIVES. To describe the findings and analyse trends from surveys of CS doctors between 2000 and 2014, specifically with regard to their distribution, support, feedback and career plans.
METHODS. A consecutive cross-sectional descriptive study design was used based on annual national surveys of CS doctors. The study population of between 1 000 and 1 300 each year was surveyed with regard to their origins, allocations, experiences of the year and future career plans.
RESULTS. The total study population varied between 1 057 and 1 308 each year, with response rates of 20 - 77%. The average turn-up rate of 89% showed a decreasing tendency, while 77% of respondents were satisfied with the allocation process. Over the 15-year period, the proportion of CS doctors who were black and received a study bursary, and who were allocated to rural areas and district hospitals, increased. The great majority believed that they had made a difference (91%) and developed professionally (81%) over the course of the year, but only about half felt adequately supported clinically and administratively. The attitude towards CS of the majority of respondents shifted significantly from neutral to positive over the course of the 15 years. In terms of future career plans, 50% hoped to specialise, a decreasing minority to go overseas or into private practice, and a constant 15% to work in rural or underserved areas.
CONCLUSIONS. This study is the first to track the experience of compulsory CS over time in any country in order to describe the trends once it had become institutionalised. The SA experience of CS for doctors over the first 15 years appears to have been a successively positive one, and it has largely met its original objectives of redistribution of health professionals and professional development. Greater attention needs to be given to orientation, management support and clinical supervision, and focusing professional development opportunities on the important minority who are prepared to stay on longer than their obligatory year. CS still needs to be complemented by other interventions to capitalise on its potential.
Since the implementation in 1998 of the community service (CS) programme for 12 months of compulsory service for health professionals up to and including 2014, a total of 17 413 doctors of ~44 000 CS health professionals completed their year of service in public health facilities in South Africa (SA).[1] Doctors were the first to be contracted under this programme, followed by dentists, pharmacists and eventually all other health professionals, including nurses, who form the largest cohort.[2] The scheme currently employs an annual cohort of ~8 000 young professionals on 12-month contracts, who are allocated to public health facilities in different provinces according to the human resources need. While a number of studies have described the initial experience and effects of CS officers of various professional groups qualitatively,[3-7] none has yet looked at the programme longitudinally. This article focuses on medical practitioners, about whom most of the longitudinal data have been accumulated based on an annual survey of CS officers that was instituted in 2000.[3]
CS in SA primarily aimed to improve the supply of professional health personnel in underserved areas, thereby improving health service provision to all South Africans.[3] The objectives, gathered from a speech by Dr Ayanda Ntsaluba, director general of health in 1998, were as follows:
-
to ensure improved provision of health services to all citizens of the country
-
to provide our young professionals with an opportunity to further develop their skills, acquire knowledge and develop behaviour patterns and critical thinking that would help them in their professional development and future careers.
It is significant that the two objectives appear to be given equal importance, although the former might be regarded as the main purpose of the CS year. However, as the programme was said to be 'service, not training', CS officers were allocated according to healthcare needs, as determined by the National Department of Health,[4] rather than according to available supervision.[3]
Frehywot et al.,[9] in their study of compulsory service programmes worldwide, found that SA is one of 70 countries globally that implements compulsory CS.[9] They described three different types of compulsory service in different countries as follows:
-
a condition of service/state employment programme, e.g. for foreign-qualified professionals
-
compulsory service with incentives, such as education, employment or living conditions
-
compulsory service without incentives.
SA falls into the second category, with CS as a requirement for attaining full registration to practise publically or privately. A second strategy in the same category, which operates in countries such as Pakistan and Peru, uses a period of service in an underserved area as a prerequisite for career advancement such as specialisation. No rigorous study has systematically compared countries with rural and remote workforce disparities with compulsory service with those that do not have such programmes. They concluded that compulsory service programmes are a mechanism for staffing and reinforcing the health workforce, especially in areas where access to primary and essential healthcare services and systems are weak, but this should not be the only mechanism.
