Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 no.9 Pretoria Set. 2018
http://dx.doi.org/10.7196/samj.2018.v108i9.13054
RESEARCH
The unmet needs and health priorities of the urban poor: Generating the evidence base for urban community health worker programmes in South Africa
A van RieI; N S WestII; S R SchwartzIII; L MutungaV; C F HanrahanIV; J NcayiyanaVII; J BassettVI
IMD, PhD; Department of Epidemiology and Social Medicine, University of Antwerp, Belgium
IIMSPH; Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Md, USA
IIIPhD, MPH; Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Md, USA
IVPhD, MS; Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Md, USA
VMS; Witkoppen Health and Welfare Centre, Johannesburg, South Africa
VIMB BCh;Witkoppen Health and Welfare Centre, Johannesburg, South Africa
VIIPhD; School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. There is a growing interest in involving community health workers (CHWs) into the formal healthcare system in South Africa (SA).
OBJECTIVES. To generate evidence for defining CHW tasks in urban SA.
METHODS. A cross-sectional survey of residents of Diepsloot, northern Johannesburg, was performed using geographically weighted random sampling, with home-based health assessment and a questionnaire on sociodemographics, medical history, experience of violence, health-seeking behaviour and perceived health priorities.
RESULTS. Between May 2013 and March 2014, 1 230 adults participated. Self-reported medical conditions included hypertension (12%), HIV (10%), diabetes (3%), cancer (1%) and mental illness (1%). Health assessments identified a high prevalence of undiagnosed conditions: hypertension (26%), obesity or overweight (46%), mild to severe depression (23%), HIV infection (5.8%) and tuberculosis (TB) (0.4%). Among women, 18% had unmet family planning needs and 77% had never had a Pap smear. Sexually transmitted infection symptoms were reported by 7% of participants. Physical violence was widespread, with 13% having experienced and 16% witnessing violence in the past year, with women mostly experiencing violence at home and men in the community. Participants' top health concerns were crime, safety and violence (49%) and HIV (18%); healthy living/weight control was listed by only 8% of participants.
CONCLUSIONS. Alignment of CHW roles to unmet health needs and perceived health priorities will be important for optimal impact of CHW programmes in urban communities. Our data suggest that the CHW role should expand from a traditional focus on HIV, TB and maternal health to include non-communicable diseases, healthy lifestyle, and the intersection of violence and health.
Since the adoption of the Alma-Ata Declaration, primary healthcare (PHC) has been the global paradigm for comprehensive, equitable and affordable healthcare.[1] According to the Declaration, PHC should provide health education, promote appropriate nutrition and sanitation, deliver maternal and child health services, offer vaccination, aim to prevent endemic diseases and provide treatment for common diseases. The Declaration further states that PHC should bring healthcare as close as possible to the places where people live and work, that PHC should constitute the first element of a continuing healthcare process, and that it should rely on health workers, including community health workers (CHWs), who are trained to respond to the health needs of the community.[2] PHC initially focused efforts on expanding health facilities with highly skilled workers,[3] and CHWs were only viewed as a temporary measure to fill gaps and overcome the lack of skilled workers. More recently, the severe shortage of healthcare workers in low- and middle-income countries (LMICs) has renewed interest in task-shifting and CHW programmes.[4] The World Health Organization Global Strategy on Human Resources for Health: Workforce 2030[5] and the United Nations Leaving No One Behind[6] reports recognised that addressing population needs will require a more sustainable and responsive skills mix of healthcare workers, including CHWs who deliver services at the community and household level.
