Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 no.3 Pretoria Mar. 2018
http://dx.doi.org/10.7196/samj.2018.v108i3.12876
IN PRACTICE
HEALTHCARE DELIVERY
Maternal near-miss audit in the Metro West maternity service, Cape Town, South Africa: A retrospective observational study
I A IwuhI, II; S FawcusIII; L SchoemanIV
IMB BS, FCOG, MMed; Princess Marina Hospital and University of Botswana, Gaborone, Botswana
IIMB BS, FCOG, MMed; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Cape Town, South Africa
IIIMB ChB, FRCOG, MA; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Cape Town, South Africa
IVMB BCh, FRCOG; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND. A maternal near-miss is defined as a life-threatening pregnancy-related complication where the woman survives. The World Health Organization (WHO) has produced a tool for identifying near-misses according to criteria that include the occurrence of a severe maternal complication together with organ dysfunction and/or specified critical interventions. Maternal deaths have been audited in the public sector Metro West maternity service in Cape Town, South Africa, for many years, but there has been no monitoring of near-misses.
OBJECTIVES. To measure the near-miss ratio (NMR), maternal mortality ratio (MMR) and mortality index (MI), and to investigate the near-miss cases.
METHODS. A retrospective observational study conducted during 6 months in 2014 identified and analysed all near-miss cases and maternal deaths in Metro West, using the WHO criteria.
RESULTS. From a total of 19 222 live births, 112 near-misses and 13 maternal deaths were identified. The MMR was 67.6 per 100 000 live births and the NMR 5.83 per 1 000 live births. The maternal near-miss/maternal death ratio was 8.6:1 and the MI 10.4%. The major causes of near-miss were hypertension (n=50, 44.6%), haemorrhage (n=38, 33.9%) and puerperal sepsis (n=13, 11.6%). The first two conditions both had very low MIs (1.9% and 0%, respectively), whereas the figure for puerperal sepsis was 18.9%. Less common near-miss causes were medical/surgical conditions (n=7, 6.3%), non-pregnancy-related infections (n=2, 1.8%) and acute collapse (n=2, 1.8%), with higher MIs (33.3%, 66.7% and 33.3%, respectively). Critical interventions included massive blood transfusion (34.8%), ventilation (40.2%) and hysterectomy (30.4%). Considering health system factors, 63 near-misses (56.3%) initially occurred at a primary care facility, and the patients were all referred to the tertiary hospital; 38 (33.9%) occurred at a secondary hospital, and 11 (9.8%) at the tertiary hospital. Analysis of avoidable factors identified lack of antenatal clinic attendance (11.6%), inter-facility transport problems (6.3%) and health provider-related factors (25.9% at the primary level of care, 38.2% at secondary level and 7.1% at tertiary level).
CONCLUSIONS. The NMR and MMR for Metro West were lower than in other developing countries, but higher than in high-income countries. The MI was low for direct obstetric conditions (hypertension, haemorrhage and puerperal sepsis), reflecting good quality of care and referral mechanisms for these conditions. The MIs for non-pregnancy-related infections, medical/surgical conditions and acute collapse were higher, suggesting that medical problems need more focused attention.
In the past decade, maternal near-miss audits have been introduced as an additional method for monitoring maternal health outcomes. A maternal near-miss describes a life-threatening event or complication occurring during pregnancy or within 42 days after the end of the pregnancy that may lead to acute severe morbidity, but not to death. The near-miss ratio (NMR) is measured per 1 000 live births.[1]
Life-threatening conditions (LTCs) are defined as severe pregnancy-related complications that cause organ dysfunction and/ or require major interventions and may result in maternal death. LTCs lead to severe maternal outcomes that include both near-misses and deaths.