In 2010 the World Health Organization (WHO) developed a comprehensive set of guidelines based on the best available evidence for the recruitment and retention of healthcare professionals in rural and remote areas (Table 1), which include 'regulatory' interventions, such as compulsory service.[10] This places the strategy of coercion into a broader set of options for increasing the supply of health professionals in areas that are difficult to staff.[11]
In light of these alternatives, it is important to analyse the implementation and subsequent effect of the CS programme in SA against the initial objectives. Since its launch in 1998, various evaluations of the CS programme in SA have been completed, most of them qualitative in nature, focusing on its effectiveness,[12-15] to the extent of calling for its revision.[16] An analysis of the first year of CS implementation, using mixed methods, revealed a situation of some confusion in the absence of more specific guidelines. Consequently, provinces were left to make their own rules, which resulted in very variable implementation.[3] This initial study developed the first version of a survey tool, which was subsequently used annually until 2015, with some modifications, and forms the basis of the current review. Although the survey instrument has been modified over the intervening years, a sufficient number of data elements has remained unchanged to allow longitudinal trends to be described and comparisons made between the outcomes and demographic information, placement sites, provinces and universities of graduation.
Using the same data, a detailed study of the 2009 cohort of CS doctors developed a supervision satisfaction score (SSS) and found a high level of participant satisfaction with CS.[17] The authors noted that participants reporting professional development during the CS year were twice as likely to report intentions to remain in rural, underserved communities.
The initial 2001 study called for the establishment of a 'comprehensive policy of human resources for medically underserved areas in South Africa, with obligatory CS for doctors constituting only a part of it'.[3] It is in this context that the National Department of Health eventually developed a Human Resources for Health (HRH) strategy in 2011,[18] which included three strategic objectives directly relevant to CS: human resource management, quality of care and access in rural areas (Table 2).
By the time that the HRH strategy for 2012/2013 - 2016/2017 was published in 2011, the CS programme had already been running for 13 years and was institutionalised; therefore, the complementary strategies of the broader HRH policy framework that needed to optimise CS were not implemented for most of the period studied.
A summit on CS, convened by the Foundation for Professional Development (FPD) in 2015, aimed to review the progress of the programme and make recommendations for its further development.[19] Some of the results reported in this article were reported then, and the recommendations arising from the summit workshop have been incorporated into this article, representing the collective proposals of stakeholders rather than those of the authors alone.
Methods
Study objectives
This project aims to describe findings and analyse trends from surveys of CS doctors in SA between 2000 and 2014, specifically with regard to their distribution, support, feedback and career plans.
Study design
A consecutive cross-sectional descriptive study design was used based on annual national surveys of CS doctors.
Study variables
A structured self-assessment questionnaire developed from initial qualitative research conducted in 2000[3] was used, with some changes, adjustments and additions throughout the period. Most items requiring a subjective response were presented in the form of a 5-point Likert scale. Demographic variables included gender, race, marital status and receipt of a provincial bursary. Medical training characteristics included the university attended and level of the hospital of internship. A number of items explored characteristics of CS placement, including whether the facility was the participant's first, second or third choice in the allocation process. Rural placement was determined by participants, who indicated whether they received a government rural allowance. Placement satisfaction included practical items such as quality of accommodation, overtime duties, personal safety, fairness of remuneration and timeous payment of salaries. Their experiences of CS were indicated, e.g. by questions related to their attitude to CS, professional development, supervision and availability of seniors. Future career plans were assessed in terms of their intention to work in the public service or private sector, to specialise, or to work overseas or in a rural or underserved community.
Data collection
National, cross-sectional data were collected from CS officers using the abovementioned survey tool administered in the final quarter of each respective year. The cross-sectional design and methodology for the study from 2000 to 2008 made use of hard copies of the survey forms distributed and collected via provincial and hospital CS co-ordinators throughout SA. Attention was paid to confidentiality by using sealed envelopes when the hard-copy questionnaires were collected by the hospital CS co-ordinators. For the 2009 and subsequent studies, in an attempt to improve the response rate and validity, the methodology was according to that performed by Hatcher et al.,[17] in which participants were invited to complete the same survey instrument online, supplemented by follow-up phone calls to non-respondents, collated by an independent non-governmental organisation, Africa Health Placements. An information sheet explaining the study stipulated that completion of the survey implied consent, and that the survey was anonymous.
Additional information regarding turn-up rates was obtained directly from the National Department of Health. Turn-up rates were defined as the proportion of doctors who took up CS posts after completing their internship.
Data analysis
Data were cleaned and entered into Microsoft Access or Excel, analysed, and managed in Stata 13 (StataCorp., USA). Descriptive data (frequencies and proportions) were conducted for the entire cohort and the participating respondents.