In Africa, most CHW programmes are vertically and disease orientated, with a focus on maternal and child health, tuberculosis (TB), HIV or malaria.[7,8] This has resulted in an amalgam of well-intended, top-down and externally funded CHW programmes that often experience important challenges in achieving their potential owing to poor planning, poor supervision, fragmented disease-specific training and tenuous links with the formal health system, resulting in an inefficient use of valuable human resources.[7-9]
There is a growing consensus that CHW programmes require a comprehensive reconfiguration of PHC teams, with changes in scope and role of CHWs, development of regulatory frameworks, integration of CHWs in the formal healthcare system, and enhanced training and continuing education.[2-4,7,9-11] In this spirit, the South African (SA) Ministry of Health developed a vision for the re-engineering of PHC, with a central role for PHC outreach teams that are accountable to the health facility.[12] The role of the CHWs, under supervision of a professional nurse, is comprehensive with regard to disease prevention and health promotion, with a focus on HIV/TB, maternal and child health, non-communicable diseases (NCDs) and social determinants of health. The Ministry of Health acknowledged that PHC outreach teams need to respond to the evolving public health challenges in the era of increased migration, urbanisation and the epidemiological transition from infectious disease to NCDs.
Objectives
To assess the most prevalent health problems, unmet health needs and health priorities experienced by residents of an impoverished urban community in Johannesburg, SA, in order to gather the evidence required to align the tasks, training needs and curricula for urban CHWs with the needs of the community.
Methods
Between May 2013 and March 2014, we performed a cross-sectional survey of residents of Diepsloot, a densely populated, poor urban township consisting of formal and informal settlements in northern Johannesburg. Diepsloot is approximately 12 km2 in area and has an estimated population of 350 000, resulting in a very high population density of almost 30 000 people/km2.[13] Housing is a mixture of corrugated iron shacks and governmental Reconstruction and Development Programme houses. Healthcare is provided by two public primary care clinics, private doctors and traditional healers, as well as public and private hospitals located at a distance in central Johannesburg.
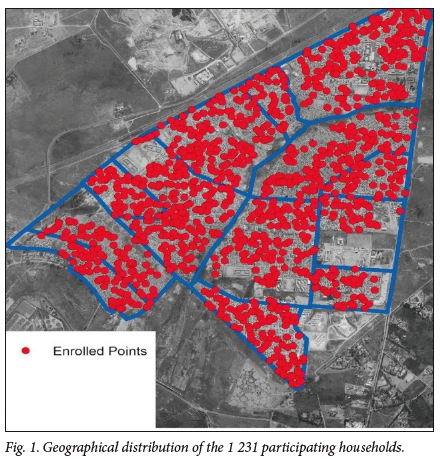
By using a geographically weighted random sampling framework, we aimed to include a representative sample of all Diepsloot adult (age >15 years) residents and their children. Survey teams consisting of nurses and lay HIV counsellors visited the closest household to each of the 2007 randomly selected geo-co-ordinates. At time of the home visit, all household members were enumerated and one adult household member was randomly selected for study participation using the Kish grid method.[14] This method, the gold standard for within-unit respondent selection for interviewer-administered surveys, was applied to prevent the bias that would occur when only family members who are at home at time of the first visit are enrolled. When the randomly selected household member was not at home, the survey team completed up to four additional household visits on different days and times to maximise enrolment.
All consenting participants underwent a home-based health assessment that included anthropometrics, blood pressure measurement, collection of a urine sample for point-of-care assessment of proteinuria and glucosuria, pregnancy testing, HIV counselling and testing, assessment for latent Mycobacterium tuberculosis infection by tuberculin skin testing, diagnosis of active TB by symptom screening and sputum Xpert MTB/RIF in participants with presumptive TB, and screening for mental health using the Mental Health Inventory-5 (MHI-5).[15] Individuals in need of care or further assessment were referred to the primary care clinic of their choice.
A questionnaire was administered by the survey team to assess sociodemographics, reproductive health and medical history (including TB, HIV, sexually transmitted infections, injury, hypertension, cardiovascular diseases, cancer, mental health, chronic obstructive pulmonary disease, asthma, arthritis and epilepsy), experience of violence and health-seeking behaviour. To determine the health priorities from the participant perspective, we asked: As a woman/man in this community, what is your/your partner's/your children's single biggest health-related concern?'