Globally, much attention has been directed towards reducing maternal mortality, with the Millennium Development Goals and now the Sustainable Development Goals. The latter has the target of ending preventable maternal mortality by reducing the maternal mortality ratio (MMR) by two-thirds by 2030.[2,3]
The Confidential Enquiry into Maternal Deaths in South Africa (SA) was introduced in 1998, and triennial reports show the MMR to be much higher than in developed countries, but slightly lower than the average for sub-Saharan Africa.[4,5] The most recent triennial report shows that the institutional MMR, after an initial steep rise from 150 per 100 000 in 1998, decreased from 176.2 per 100 000 in 2008 - 2010 to 154.1 in 2011 - 2013.[6] The five main causes of maternal mortality in SA for 2011 - 2013 were non-pregnancy-related infections, including HIV-related infections such as tuberculosis and pneumonia (34.7%), obstetric haemorrhage (15.8%), hypertension (14.8%), medical and surgical disorders (11.4%) and pregnancy-related sepsis (5.2%).
Near-miss audits have become part of ongoing monitoring systems in many well-resourced countries, and are now being introduced in several poorly resourced settings. In the UK, where the MMR is <10 per 100 000 live births, there is an ongoing national surveillance system (the United Kingdom Obstetric Surveillance System) that measures and monitors all cases with severe acute maternal morbidity (near-misses). This includes obstetric conditions such as eclampsia, obstetric haemorrhage, pulmonary embolism and peripartum cardiomyopathy.[7] One of the first near-miss audits to be performed in a lower-resourced setting was conducted by Mantel et αl.[8]in Pretoria in 1998.
There have been several near-miss audits in different settings, which have used various definitions of near-miss based on clinical criteria and/or organ dysfunction-based criteria and/or intervention-based criteria.[9-12] In order to standardise definitions of near-misses as well as audit them, the World Health Organization (WHO) developed a very useful tool to assist countries and facilities to set up their own near-miss audits.[13] It includes clear definitions, as well as near-miss data collection forms that can be adapted to local settings.
Audits of maternal near-misses give the healthcare system the opportunity to improve insight into issues surrounding quality of care, because near-misses are more frequent than maternal deaths.114 An indicator called the mortality index (MI) (maternal deaths expressed as a percentage of total numbers of LTCs) is a useful indicator of quality of care.[13,14] When a woman experiences an LTC and survives, practitioners are able not only to identify the positive or negative components of her care, but also to elucidate any difficulties she experienced in seeking care or lack of understanding she had of her health problems.[15]
In the Metro West maternity service of Cape Town, SA (formerly the Peninsula Maternal and Neonatal Service), maternal mortality has been systematically monitored since 1953, but there has been no system of measuring and monitoring near-misses.[16]
Objectives
To identify all women with life-threatening obstetric conditions and estimate the NMR, MMR and MI, to identify the severe maternal complications causing the near-misses and maternal deaths, and to perform an in-depth investigation of the near-miss cases for demographic characteristics, clinical factors and avoidable factors occurring in the health system. It was anticipated that the process of conducting this study could provide input to the future development of an ongoing system for monitoring near-misses in Metro West.
Methods
A retrospective observational study was conducted over 6 months between mid-March 2014 and mid-September 2014 in the Metro West maternity service. This service includes nine primary care maternity facilities (midwife obstetric units), which refer all complicated maternal cases to two secondary hospitals, New Somerset Hospital and Mowbray Maternity Hospital, or to the maternity centre at the tertiary hospital, Groote Schuur Hospital (GSH).
The sample size was calculated from a practical estimate of 38 000 deliveries per year in Metro West, with an average of 20 - 30 maternal deaths per annum. We used a presumed MI of 10%, which would give a figure of at least 100 women with LTCs during a 6-month period.
All near-miss cases managed at the three hospitals were identified weekly by the author, with the assistance of on-site healthcare providers. These cases included near-misses that occurred at primary care facilities and were referred to one or more of the three hospitals. Strict criteria were used to ascertain a case as a near-miss according to the following WHO criteria:[13](i) the woman sustained a near-miss-defining severe maternal complication such as eclampsia or a ruptured uterus; or (ii) the woman had a severe maternal complication that was insufficient to classify it as a near-miss on its own, but had in addition one or more specified organ dysfunctions, and/or one or more defined critical interventions.