Not all data were available for every year, because the survey tool varied slightly as the programme progressed. The results presented below represent the data that could be directly correlated to demonstrate trends.
Research ethics
The protocol for the earlier surveys up to 2011 was approved by the University of KwaZulu-Natal, Durban, and subsequent surveys were approved by the University of Cape Town Human Research Ethics Committee (ref. no. HREC 450/2012). The survey was anonymous and the covering letter containing information about the study made it clear that completion of the questionnaire implied consent.
Results
Turn-up and response rates
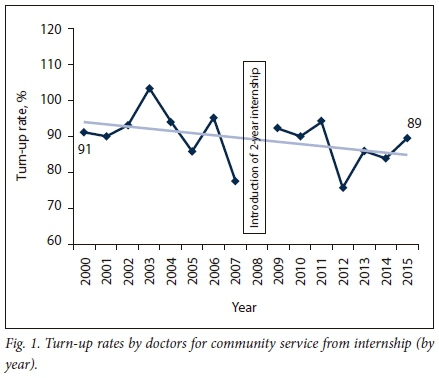
The total study population each year varied between 1 057 and 1 308. Turn-up rates were calculated independently of the surveys from data provided by the National Department of Health. Fig. 1 shows a slight decline in the year-on-year turn-up rate - from 91% in 2000 to ~87% in 2013, with an average of 89%, although there were wide variations. The data were interrupted by the introduction of the 2-year internship in 2008.
Response rates to the survey varied from a high of 77% in 2001 to a low of 20% in 2002, with an average of 51%, as data collection methods and availability of funding changed. For 2001, 2009, 2011 and 2013, which were used for comparative analysis below, the number of respondents was 902 (77%), 628 (48%), 668 (55%) and 648 (68%), respectively. Response rates for doctors from different universities were very similar across all years, whereas response rates within different provinces varied between 15% and 73% from 2000 to 2009, and between 42% and 51% from 2010 to 2014.
Demographics and allocations
Of the total sample, 58% were female and 36% were married. While the proportion of respondents who stated coloured and Indian as race remained fairly constant, the proportion stating black as race increased from 17% in 2001 to 45% in 2012, and those stating white as race decreased from 50% to 33% over the same period. These reciprocal changes were particularly rapid in the period 2009 - 2012.
There was a steadily increasing trend in the proportion of respondents who received a provincial study bursary - from 22% in 2009 to 42% in 2014 (no data were available before 2009). Similarly, the proportion of those allocated to rural hospitals, as measured by the payment of the rural allowance, rose from 24% in 1999, stabilising at ~50% between 2012 and 2014, with a high of 60% in 2007. The majority of CS respondents were placed at district hospitals, showing an increasing trend from 41% in 2001 to 49% in 2013, while those placed at tertiary and specialised hospitals decreased over the same period - from 18% to 15% - and regional hospital placements also decreased from 33% to 22%.
Fig. 2 plots the number of CS doctors allocated and the number of accredited facilities in each province against the percentage of the national population and the percentage of each rural provincial population, using data from StatsSA censuses 2001 and 2011,'2°1 with the latter in decreasing order. The aim of this comparison was to show allocations in terms of relative need in rural areas. Limpopo Province received a disproportionately low number of CS doctors for its rural needs, while the Western Cape and Gauteng provinces received disproportionately high numbers of CS doctors.

Applicants to the programme were required to make five choices from a list of public healthcare facilities approved for CS by the National Department of Health. If an allocation was not made within these initial requests, a second round of five choices was made available. A third round followed for the few who were still not allocated in the second round. The results show that an average of 80% of applicants were placed in the first round; this remained fairly constant from 2001 onwards, with a range of 77 - 87%. An average of 70% of respondents were satisfied with the allocation process. On analysing the proportion of posts filled by the end of the second round, the rural provinces (Eastern Cape, Limpopo, Northern Cape and North West) had disproportionately high numbers of vacant CS posts, indicating that these were not popular choices. Turn-up rates in the third round of allocations were the lowest of all (H Groenewald - personal communication, 2013).
Experiences of community service
A significant majority of respondents consistently stated that they had made a difference during their year of CS (76% in 2001, rising to 91% in 2014), and that they had experienced professional development (range 72 - 91%). An average of 96% performed overtime duties. Of those provided with accommodation, an average of 61% were satisfied with it, but 64% felt some risk to their personal safety (Table 3).