We performed a descriptive analysis, presenting proportions and means, and compared findings between genders using t-tests for means, Wilcoxon rank-sum tests for medians, and χ2 tests for proportions. Overweight was defined as body mass index (BMI) between 25.0 and 29.9 kg/m2, obesity as BMI >30 kg/m2, hypertension as blood pressure >140 mmHg systolic and/or >90 mmHg diastolic based on the average calculated from three measurements, and presence of depressive symptoms as a score <68 on the MHI-5. All analyses were performed in Stata version 13 (StataCorp, USA).
Ethical approval for the study was obtained from the Human Research Ethics Committee of the University of the Witwatersrand (ref. no. M130204) and the Institutional Review Board of the University of North Carolina at Chapel Hill (ref. no. 13-1654). All participants provided written informed consent (adults) or assent (children).
Results
Study population and characteristics
Between May 2013 and March 2014, 2007 randomly selected geo-co-ordinates were visited, which resulted in the enrolment of 1 231 participants. Of the remaining 782 (39%) sampling points, 401 households refused participation, 321 households agreed to participate but the randomly selected household member could not be reached despite five attempts, and 60 were ineligible due to lack of knowledge of English, Sesotho or isiZulu or because there was no household living within 30 m of the GPS point. Despite incomplete participation, we achieved a geographical distribution of participation similar to what was targeted (p=0.997) (Fig. 1).
Among the 1 231 adult participants, the median age was 32 years (interquartile range (IQR) 26 - 42) and 55% were female. The median length of time participants had lived in Diepsloot was 8 years (IQR 4 - 13). Most (75%) had a current partner (boyfriend, girlfriend or spouse). One in five self-reported a nationality other than South African (Table 1). The majority (57%) were unemployed. Even though half (51%) of all participants lived in an informal dwelling constructed with cardboard or corrugated iron, most had electricity (73%) and access to piped water in their home (75%).
Health and health-seeking behaviour
Self-reported alcohol consumption was low, with 80% of women and 46% of men reporting that they never drink alcohol, and only 13 men and 1 woman reporting drinking >5 days per week (Table 2). Current tobacco use was high among men (43%) but low among women (5%). Physical activity was low, with most participants (70%) not having engaged in any type of vigorous physical activity (running, heavy lifting, aerobics or fast bicycling) in the past week, and less than half (47%) having walked for >30 minutes for 2 or more days in the past week.
Health-seeking behaviour was higher among women than among men, with most women (70%) but less than half of all men (44%) having accessed formal health services in the past year, mainly at primary care clinics in the community (91%). Most participants (85%) were satisfied with the healthcare they received. Common reasons for dissatisfaction were long waiting times (42%), poor quality of care (33%) and rude clinic staff (12%).
Burden of disease and unmet health needs
Self-report of known medical conditions included hypertension (11%), HIV infection (10%), diabetes (3%), cancer (1%), high cholesterol (1%), mental health conditions (1%) and active TB (0.04%) (Table 3). In contrast to the relatively low prevalence of known health conditions, a large burden of undiagnosed health problems was identified during the health assessment. Hypertension was equally common in men (28%) and women (24%) (p=0.114). Almost half of all participants (48%) were either obese or overweight, with women more likely to be overweight or obese compared with men (30% v. 19% overweight; p<0.001, and 36% v. 7% obese; p<0.001). One in four participants (23%, n=283) reported symptoms of depression. Among participants not known to be HIV-infected, 8.4% were newly diagnosed with HIV. One in three (34%) of those in whom a tuberculin skin test was done (n=446) were diagnosed with latent M. tuberculosis infection. Only 5 participants (0.4%) were diagnosed with active TB disease.
A substantial proportion (30%) of the 567 women who were sexually active, had no reproductive intentions and were not using contraception reported unmet family planning needs, and only one in three women (30%) had ever had a Pap smear to screen for cervical cancer. Symptoms of sexually transmitted infection were reported by 11% of men and women. Less than half of all participants (49% of men and 38% of women) reported condom use the last time they had sex.