The folders of all the near-misses were reviewed and relevant data were entered into a data collection form adapted from the WHO near-miss form. In addition, the folders were reviewed by two senior obstetric specialists to confirm adherence to the WHO inclusion criteria for near-miss classification, and also to determine avoidable factors in the management of the near-miss cases. The classification of avoidability was done using the criteria used for assessing maternal deaths by the National Committee for Confidential Enquiry into Maternal Deaths, which grouped them into patient-related, administrative and health provider-related factors.[4,5]
Maternal deaths occurring during the time period of the near-miss audit were identified from monthly mortality meetings and the ongoing maternal mortality audit system in Metro West. Live births occurring during the study period in all the 12 facilities of Metro West were obtained from the hospital information system CLINICOM and routinely measured perinatal statistics, for the denominator in measuring ratios.
Results
A total of 112 maternal near-miss cases and 13 maternal deaths in the Metro West maternity service were identified between 15 March 2014 and 15 September 2014. There was therefore a total of 125 women with severe maternal outcomes. There were 19 524 deliveries and 19 222 live births in Metro West maternity facilities during the same time period. Table 1 shows the maternal near-miss indicators.
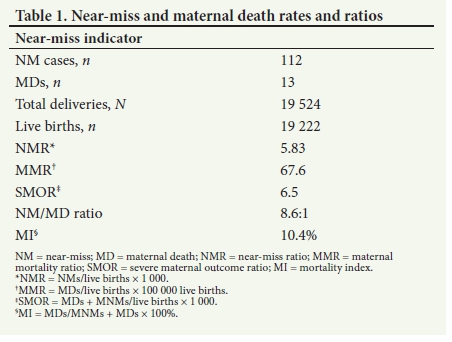
The NMR was 5.83 near-miss cases per 1 000 live births, and the MMR was 67.6 maternal deaths per 100 000 live births. The maternal near-miss/maternal death ratio was 8.6:1 and the MI was 10.4%. Note that these indicators refer to mortality and morbidity in the facilities of Metro West and are institutional ratios. Table 2 shows sociodemographic characteristics of the women with near-misses. Most of the women lived in low-income and high-density areas of Cape Town, with the largest proportions from Gugulethu (38.4%) and Mitchells Plain (24.1%). The majority of the women (88.4%) had booked for antenatal care. Twenty-five (22.3%) of the women were HIV-positive.
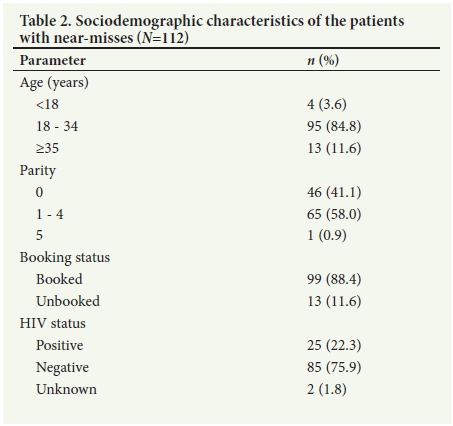
Table 3 presents the clinical complications causing the near-misses and maternal deaths, and the MI for each complication. Hypertension, obstetric haemorrhage and pregnancy-related sepsis were the most frequent clinical complications causing the near-misses, accounting for 50 (44.6%), 38 (33.9%), and 13 (11.6%), respectively. Hypertension and haemorrhage had very low Mis of 1.9%, and 0%, respectively, while for pregnancy-related sepsis the figure was higher at 18.9%.
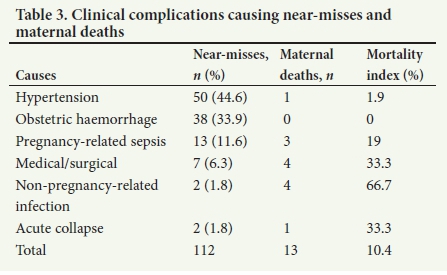
Less common conditions causing near-misses were medical/surgical conditions, non-pregnancy-related infections and acute collapse, accounting for 7 (6.3%), 2 (1.8%), and 2 (1.8%) near-misses, respectively. Although the numbers were small, these three conditions accounted for proportionately more maternal deaths, with MIs of 66.7%, 33.3% and 33.3% for non-pregnancy-related sepsis, medical/ surgical conditions and acute collapse, respectively.
