Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 no.6 Pretoria Jun. 2018
http://dx.doi.org/10.7196/samj.2018.v108i6.12983
RESEARCH
Outcomes of outpatient ureteral stenting without fluoroscopy at Groote Schuur Hospital, Cape Town, South Africa
S SinhaI; S Z JaumdallyII, III; F CassimIV; J WichtIV; L KaestnerIV; A PanackalV; C H JehleVI; P GovenderIV; S de JagerVII; E de WetVII; M DewarIV; M E KoliaVIII; S SalukazanaVII; C MoolmanIV; A P van den HeeverIX; B KowlessurX; G PintoXI; J LazarusIV
IMBBS, MS, FRCS (Glasg), FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIPhD; Division of Immunology, Institute of Infectious Disease and Molecular Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IIIPhD; School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IVMB ChB, MMed (Urol), FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VMD, FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VIMB ChB, MRCS (Lond), MMed (Urol), FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VIIMB ChB; Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VIIIMB ChB, FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IXMB ChB, FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
XMBBS, FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
XIMD, FC Urol (SA); Division of Urology, Department of Surgery, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND. Ureteral stenting is generally a theatre-based procedure that requires a multidisciplinary team and on-table imaging. Limited hospital bed numbers and theatre time in our centre in Cape Town, South Africa, have led us to explore an alternative approach.
OBJECTIVES. To see whether outpatient insertion of ureteric stents under local anaesthesia without fluoroscopy was a possible and acceptable alternative to theatre-based ureteral stenting.
METHODS. Ureteral stenting (double-J stents and ureteric catheters) was performed with flexible cystoscopy under local anaesthesia and chemoprophylaxis, but without fluoroscopic guidance, in an outpatient setting. Every patient had an abdominal radiograph and an ultrasound scan of the kidney after the procedure to confirm stent position.
RESULTS. Three hundred and sixteen procedures (276 double-J stents and 40 ureteric catheters) were performed in 161 men and 155 women. The overall success rate for the procedures was 85.4%, independent of gender (p=0.87), age (p=0.13), type of device inserted (p=0.81) or unilateral/bilateral nature of the procedure (p=1.0). Procedures with a successful outcome were performed in a significantly (p<0.0001) shorter median time (10 minutes (interquartile range (IQR) 5 - 15)) than failed procedures (20 minutes (IQR 10 - 30)). Patients with a pain score of >5 experienced a significantly (p=0.02) greater proportion of failure (27.3%) than patients with a pain score of <5 (12.5%). Difficulties were encountered in 23.7% of procedures, with a significantly higher proportion being registered in failed interventions compared with successful ones (82.6% v. 13.7%; p<0.0001).
CONCLUSIONS. The procedure was easily mastered and technically simple, and represents savings in cost, time and human resources in our setting.
Ureteral stenting is a vital part of a urology service. Ureteral stenting (double-J stents and ureteric catheters) is traditionally performed under general anaesthesia (GA) with fluoroscopic guidance. Some centres have reported on insertion of ureteric stents and catheters as an office-based procedure,[1-4] the reasons for performing the intervention on an outpatient basis including: (i) avoiding unnecessary admission; (ii) saving cost and time; (iii) avoiding the necessity of GA; (iv) patient tolerance of the procedure; and (v) minimal complications. Most of these centres have, however, performed the procedure using sedation as well as local anaesthesia, and under fluoroscopic guidance.
A few centres, however, have reported using fluoroscopic guidance for the procedure in selected cases only, such as in pregnant women when a rigid cystoscope is used[5] and for exchange of double-J stents.[6] To our knowledge, flexible cystoscope-assisted ureteral stenting on an outpatient basis without the use of fluoroscopy has not yet been reported. This procedure has been performed at our centre, Groote Schuur Hospital (GSH) in Cape Town, South Africa (SA),
for several years, resource limitations in the form of hospital bed numbers for admission and theatre time having led us to seek a safe, efficacious and well-tolerated alternative to the same procedure done under general anesthesia and fluoroscopic guidance.