A substantial proportion of participants had experienced (12%) or witnessed (16%) physical violence in the past year, either in a public place (57%) or at home (43%). Men were as likely as women to have experienced violence (13% v. 12%; p=0.398), but men were more likely to have witnessed violence (20% v. 13%; p=0.001). Violence in the home was experienced more often by women (68% v. 17%; p<0.001), while men were more likely than women to experience violence in a public place (83% v. 32%; p<0.001).
Health priorities
For both men and women, the top health concerns for themselves were crime, safety or violence (52% of men and 49% of women) and HIV (20% of women and 17% of men) (Fig. 2). Issues less frequently reported as health priorities were healthy living or weight control (10% of men and 8% of women), water and sanitation (8% of men and 7% of women), and alcohol or substance abuse (5% of men and 2% of women). TB and cancer were rarely reported as a health priority (<2%). Women perceived crime, safety, violence or abuse (48%) and HIV (35%) as the health priorities for their partners. Similarly, men perceived crime, safety, violence or abuse (61%) and HIV (24%) as top health concerns for their female partners. Crime, safety, violence and abuse were also the top health concerns shared by both men and women for their children (60% of men and 62% of women).

Discussion
The goals of 'Leaving no one behind' and achieving universal and equitable health coverage in LMICs will require the development of a health system that responds to the greatest needs of the population and appeals to the community.[4,16]
In 2011, SA started establishing ward-based CHW outreach teams. Rapid assessments of these programmes have found that they can contribute to maternal and child health, adherence support and home-based care, but insufficient attention has been paid to human resources, leadership and accountability, infrastructure and provision of materials.[17,1] CHWs are often inadequately prepared and have a low level of education, and competencies are limited as they are created through a legacy of vertical programmes.[18] It has been highlighted that the programme requires detailed policy directives, planning guidelines, budgetary commitments, commitment to human resources development and capacity building, and better integration into the healthcare system.[19]
To optimise these programmes, policy makers must be aware of the unmet needs of the most vulnerable and poor in their country and gain insights into the people's perspectives on health priorities. Unfortunately this information is scarce, as most research on unmet needs has been fragmented, with a focus on reproductive and sexual health (including contraception, family planning and obstetric care), mental health and oral health. Similarly, insights on public health priorities from a community perspective are rarely available.
In this cross-sectional survey of residents of an impoverished urban community in Johannesburg, we observed that men had poor health-seeking behaviour and that obesity, hypertension and depression were the most common undiagnosed medical conditions. Furthermore, in contrast to our expectation, violence and not HIV, TB or NCDs were viewed by the community as their top health concern. Our findings confirm that the urban poor have a triple burden of health problems as they suffer disproportionately from communicable diseases, NCDs, and exposure to the negative health effects associated with the wealth inequalities that characterise many cities in LMICs.[20] It has been suggested that CHWs may be the 'secret weapon' to combat NCDs as they can effectively screen populations for NCD risk, act as agents of social change, facilitate information and education campaigns through existing social networks, and reach out to populations who have limited mobility and low decision-making power.[3,21,22] Our findings also highlight that the urban poor suffer disproportionately from interpersonal violence, which is a risk factor for poor health as it increases an individual's risk of substance abuse and mental health disorders, and inflicts poverty through school dropout, unemployment, and death or disability of a breadwinner.[23] As Nelson Mandela wrote, 'Many who live with violence day in and day out assume that it is an intrinsic part of the human condition. But this is not so. Violence can be prevented. Governments, communities and individuals can make a difference.'[23] When appropriately trained, CHWs could create awareness and foster community-based action to generate resilience against violence and its negative effects on health.[7,10] Given the level of violence in many urban African settings, attention should also be paid to the protection of CHWs when providing care in these communities.