Organ dysfunction occurred in 52 (46.4%) of the 112 near-misses; 30 women had dysfunction of one organ and 22 dysfunction of two or more. The most common organ dysfunctions were circulatory and respiratory, occurring in 36.6% and 22.3% of near-misses, respectively. Other organ dysfunctions were renal (13.4%), coagulation (9.8%) and neurological (3.6%).
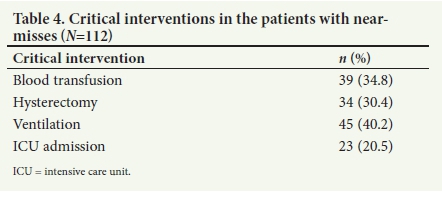
Table 4 shows that the 112 women with near-misses underwent 141 critical interventions (some women had more than one). These included 39 women (34.8%) who had massive blood transfusion (>5 units of red cells), 34 (30.4%) who had a hysterectomy, 45 (40.2%) who required intubation and ventilation, and 23 (20.5%) who were admitted to the tertiary hospital main intensive care unit. Of note, 19 (50.0%) of women with near-misses from haemorrhage and all 13 with near-misses from pregnancy-related sepsis had a hysterectomy.
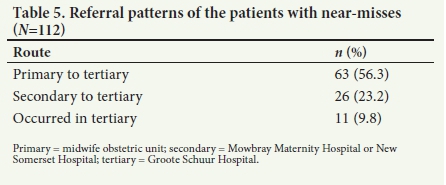
In terms of health system factors, 63 (56.3%) of the near-misses initially occurred at a primary care facility, and were all referred to the tertiary hospital (GSH); 38 (33.9%) of near-misses initially occurred at the secondary hospitals and 11 (9.8%) at the tertiary hospital (GSH). Table 5 shows the referral patterns: all near-misses occurring at primary care were referred to the tertiary hospital, and 26 of the 38 occurring at the secondary hospitals were referred to the tertiary hospital.
Avoidable factors were classified into patient-related, administrative and healthcare provider-related factors according to the system used in the SA Saving Mothers reports.[4,5] These were identified by the two specialist obstetricians who reviewed the near-miss folders.
Table 6 shows that there was a high proportion of cases in which no patient-related or administrative avoidable factors were identified: 78.6% and 81.3%, respectively. Avoidable factors that occurred frequently in these two categories were lack of antenatal clinic attendance and inter-facility transport problems (particularly from primary level to tertiary hospital).
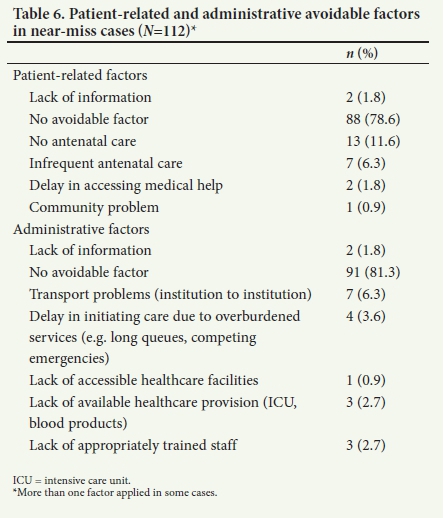
Table 7 shows the problems in clinical management by healthcare providers at different levels of care. Most avoidable factors were identified at secondary hospitals (n=25, 65.8%), followed by primary (n=21, 33.3%) and tertiary level (n=10, 90.1%). Sub-standard care was the most common healthcare provider-related factor at secondary hospitals. Examples were delayed intervention for prolonged labour, and inadequate monitoring resulting in the discovery that a patient was in shock a few hours after delivery. At primary care level, the most frequent avoidable factors were poor problem recognition and inadequate monitoring. At tertiary level, the main avoidable factor was delay in initiating appropriate treatment (e.g. delay in starting magnesium sulphate and planning delivery when eclampsia was imminent).