Methods
Patients and outcomes
This study comprised a retrospective review of a series of patients undergoing ureteric stent or catheter insertion using flexible cystoscope guidance, performed on an outpatient basis at the Division of Urology, GSH, over the period July 2007 - June 2015. The main indication for ureteral stenting was obstruction due to ureteric stone complicated by non-resolving pain, failure of medical expulsive therapy, urinary tract infection or renal failure. We also did this procedure (ureteral catheterisation) before percutaneous nephrolithotomy to save time in theatre or a retrograde pyelogram. In most cases such urgent procedures could not be undertaken because of overbooked emergency and elective operative lists.
Ethical approval was obtained from the Human Research Ethics Committee at the University of Cape Town (ref. no. UCT 771/2015). Patients included in the study were identified from the records list of the Urology Clinic at GSH. A comprehensive database comprising patient demographic characteristics (age, gender, hospital fee), operative information (surgeon's name, operative time, nature of the procedure (stent or catheter), side (left, right or bilateral), outcome, pain score and difficulties) and postoperative complications was set up from data extracted from medical records.
Procedure
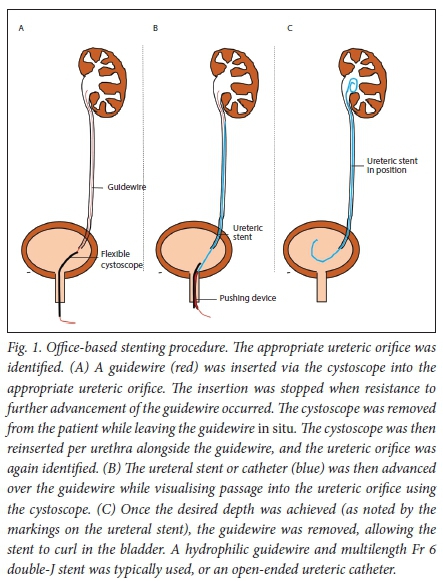
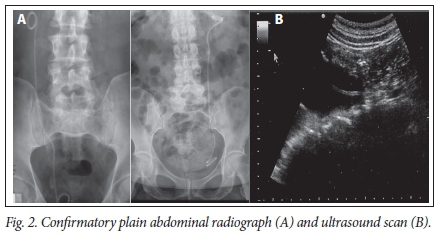
The procedure was performed with written informed consent from the patient and a single dose of prophylactic antibiotics (cefepime 400 mg/ciprofloxacin 500 mg orally depending on availability). If the patient was on a course of antibiotics for urosepsis, or a pre-procedural urine culture was positive, culture-specific antibiotics were given prior to the procedure. Anxious patients and those with complicated prior ureteric stent placement were taken to the main theatre for the stent to be placed under GA. The patient was positioned supine and anaesthetic gel (Remicaine Jelly 2%) was introduced per urethra after preparing and draping the patient. Flexible cystoscopy was performed as described in Fig. 1. Each patient was immediately asked to rate the level of pain using the '0 -10 Numeric Pain Rating Scale' (0 being the lowest and 10 being the highest).[7] The full procedure was performed without the assistance of fluoroscopic guidance or sedation. The patient was then allowed to empty his/her bladder and sent for a confirmatory plain abdominal radiograph to assess for adequate positioning of the stent after its position had been confirmed by ultrasonography at the bedside (Fig. 2). In the event of failure, the patient was admitted and placed on the emergency theatre list for the procedure to be attempted under GA. If the reason for failure was thought to be an impacted stone, a percutaneous nephrostomy was inserted (in the radiology department) instead.
Learning curve
We sought to understand the learning curve of flexible cystoscopic stent placement, using time to complete the procedure as a proxy measure of mastery.
Statistical analysis
Explorative univariate statistical analysis of the data extracted was done. Unpaired non-parametric data were compared using the Mann-Whitney Latest. Statistical inferences on binary sets of data were performed using Fisher's exact test. Statistical analyses were performed using GraphPad Prism version 5.0 for Windows (GraphPad Software, USA). All tests were two-tailed and p-values of <0.05 were considered significant.