Our data provide useful information for the SA PHC re-engineering programme. In this programme, the CHWs are expected to promote health and provide comprehensive care with a focus on HIV/TB, maternal and child health, NCDs and social determinants of health. Our data suggest that policy makers will also need to find ways to effectively engage men into community-based care and include efforts that promote a healthy lifestyle. Furthermore, with violence being the communities' top health priority, strategies to prevent violent behaviour, reverse social fragmentation, and generate resilience to the negative health effects of violence in the urban poor should be included in PHC strategies.
Study strengths and limitations
Strengths of this study are its large sample size, participatory nature, comprehensiveness with regard to array of health topics investigated, and methodological rigour (geographically weighted sampling and Kish method for within-unit respondent selection), resulting in high internal validity of the results. However, the interpretation of the results is limited by two important factors. First, 20% of eligible households refused participation, and among households agreeing to participate, the randomly selected adult in the households could not be identified in 16% of cases despite multiple attempts. While this may have resulted in some selection bias, we believe it to be minimal as the geographical representation of participants was similar to our a priori set target. Second, we asked participants about their healthcare-seeking behaviour in the past year but did not explore whether they had been visited by a CHW. Finally, we investigated the unmet needs and priorities of a single urban community, limiting the generalisability of the results.
Conclusions
CHWs fully aligned with and integrated in the formal healthcare system could play a front-line role in the equitable expansion of disease prevention and health promotion if they respond to the needs and expectations of the urban communities. Future research should evaluate breadth of CHW coverage in marginalised and poor communities, and the extent to which CHWs address unmet needs and health priorities.
Acknowledgements. We extend our thanks to all the survey participants who contributed their valuable time, and the data collection team for their hard work. We also thank Ian Sanne, the Community Advisory Forum, Diepsloot service providers, the Diepsloot ward counsellors and offices of the Diepsloot ward counsellors, and the Diepsloot South African Police Service for their support.
Author contributions. AvR, SS, CH and JB designed the study, NW and LM supervised all data collection, JN participated in data collection, AvR, NW, SS, CH and JN contributed to data analysis, AvR drafted the manuscript, and all authors contributed to and approved the final version of the manuscript.
Funding. This study was funded by the United States Agency for International Development (USAID) under award number AID-674-A-12-00033, with additional funding from AID 674-A-12-00020.
Conflicts of interest. None.
References
1. World Health Organization. Declaration of Alma Ata. Geneva: WHO, 1978. http://www.who.int/publications/almaala_declaration_en.pdf (accessed 3 July 2018). [ Links ]
2. Hall JJ, Taylor R. Health for all beyond 2000: The demise of the Alma-Ata Declaration and primary health care in developing countries. Med J Aust 2003;178(1):17-20. [ Links ]
3. Liu A, Sullivan S, Khan M, et al. Community health workers in global health: Scale and scalability. Mt Sinai J Med 2011;78(3):419-435. https://doi.org/10.1002/msj.20260 [ Links ]
4. Maher D, Cometto G. Research on community-based health workers is needed to achieve the sustainable development goals. Bull World Health Organ 2016;94(11):786. https://doi.org/10.2471/BLT.16.185918 [ Links ]
5. World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030. Geneva: WHO, 2016. http://www.who.int/hrh/resources/globstrathrh-2030/en/(accessed 31 July 2018). [ Links ]
6. United Nations. Leaving No One Behind: The Imperative of Inclusive Development. Report on the World Social Situation 2016. New York: United Nations, 2016. http://www.un.org/esa/socdev/rwss/2016/full-report.pdf (accessed 3 August 2018). [ Links ]