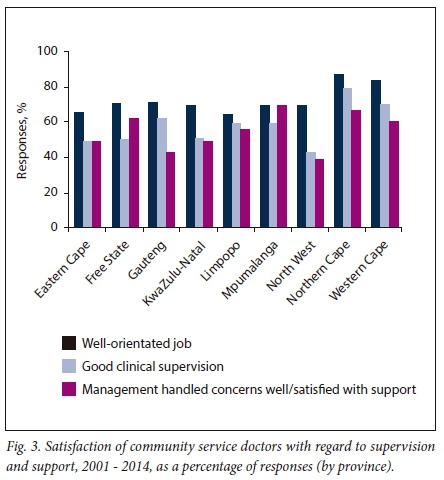
A ma'ority of CS doctors felt well orientated in their jobs (average 65%) and thought that they received good clinical supervision (average 52%). The latter varied according to placement site, with significantly fewer respondents in rural sites reporting good supervision than those in urban sites. However, just <50% of respondents said that their managers handled their concerns well and they were satisfied with the support received from them. This varied significantly by province - from 39% in North West to 69% in Mpumalanga (Fig. 3).
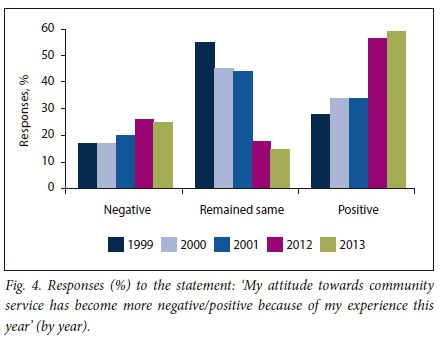
The attitude towards CS has been increasingly perceived as positive overall from 1999 to 2013 (Fig. 4). In response to the statement: 'My attitude towards community service has become more negative/ positive as a result of my experience this year', the majority of respondents had shifted from a neutral attitude to a positive one over the course of the 15 years.
Future career plans
Future work intentions varied widely on an annual basis. When comparing the average of respondents for each career intention for the last 3 years, the intention to move overseas had decreased significantly since a record figure of 43% was obtained from the 2001 survey (Table 4). However, the intention to move into the private sector and specialise had increased somewhat, with an average of 50% of CS doctors planning to specialise immediately after completing their CS year. The intention to remain at the same health facility and to work in rural, underserved communities had remained relatively static at ~30% and ~15%, respectively.
Discussion
CS in SA has become institutionalised and has stabilised as a programme. In contrast to the first few years of uncertainty and resentment, the expectations of all current SA health science graduates are that they will undergo their CS year in a public hospital, which is likely to be in a rural area, and conversely, hospital managers have come to rely on them as human resources.
Studies in other low- and middle-income countries, including Puerto Rico,[21] Indonesia,[22] Turkey,[23] and Thailand,[24] have demonstrated an improvement of staffing levels by doctors after the introduction of a period of compulsory service. As Frehywot et at.[9]assert:
'Compulsory service programmes are an instrument of social justice, an exercise in health equity, in that they enable governments to direct or augment health services to geographical areas that are not well served and in communities that are not favoured by market forces and health worker preferences.'
The increase in provincial study bursaries indicates an increasing sense of ownership of the future workforce by provincial health departments, and the allocation rate of 80% in the first round is commendable. However, if the turn-up rate is an indicator of the acceptability of CS among those who are eligible, the 11% who do not take up CS annually is cause for concern, as these 120 - 150 young doctors represent the output of one entire medical school. It is clear that there are significant personal choices to be made at that stage in life, such as starting a family or taking a break, and a degree of flexibility is needed. A small percentage might quit the profession either temporarily or permanently, and another group might head abroad directly after internship. Some applicants who are allocated in the second or third rounds might adopt a 'wait and see' strategy and do not turn up, preferring to wait unemployed for more desirable posts to become available in urban areas.