Results
A total of 316 procedures were included in this study, performed in 161 men (median age 48 years (interquartile range (IQR) 38 - 57) and 155 women (median age 45 years (IQR 38 - 59)). These involved the insertion of 276 stents (250 (90.9%) being unilateral) and 40 catheters (all unilateral). The overall success rate for the procedures was 85.4% (270/316). As shown in Table 1, success was independent of gender (p=0.87), age (p=0.13), type of device inserted (p=0.81) or unilateral/bilateral nature of the procedure (p=1.0). Procedures with a successful outcome were performed in a significantly (p<0.0001) shorter median time (10 minutes (IQR 5 - 15)) than failed procedures (20 minutes (IQR 10 - 30)). When stratified across a pain score of ≤5 or >5, patients with a pain score of >5 experienced a significantly (p=0.02) greater proportion of failure (27.3%) than patients reporting a pain score of ≤5 (12.5%).
Learning curve
The initial phase of the supervised learning curve consisted of the first 10 successful procedures, for which the median completion time was 12 minutes (Fig. 3). There was a statistically significant improvement in time to successful completion, halving from 12 minutes at the start of the apprenticeship to 6 minutes following successful completion of ≥30 interventions.

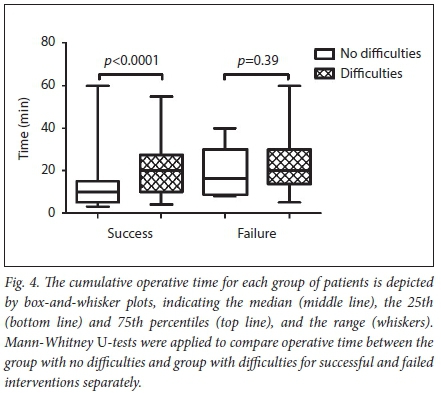
Difficulty
Overall, difficulties were encountered in 23.7% (75/316) of the interventions. Difficulty encountered during intervention was the main reason for failure, as is supported by the significantly different proportion of difficulty in failures (82.6%, 38/46) compared with successful procedures (13.7%, 37/270). It is of interest to note that difficulties did not necessarily lead to failure, as difficulties were encountered in 37 procedures in the successful group. Almost half of the difficulties leading to failures were due to impacted stone, but not all procedures with impacted stone ended up as failures, suggesting that careful perseverance resulted in success (Table 2). Stent blockage (encrustations), difficult angle of the ureteric orifice, trabeculated bladder and patient difficulty (procedure poorly tolerated by patient, language barrier and full bladder) represented 30.2% of the reported difficulties, but in most cases (83.4%) these were successfully dealt with during the procedure. Poor vision accounted for a third of all difficulties, and these included haematuria, cloudy urine, snowstorm, oedema, technical issues, and ureteric orifice not seen due to an enlarged prostatic middle lobe. Encountering any form of difficulty led to a significant increase in the median time required for the successful completion of the intervention (20 minutes with difficulties v. 10 minutes without difficulties; p<0.0001) (Fig. 4).
Complications
The overall complication rate reported for this procedure was very low (3.8%, 12/316). Two cases of complication were encountered in the failed set of interventions, as the stents were deployed distal to the impacted stone. Of the complications in successful interventions, seven were in patients with urinary tract infection/pyelonephritis and the other three were linked to stent migration.
Discussion
The development of flexible cystoscopy started through the novel use of the choledochoscope into the bladder (originally it was only meant for use in the common bile duct).[8] This breakthrough revolutionised the use of endoscopy in urology. Since then, there has been a paradigm shift in the use of endoscopy in urology from purely diagnostic to therapeutic management, not only in the bladder but also encompassing the upper urinary tract. With the advent of double-J stents, the extent of therapeutic management widened to incorporate the use of flexible ureteroendoscopy to disobstruct blocked ureters and alleviate obstructive uropathy.
Ureteric stents are one of the most common devices used by urologists. At our institution, where resources in terms of both infrastructure and medical personnel are limited, an alternative form of management was necessary to circumvent the long wait for theatre time. This study documents the convenience of an alternative method. We were able to demonstrate an 85.4% success rate with flexible cystoscopic stent insertion without fluoroscopy. These successful procedures could be performed in a median of 10 minutes. Sivalingam et al.[3] demonstrated that urgent ureteric stent placement for obstructing stones can be performed safely and effectively under local anaesthesia in the office.[3] The authors note that there is little in the literature on the use of ureteral stenting for renal colic under local anaesthesia. They used rigid as well as flexible cystoscopy under local anaesthesia with the addition of fluoroscopy, and reported a failure rate of 9% compared with our 15% failure rate without fluoroscopy or rigid cystoscopy.