7. Tulenko K, Mogedal S, Afzal MM, et al. Community health workers for universal health-care coverage: From fragmentation to synergy. Bull World Health Organ 2013;91(11):847-852. https://doi.org/10.2471/BLT.13.118745 [ Links ]
8. Schneider H, Okello D, Lehmann U. The global pendulum swing towards community health workers in low- and middle-income countries: A scoping review of trends, geographical distribution and programmatic orientations, 2005 to 2014. Hum Resour Health 2016;14(1):65. https://doi.org/10.1186/s12960-016-0163-2 [ Links ]
9. Lehmann U, Sanders D. Community Health Workers: What Do We Know About Them? The State of the Evidence on Programs, Activities, Costs and Impact on Health Outcomes Using Community Health Workers. Geneva: World Health Organization, 2007. http://www.who.int/hrh/documents/community_health_workers.pdf (accessed 3 August 2018). [ Links ]
10. Standing H, Chowdhury AM. Producing effective knowledge agents in a pluralistic environment: What future for community health workers? Soc Sci Med 2008;66(10):2096-2107. https://doi.org/10.1016/j.socscimed.2008.01.046 [ Links ]
11. Lehmann U, van Damme W, Barten F, et al. Task shifting: The answer to the human resources crisis in Africa? Hum Resour Health 2009;7:49. https://doi.org/10.1186/1478-4491-7-49 [ Links ]
12. Pillay Y, Barron P. The Implementation of PHC-reengineering in South Africa. Cape Town: Public Health Association of South Africa, 2011. [ Links ]
13. Statistics South Africa. Census 2011 - interactive data in SuperCROSS. Johannesburg: Stats SA, 2011. [ Links ]
14. Kish L. A procedure for objective respondent selection within the household. J Am Stat Assoc 1949;44(247):380-387. https://doi.org/10.1080/01621459.1949.10483314 [ Links ]
15. Berwick DM, Murphy JM, Goldman PA, et al. Performance of a five-item mental health screening test. Med Care 1991;29(2):169-176. https://doi.org/10.1097/00005650-199102000-00008 [ Links ]
16. Mburu FM. Health systems as defences against the consequences of poverty: Equity in health as social justice. Soc Sci Med 1983;17(16):1149-1157. https://doi.org/10.1016/0277-9536(83)90007-2 [ Links ]
17. Sodo P, Bosnians A. Progress of the municipal ward-based primary health care outreach teams in Vhembe, Limpopo Province. Strengthening Health Syst 2017;2(1):18-22. https://doi.org/10.7196/SHS.2017.v2.i1.34 [ Links ]
18. Jinabhai CC, Marcus TS, Chaponda A. Rapid appraisal of ward-based outreach teams. 2015. https://www.up.ac.za/media/shared/62/COPC/COPC%20Reports%20 Publications/wbot-report-epub-lr-2.zp86437.pdf (accessed 3 August 2018). [ Links ]
19. Munshi S. Exploring the municipal ward based primary health care outreach teams implementation in the context of primary health care re-engineering in Gauteng. Master's in Public Health thesis. Johannesburg: School of Public Health, Faculty of Health Sciences, Universityof the Witwatersrand, 2017. http://wiredspace.wits.ac.za/bitstream/handle/10539/23346/SMunshi_Thesis _Final%20 Version_19%20June%20_submission.pdf?sequence=1&isAllowed=y (accessed 3 August 2018). [ Links ]
20. Harpham T. Urban health in developing countries: What do we know and where do we go? Health Place 2009;15(1):107-116. https://doi.org/10.1016/j.healthplace.2008.03.004 [ Links ]
21. Jarvis JD, Kataria I, Murgor M, et al. Community health workers: An underappreciated asset to tackle NCD. Glob Heart 2016;11(4):455-457. https://doi.org/10.1016/j.gheart.2016.10.004 [ Links ]
22. Gaziano TA, Abrahams-Gessel S, Denman CA, et al. An assessment of community health workers' ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: An observational study. Lancet Glob Health 2015;3(9):e556-e563. https://doi.org/10.1016/S2214-109X(15)00143-6 [ Links ]
23. World Health Organization. Global Status Report on Violence Prevention 2014. Geneva: WHO, 2014. http://www.who.int/violence_injury_prevention/violence/status_report/2014/en/ (accessed 3 August 2018). [ Links ]
 Correspondence:
Correspondence:
A van Rie
annelies.vanrie@uantwerpen.be
Accepted 15 March 2018