The primary objective of CS, to improve the distribution of health professionals throughout the country, has been partially achieved, as rural placements have increased to ~50%, but not to the extent of the relative need in rural provinces. Clearly, the CS workforce is a reliable recruitment strategy, bringing 8 000 fresh young graduates into the public service each year to fill the posts vacated by their predecessors, but the temporary contract nature of these posts creates a situation of constant staff turnover and does little to create a stable long-term workforce. Other human resource mechanisms complementary to CS are needed to achieve this. In other words, CS is an effective recruitment strategy, but in the absence of other interventions, does nothing for the development of an effective long-term workforce. Few international studies have shown increased retention of doctors after compulsory CS, while one SA study found 16% of CS doctors in one province remaining at the same district hospital beyond the obligatory time.[14] Pathman et at.,[25] in a 9-year follow-up study of doctors in the National Health Corps in the USA, found that those who were contracted into service in rural areas as compensation for the payment of their education costs, did not remain longer than their required service obligations. As previously pointed out, CS might to some extent defeat its own ends if newly qualified professionals assume that they have 'done their duty' and have compensated society for the costs of their studies after only 1 year in public service.[2]Nonetheless, the Umthombo Youth Development Foundation has raised the retention of graduates from rural areas that they support to >70% after they have completed their year-for-year contract time by means of effective mentoring and support.[26] It is, therefore, possible to achieve a much higher rate of retention in SA through complementary strategies.
Considering the data on career plans of CS doctors, the consistent 30% who preferred to stay on at their CS placement site, and the 15% who were prepared to work in rural or underserved areas after CS, consistent with other studies, represented an important human resource. If the latter were to be permanently employed and incentivised to create a longer-term experienced workforce, the problem of retention of professional staff in rural and remote areas could be solved in a few years by the accumulation of successive cohorts of willing professionals. It is better to have 1 doctor for 10 years than 10 doctors for 1 year each, as the continuity of relationships in medicine is not only more efficient but also leads to greater job satisfaction. In terms of achieving the first objective of CS, this hypothetical approach could be contrasted with forcing all graduates to work as so-called 'slaves of the state'.[27] However, despite the significance of the reaction to the coercive nature of CS, it has stabilised over time, as the turn-up rate of almost 90% and the rural career plans of 15% of each cohort mentioned above indicate.
The year-on-year variability of career plans is difficult to explain logically, apart from fluctuations in collective aspirations as opportunities changed. Since 2001, the decrease in intentions to practise abroad has been substantial, and probably is the result of the tightening of registration requirements in other countries rather than reduced local 'push' factors.[28] There may also have been a response bias, as those who were considering leaving the country may have been reluctant to reveal their plans in the survey, despite assurances of anonymity. The 30% who preferred to stay on at their CS hospital were probably disappointed because of the fixed-term contracts, as noted above, and the increasing challenge that provincial health departments are now having in funding permanent posts with the current budgetary restrictions.
The second objective of CS is also important, i.e. the professional development of young professionals. Often CS is the first in-depth exposure that junior doctors have to rural or underserved communities, and it is a significant wake-up call to the real health needs of large numbers of South Africans. Having the skills and confidence to make a difference after the 2-year internship, allows young doctors to stand on their own feet professionally and fulfil a real need, which carries the sense of professional satisfaction seen in the results. The direct exposure to the consequences of resource constraints in the public health service, including a relative lack of supervision and support, while not ideal, nevertheless serves to develop resilience in our young professionals for the challenges of future practice. By comparison, those trained in well-resourced settings do not cope as well.[29]
Attitudes towards CS have become progressively more positive over 15 years, rated by successive cohorts of CS doctors, which is an interesting finding, as it indicates that the experience of CS has shifted significantly, and the uncertainty and resentment that surrounded CS in its early years have possibly given way to accepting it as an unavoidable part of career development. The introduction of the occupation-specific dispensation in 2007,[30] which raised doctors' salaries to relatively high levels, might be linked to the improvement in attitudes, while more indirect links could have been the parallel increase in the proportion of black graduates, provincial bursary holders and rural placements. More qualitative research is warranted to explore this phenomenon.
The level of support from managers, rated at an average of 50%, is inadequate and represents a waste of human resource potential. That <50% of the respondents in KwaZulu-Natal, Limpopo and Mpumalanga felt adequately supervised clinically and supported by management, is an indictment on those seniors and managers. This young cohort of professionals could contribute their skills and energy far more effectively if they are proactively incorporated into working teams, supervised and mentored by more experienced practitioners, and supported administratively through decent housing and living conditions.
Study limitations
The response rates were reasonable for repeated surveys of this nature, but the limitations of the study include a substantial response bias. Those who completed the surveys, although demographically similar to the study population as a whole, were more likely to have been positive about their experiences; therefore, the results may reflect a more optimistic view than the reality. They also rely on self-reported feedback, which cannot easily be verified, and so the true picture of CS may be different to what is reported. The changes in the survey tool over 15 years introduced some variations, but having a single principal investigator played a part in ensuring consistency of data collection and results. Finally, a possible social desirability bias was mitigated to some extent by emphasising that the results would be collated by an organisation independent of the National Department of Health - in earlier surveys the University of KwaZulu-Natal and in later ones, Africa Health Placements.