Discussion
The current study used the WHO near-miss audit tool for defining and investigating near-misses, as well as calculating rates and ratios.[13] However, we adapted the WHO list of severe maternal complications to include the additional categories of acute collapse/ thromboembolism, non-pregnancy-related infections and medical/ surgical disorders. The WHO criteria for organ dysfunction and critical interventions were strictly followed in order to identify cases as near-misses. We added a section to the audit tool that enabled a quality of care assessment by two independent specialists who evaluated cases for avoidable factors. These modifications of the WHO audit tool appeared to add value to the data and could be considered when the WHO near-miss audit tool is next updated.
In our setting we were able to apply the WHO criteria for ascertaining near-misses because of ready availability of laboratory services for evaluating organ failure and sufficient access to life-saving interventions such as blood products and intensive care. In many poorly resourced settings these are not available, which would limit the identification of near-miss cases.[17]
A recent near-miss study in Tanzania modified the WHO criteria to be more reliant on clinical criteria and less on stringent laboratory criteria and intervention criteria (e.g. 2 units of blood rather than 5 units).[18] This modification may be relevant for poorly resourced settings.
Our study identified 13 maternal deaths and 112 maternal near-misses. The NMR was 5.83 per 1 000 live births, which is comparable to studies in Pakistan, India and Baghdad, with rates of 8.6, 4.4 and 5.06, respectively.[19-21] Our NMR was higher than in several developed countries, such as Canada, the UK and Scotland, where the NMR was 0.7, 1.2 and 1.34 per 1 000, respectively.™ Possible explanations for this finding are the higher proportion of women in our study population living in poverty, a higher prevalence of HIV, and a less well developed health system. A study in the USA had an MMR of 6.5 deaths per 100 000 live births, which is 10 times lower than the MMR in our study.[11] However, the NMR was 8.1 per 1 000, which is higher than the NMR of 5.83 in our study. A possible explanation could be that lowering of MMRs may translate to a high NMR because women who survived but almost died will join the pool of women who end up as near-misses.
The severe maternal outcome ratio of 6.5 per 1 000 in our study is similar to the rate of 5 per 1 000 found in a recent population-based study in Pretoria, SA.[22]
Our study found an overall MI of 10.4%, which is slightly lower than those in the Pretoria study, which had an overall MI of 14%,[22] and the Pakistan and Baghdad studies, with MIs of 12 % and 11%, respectively.[19,21]
Our MI was very low for hypertensive disorders (1.9%) and haemorrhage (0%), and higher for pregnancy-related sepsis (18.9%). The Pretoria study also had a low MI for haemorrhage of 2%,[22] whereas in Pakistan it was much higher at 17.2%.[19] An audit in Johannesburg on morbidity and mortality from obstetric haemorrhage in caesarean deliveries showed an MI of 7% (93 near-misses and 7 maternal deaths),[23] and although our study did not focus on morbidity/mortality from caesarean deliveries, we found a caesar-ean section rate of 62.5% and 33.9% of near-misses due to obstetric haemorrhage, with an MI of 0%. The lower MI in SA studies could reflect better prevention and/or management of obstetric haemorrhage in SA. Similarly, the MI for hypertensive disorders in our study was found to be low, at 1.9%; this is lower than the Pretoria study's MI of 13.6%.[22]
The relatively low MIs for direct obstetric conditions in the Metro West maternity service compared with other low-resource settings reflect reasonable quality of care and a functional health system. There are clear referral guidelines, and the levels of care in the maternity system are interconnected via clinical outreach and a well-established system of clinical governance and emergency transport. There are also regular mortality meetings and in-service training at all levels of care. Clear protocols exist for prevention and management of obstetric emergencies. These are particularly effective for obstetric haemorrhage and eclampsia/severe pre-eclampsia, where clinical management tends to be aggressive. The tiered system of care allows the tertiary level to provide critical individualised care for very sick women. Of note, 56.3% of near-misses occurred at primary care facilities and were referred timeously to tertiary level. The Pretoria study had a corresponding figure of 39.3%.[21] However, in terms of avoidable factors, our study showed that 26.3% of the near-miss cases at secondary level had substandard care, while 36.4% of the near-miss cases at tertiary level had substandard care. These findings are consistent with the findings in another recent study in Pretoria[24] looking at the barriers to obstetric care in maternal near-miss cases, where 36% were found to have received substandard care.
