Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 no.8 Pretoria Ago. 2018
http://dx.doi.org/10.7196/samj.2018.v108i8.13394
CORRESPONDENCE
Variation in HIV prevalence and the population-level effects of antiretroviral therapy in reducing tuberculosis incidence in South Africa
To the Editor: The current year (2018) marks the 10th year after the tuberculosis (TB) epidemic in South Africa (SA) reached a historic peak of 848 incident TB cases per 100 000 population in 2008.[1,2] TB incidence has since decreased at an average of 2.0% annually to 781 per 100 000 in 2016.[1,2] The decline observed in the past decade has mainly been attributed to the expansion of HIV testing and antiretroviral therapy (ART).[1,2] Despite these and other public health efforts, TB remains a leading cause of death in SA,[1] and at the current rate of decline, SA will not reach the 2035 targets of the End TB Strategy.[3]
National-level observational and mathematical modelling studies suggest that further scale-up of ART could yield substantial reductions in TB incidence and mortality over the next two decades.[4,5] The effect of ART on halting and reversing local TB incidence depends on the extent to which TB (and transmission) in the population is attributable to HIV infection. To date, there is limited information about trends in HIV prevalence, ART coverage and TB at subnational level in SA. We reviewed data from the National Antenatal Sentinel HIV Prevalence Survey[6] and the District Health Barometer[7] to compare rates of TB and HIV in the 52 SA health districts. HIV prevalence estimates ranged from 2.3% to 46.9% in 2013 and were poorly associated with rates of reported TB in the districts (Fig. 1).
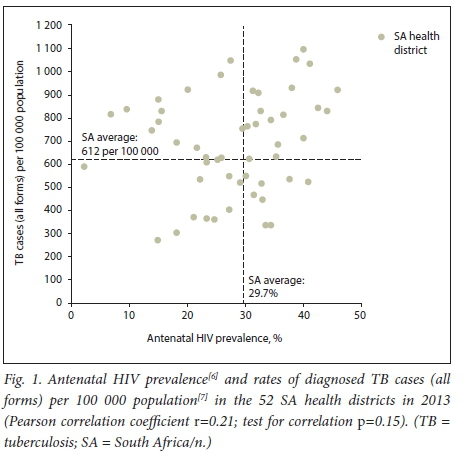
Several districts reported high TB rates (exceeding 700 per 100 000) despite relatively low estimates of HIV prevalence. We note that the observed variation in HIV and TB rates at subnational level has important implications for TB control in SA and therefore deserves further investigation. It is currently not known whether varying levels of ART coverage in the SA population explain the poor association between local TB and HIV rates, or to what extent other factors, such as poor TB case detection, initial loss to follow-up, failing delivery of integrated HIV-TB services and poor treatment outcomes, contribute to ongoing transmission and high TB rates.
We conclude that efforts are needed to better understand the determinants of local variation in TB and HIV rates in SA. Comprehensive data on the uptake and coverage of ART can guide ART scale-up in the forthcoming years and will inform projections of the effects that ART will have towards reducing TB in different parts of the country. An integrated control strategy that further strengthens HIV prevention and treatment but also effectively addresses other important barriers to TB control will help the country to make significant progress in the forthcoming years.[8]
R Sloot, G J Maarman, M Osman, F M Marx, on behalf of the Desmond Tutu TB Centre - Working Group Data Analysis and Modelling (complete list of Working Group members: Rory Dunbar, Karen du Preez, Marché Jaftha, Gerald Maarman, Sue-Ann Meehan, Muhammad Osman, James Seddon, Rosa Sloot, Redwaan Vermaak and Florian Marx (lead))
Desmond Tutu TB Centre, Department of Paediatrics and Child Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa rsloot@sun.ac.za
References
1. World Health Organization. Global Tuberculosis Report 2017. Geneva: WHO, 2017. [ Links ]
2. Nanoo A, Izu A, Ismail NA, et al. Nationwide and regional incidence of microbiologically confirmed pulmonary tuberculosis in South Africa, 2004 - 12: A time series analysis. Lancet Infect Dis 2015;15(9):1066-1076. https://doi.org/10.1016/S1473-3099(15)00147-4 [ Links ]
3. Naidoo P, Theron G, Rangaka MX, et al. The South African tuberculosis care cascade: Estimated losses and methodological challenges. J Infect Dis 2017;216(Suppl 7): S702-S713. https://doi.org/10.1093/infdis/jix335 [ Links ]
4. Chindelevitch L, Menzies NA, Pretorius C, Stover J, Salomon JA, Cohen T. Evaluating the potential impact of enhancing HIV treatment and tuberculosis control programmes on the burden of tuberculosis. J R Soc Interface 2015;12(106). https://doi.org/10.1098/rsif.2015.0146 [ Links ]
5. Pretorius C, Menzies NA, Chindelevitch L, et al. The potential effects of changing HIV treatment policy on tuberculosis outcomes in South Africa: Results from three tuberculosis-HIV transmission models. AIDS 2014;28(Suppl 1):S25-S34. https://doi.org/10.1097/QAD.0000000000000085 [ Links ]
6. National Department of Health, South Africa. The 2013 National Antenatal Sentinel HIV Prevalence Survey South Africa. Pretoria: NDoH, 2015. [ Links ]
7. Massyn N, Day C, Peer N, Padarath A, Barron P, English R, eds. District Health Barometer 2013/14. Durban: Health Systems Trust, 2014. [ Links ]
8. Churchyard GJ, Mametja LD, Mvusi L, et al. Tuberculosis control in South Africa: Successes, challenges and recommendations. S Afr Med J 2014;104(3 Suppl 1):244-248. https://doi.org/10.7196/SAMJ.7689 [ Links ]