Conclusion
This study is the first to track the experience of compulsory CS over time in any country in order to describe the trends once CS has become institutionalised. The SA experience of CS for doctors over the first 15 years appears to have been a successively positive one, and it has largely met its original objectives of redistribution and professional development. CS has become an indispensable part of the provincial health services, particularly in rural hospitals, but also in larger urban hospitals. It is a medical workforce that managers can rely on each year without having to actively recruit, at the cost of annual orientation and management of successive cohorts of young professionals. As the results show, however, they could improve this renewable resource by giving more attention to orientation, management support and clinical supervision, and by focusing professional development opportunities on the important minority who are prepared to stay on longer than their obligatory year. As an entrenched feature of the national HRH strategy, CS still needs to be complemented by other interventions to capitalise on the potential it represents. Alternative strategies to retain doctors and other health professionals in rural and underserved areas, as suggested by the WHO, must be considered rather than relying only on coerced junior health professionals who rotate out after a year. A stable long-term workforce can only be achieved, particularly in rural and underserved areas, through a multifaceted human resource management plan.
Recommendations
Recommendations from the Community Service for Health Professionals summit, held at the FPD, are set out in Table 5.[19]
Acknowledgements. The authors are grateful to the National Department of Health, provincial CS co-ordinators and hospital CS co-ordinators for their assistance with data collection, and Alet Bosman of the Foundation for Professional Development (FPD) for assisting with data analysis. We thank the FPD and Dr Gwen Ramokgopa for convening the 2015 summit.
Author contributions. SR: designed the study, oversaw the data collection and drafted the manuscript as a whole. JP: collated the data, performed the statistical analyses and drafted the methods and findings sections. SK: facilitated the data collection from 2011 and reviewed the manuscript. GW: facilitated the funding for the study from 2011, and reviewed the manuscript.
Funding. The initial study was funded by the Health Systems Trust, and annual surveys from 2000 to 2010 were funded by the National Department of Health. Surveys from 2011 to 2014 were funded by the United States Agency for International Development (USAID) under the United States President's Emergency Plan for AIDS Relief (PEPFAR) programme.
Conflicts of interest. None.
References
1. Motsoaledi A. Community service to improve access to quality health care to all South Africans. Budget Speech. 2014. http://www.doh.gov.za/show.php?id=447 (accessed 24 November 2017). [ Links ]
2. Reid S. Community Service for Health Professionals. South African Health Review. Durban: Health Systems Trust, 2002:135-160. [ Links ]
3. Reid SJ. Compulsory community service for doctors in South Africa - an evaluation of the first year. S Afr Med J 2001;91(4):329-336. [ Links ]
4. National Department of Health. Health Professions Act 56, 1974. Regulations relating to performance of community service by persons registering in terms of the Health Professions Act, 1974. Government Gazette No. 18890:R688. 1998. [ Links ]
5. Naidoo S, Chikte U. Community dental service - the first year. S Afr Dent J 2002;57(5):193-196. [ Links ]
6. Khan NB, Knight S, Esterhuizen T. Perceptions of and attitudes to the compulsory community service programme for therapists in KwaZulu-Natal. S Afr J Comm Disord 2009;56:17-22. [ Links ]
7. Visser J, Marais M, Plessis J, Steenkamp I, Troskie I. Experiences and attitudes of dietitians during the first compulsory community service year. S Afr J Clin Nutr 2006;19(1):10-17. https://doi.org/10.1080%2F16070658.2006.11734084 [ Links ]
8. Pillay A, Harvey B. The experiences of the first South African community service clinical psychologists. S Afr J Psychol 2006;36:259-280. https://doi.org/10.1177%2F008124630603600204 [ Links ]