Instead of office-based fluoroscopy, we used a post-procedure abdominal radiograph to check stent/catheter position. Kose et al[6]-described their technique for manual replacement of an (existing in situ) double-J stent without fluoroscopy in female patients. This method used cystoscopy to remove the stent and do a guidewire stent exchange, gently placing the end of the stent into the bladder without a scope and positioning without fluoroscopy.
Cost benefits
Gershman et al.[4] investigated how office-based placement of ureteric stents affects cost and hospital stay. They reported a three-fold reduction in total hospital time as a result of reduced preoperative waiting times. This achieved a saving of USD1 551 per procedure.
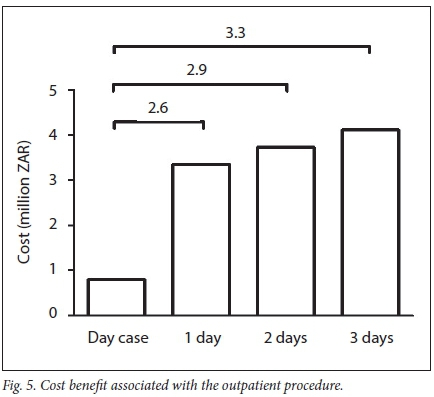
Fig. 5 provides a breakdown of cost-effectiveness associated with our proposed procedure. For our outpatient-based procedure, the patient would only be a day case, which is the reference situation used in a comparison of the 265 patients included in this study if they were to be admitted in hospital for a variable length of time (1, 2 or 3 days). After classifying patients based on their income bracket and calculating the incumbent cost of the procedure to the hospital after deduction of the patient's payment, a total saving of between ZAR2.6 million (USD162 500) if a 1-day hospital stay was required, and ZAR3.3 million (USD206 250) if a 3-day hospital stay was required, could be made. This represents a substantial saving in the current SA health system.
Tolerability
Although explanation and informed consent are vital to success with this procedure under local anaesthesia, we noted a statistically greater chance of failure with visual pain scores >5. Investigating this issue, Hussein et al.[9]recommended self-watching of the procedure on the video monitor together with a detailed explanation to reduce the pain and anxiety associated with the procedure.[9] They randomised patients to those allowed to and those prevented from viewing the procedure. The latter group had statistically greater visual analogue pain scores.
Learning curve
When we investigated the learning curve of this procedure, we found that operative time during the training of a set of registrars improved significantly, being halved from a median of 12 minutes for the initial set of 10 interventions to 6 minutes after successful completion of >30 interventions. This highlights the fact that it is relatively easy to learn this procedure, and the continuous flow of patients requiring it in our facility (a stone clinic) provides the perfect setting for rapid training of surgeons in the mastery of the technique.
Difficulty
We attempted to understand reasons for a failed procedure. Close to half of the difficulty encountered in the failed interventions was due to stone impaction. Pitfalls here include a deployed stent curling up below the impacted stone. Buckling of the guidewire in the bladder is another pitfall that has a potential to delay the procedure, but it can easily be avoided through the operator focusing carefully while introducing the guidewire into the ureter. Other challenging scenarios include an oedematous and inflamed ureteric orifice, bleeding, clots in the bladder, murky/turbid urine due to sepsis, or a blocked double J during stent exchange.
Study limitations
This study has certain limitations. Notably, it suffers from being an observational study. A randomised trial comparing equally skilled urological surgeons with a more comprehensive validated questionnaire would probably be needed to support our assertions about the safety, tolerability and efficacy of the procedure.
One criticism of this work could be that some of these patients would have been better served by being taken to the main theatre for ureteroscopy and definitive management of their stone. In our setting, emergency theatre time is very limited and logistics therefore prevent this option.
Conclusion
The ever-growing demand of surgical time on emergency slates in busy hospitals has forced the conception of an alternative outpatient procedure for the drainage of obstructed ureters by stenting. The current reliance on fluoroscopy and use of general anaesthesia for this procedure means that a significant number of patients do not reach theatre timeously. In a retrospective series of over 300 cases of flexible cystoscopic ureteral stenting without fluoroscopy, we believe that it is a safe, efficacious (85.4%) and well-tolerated procedure to deal with cases of ureteric obstruction. With a high volume of patients requiring this intervention in our setting, and motivated by the successful use of the office-based version of this procedure described in the literature, we introduced it for the first time in SA and were logically prompted to undertake a retrospective audit of data from these interventions to assess its practicality. It is established that stent insertions are done blindly without the need of fluoroscopy during laparoscopic pyeloplasty and ureteric reimplants,[10] and this encouraged us to translate this concept for our procedures.