9. Frehywot S, Mullan F, Payne PW, Ross H. Compulsory service programmes for recruiting health workers in remote and rural areas: Do they work? Bull World Health Organ 2010;88:364-370. https://doi.org/10.2471%2Fblt.09.071605 [ Links ]
10. World Health Organization. Increasing Access to Health Workers in Remote and Rural Areas Through Improved Retention: Global Policy Recommendations. Geneva: WHO, 2010. [ Links ]
11. Dolea C, Stormont L, Braichet J-M. Evaluated strategies to increase attraction and retention of health workers in remote and rural areas. Bull World Health Organ 2010;88(5):379-385. https://doi.org/10.2471%2Fblt.09.070607 [ Links ]
12. Nemutandani MS, Maluleke FRS, Rudolph MJ. Community service doctors in Limpopo province. S Afr Med J 2006;96(3):180-182. [ Links ]
13. Penn C, Mupawose A, Stein J. From pillars to posts; some reflections on community service six years on. S Afr J Commun Disord 2009;56:8-16. [ Links ]
14. Ross A, Reid S. The retention of community service officers for an additional year at district hospitals in KwaZulu-Natal and the Eastern Cape and Limpopo provinces. S Afr Fam Pract 2009;51:249-253. https://doi.org/10.1080%2F20786204.2009.10873856 [ Links ]
15. Parker W, Steyn N, Mchiza Z, et al. Challenges for efficient health service delivery: Experiences of dietitians completing their compulsory community service year in South Africa. Public Health Nutr 2012;15(8):1411-1418. https://doi.org/10.1017%2Fs1368980011003314 [ Links ]
16. Van Niekerk J de V. Internship and community service require revision. S Afr Med J 2012;102(8):638. https://doi.org/10.7196%2Fsamj.6094 [ Links ]
17. Hatcher AM, Onah M, Kornik S, Peacocke J, Reid S. Placement, support, and retention of health professionals: National, cross-sectional findings from medical and dental community service officers in South Africa. Hum Resour Health 2014;12:14. https://doi.org/10.1186%2F1478-4491-12-14 [ Links ]
18. National Department of Health. Human Resources for Health Strategy for the Health Sector 2012/13 - 2016/17. Pretoria: NDoH, 2011. [ Links ]
19. Foundation for Professional Development. Report of the Community Service for Health Professionals Summit, 22 April 2015. Pretoria: FPD, 2015. [ Links ]
20. Laldaparsad S. Urban and rural trends in South Africa. Pretoria: Statistics South Africa, 2012. [ Links ]
21. Ramirez de Arellano AB. A health 'draft': Compulsory health service in Puerto Rico. J Public Health Policy 1981;2:70-74. https://doi.org/10.2307%2F3342100 [ Links ]
22. Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: A literature review of attraction and retention. BMC Health Serv Res 2008;8:19. https://doi.org/10.1186%2F1472-6963-8-19 [ Links ]
23. Erus B, Bilir A. Obligatory service requirement and physician distribution in Turkey. Eur J Public Health 2007;17(Suppl 2):175. [ Links ]
24. Wongwatcharapaiboon P, Sirikanokwilai N, Pengpaiboon P. The 1997 massive resignation of contracted new medical graduates from the Thai Ministry of Public Health: What reasons behind? Hum Res Health Develop J 1999;3:147-156. [ Links ]
25. Pathman DE, Konrad TR, Ricketts TC. The comparative retention of National Health Service Corps and other rural physicians; results of a 9-year follow-up study. JAMA 1992;268(12):1552-1558. https://doi.org/10.1001%2Fjama.1992.03490120066030 [ Links ]
26. Ross A, MacGregor G, Campbell L. Review of the Umthombo Youth Development Foundation scholarship scheme, 1999 - 2013. Afr J Prim Health Care Fam Med 2015;7(1):1-6. https://doi.org/10.4102%2Fphcfm.v7i1.739 [ Links ]
27. Erasmus N. Slaves of the state: Medical internship and community service in South Africa. S Afr Med J 2012;102(8):655. https://doi.org/10.7196%2Fsamj.5987 [ Links ]
28. Labonté R, Sanders D, Mathole T, et al. Health worker migration from South Africa: Causes, consequences and policy responses. Hum Resource Health 2015;13:92. https://doi.org/10.1186/s12960-015-0093-4 [ Links ]
29. Phalime M. Postmortem: The Doctor Who Walked Away. Cape Town: Tafelberg, 2014. [ Links ]
30. South Africa. Occupation Specific Dispensation (OSD) in the Public Service. 2007. [ Links ]
 Correspondence:
Correspondence:
S J Reid
steve.reid@uct.ac.za
Accepted 6 April 2018