Considering the good success rate associated with our intervention and challenges with regard to theatre time and availability of fluoroscopy in outpatient settings in SA health centres, we propose the roll-out of this alternative procedure in hospitals located in high-volume areas as a screening tool to alleviate the emergency operative workload. This will be especially helpful in the developing world, where the procedure can drastically reduce the waiting time for patients requiring ureteric stenting/catheterisation. We propose to evaluate this technique more vigorously through a randomised clinical trial.
Acknowledgements. This work was made possible through the valuable support of the nursing and administrative staff of the Division of Urology at GSH, specially Sr Millia Sojola, Sr Desire Abels, Sr Julia Jacabs, Sr Cecilia Wilson, Mr Phumlani Msi, Mrs Lesley Burke, Mrs Shene Isaacs, Mrs Zubaida Viljoen and Mr Gasant Harris.
Author contributions. SS and SZJ did the data analysis and wrote up the manuscript, to which they contributed equally. All the clinicians listed as authors were involved in performing the procedure and generating the data published. JL provided guidance for the draft manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Adeyogu A, Collins G, Brooman P, et al. Outpatient flexible cystoscope-assisted insertion of ureteric catheters and ureteric stents. BJU Int 1999;83(7):748-750. https://doi.org/10.1046/j.1464-410x.1999.00994.x [ Links ]
2. McFarlane JP, Cowan C, Holt SJ, et al. Outpatient ureteric procedures: A new method for retrograde ureteropyelography and ureteric stent placement. BJU Int 2001;87(3):172-176. https://doi.org/10.1046/j.1464-410x.2001.02039.x [ Links ]
3. Sivalingam S, Tamm-Daniels I, Nakada SY. Office-based ureteral stent placement under local anesthesia for obstructing stones is safe and efficacious. Urology 2013;81(3):498-502. https://doi.org/10.1016/j.urology.2012.10.021 [ Links ]
4. Gershman B, Eisner BH, Sheth S, et al. Ureteral stenting and retrograde pyelography in the office: Clinical outcomes, cost effectiveness, and time savings. J Endourol 2013;27(5):662-666. https://doi.org/10.1089/end.2012.0644 [ Links ]
5. Ngai H, Salih HQ, Albeer A, et al. Double-J ureteric stenting in pregnancy: A single-centre experience from Iraq. Arab J Urol 2013;11(2):148-151. https://doi.org/10.1016/j.aju.2013.02.002 [ Links ]
6. Kose O, Gorgel SN, Ozbir S, et al. Manual replacement of double J stent without fluoroscopy (double J stent replacement). Int Surg 2015;100(2):381-385. https://doi.org/10.9738/INTSURG-D-13-00248.1 [ Links ]
7. McCaffery M, Beebe A, Latham J. Pain: Clinical Manual for Nursing Practice. St Louis, Mo.: Mosby, 1994. https://doi.org/10.1016/0885-3924(90)90052-L [ Links ]
8. Wilbur H. The flexible choledochoscope: A welcome addition to the urologic armamentarium. J Urol 1981;126(3):380-381. https://doi.org/10.1016/S0022-5347(17)54535-8 [ Links ]
9. Hussein NS, Norazan MR. Impact of self-watching double J stent insertion on pain experience of male patients: A randomized control study using visual analog scale. ISRN Urol 2013 (2013), article ID 523625. https://doi.org/10.1155/2013/523625 [ Links ]
10. Chandrasekharam VVSS. Is retrograde stenting more reliable than antegrade stenting for pyeloplasty in infants and children? Urology 2005;66(6):1301-1304. https://doi.org/10.1016/j.urology.2005.06.132 [ Links ]
 Correspondence:
Correspondence:
S Sinha
s.sinha@uct.ac.za
Accepted 15 December 2017