The high MIs associated with medical disorders and acute collapse (33.3% and 33.3%, respectively) in our study are consistent with other studies,[19,21,22] but our MI for non-pregnancy-related infections was very high at 66.7%, reflecting the disease burden of the HIV epidemic in SA. These high MIs suggest that these conditions need more focused attention, although their numbers as causes of deaths and near-misses were probably too small to draw conclusions.
Notably, with regard to AIDS-related infection, recent policies and clinical management protocols show extended scope and coverage. A significant reduction in HIV-related maternal mortality is the major reason for SA's recent fall in MMR.[6
Despite the results showing comparatively low MIs in Metro West there is still considerable room for improvement, as evidenced by the description of healthcare provider avoidable factors for near-misses.
Study limitations
The study was only done over a 6-month period, so the numbers were not sufficient to compare maternal deaths with near-misses or to draw conclusions about the less common causes of near-misses. In addition, risk factors for near-misses could not be identified because background demographic and clinical data were not available for the whole obstetric population during the study period. The lack of population data also meant that comparisons of near-miss rates in different areas of Cape Town could not be calculated
The study design did not enable in-depth interviews of the women with near-misses about factors related to social determinants and their experiences of accessing and receiving care, as has been done in some settings.[15] We also did not do any medium- or long-term follow-up of the women with near-misses to assess the impact of the severe morbidity on their subsequent physical and emotional wellbeing, which could have been considerable.
Conclusions
The NMR and MMR in Metro West were lower than in some other developing countries, but higher than rates in high-income countries. The most common conditions resulting in near-misses were obstetric haemorrhage, hypertensive disorders and pregnancy-related sepsis, but the MIs for these conditions were low, reflecting good quality of care and referral mechanisms for these conditions. The MIs for non-pregnancy-related infections, medical/surgical conditions and acute collapse were much higher, suggesting that medical problems may need more focused attention. The barriers to obstetric care are the avoidable factors at all three levels and substandard care, which seem to be common problems. The study showed that the WHO near-miss audit tool was effective for measuring severe maternal morbidity and quality of care in the Metro West maternity facilities. Near-miss auditing was found to be feasible, and ongoing routine audits would be valuable for the Metro West maternity service. This would require institutionalisation of the near-miss identification and monitoring systems.
Acknowledgements. We thank the staff of Metro West for assisting with identification of cases and Dr Greg Petro for assisting with statistics.
Author contributions. IAI and SF developed the proposal. IAI performed the research with input from SF and LS for assessing folders for substandard care. IAI did the final write-up, assisted by SF.
Funding. None.
Conflicts of interest. None.
References
1. Pattinson R, Say L, Souza J, van den Broek N, Rooney C. WHO Working Group on Maternal Mortality and Morbidity Classification. Bull World Health Organ 2009;87(10):734-734. https://doi.org/10.2471/BLT0.9.071001 [ Links ]
2. UNICEF. Millennium Development Goals, 2010. unicef.org/mdg/maternal.html (accessed 14 February 2018). [ Links ]
3. World Health Organization. Target and Strategies for Ending Preventable Maternal Mortality. Geneva: WHO, 2014. [ Links ]
4. Theron GB. Saving Mothers: Report on the Confidential Enquiries into Maternal Deaths in South Africa S Afr Fam Pract 2000;2(7):5-http://ww.safpj.co.za/index.php/safpj/article/view/2134/2698 (accessed 14 February 2018). [ Links ]
5. Pattinson RC, ed. Saving Mothers: Fifth report on Confidential Enquiries into Maternal Deaths in South Africa 2008 - 2010. Pretoria: National Department of Health, 2012. http://sanac.org.za/wp-content/uploads/2015/12/Report_on_Confidential_Enqifiries_into_Maternal_Deaths_ in_South_Africa.pdf (accessed 14 February 2018). [ Links ]
6. Gebhardt GS, Fawcus S, Moodley J, Farina Z. Maternal death and caesarean section in South Africa: Results from the 2011 - 2013 Saving Mothers Report of the National Committee for Confidential Enquiries into Maternal Deaths. S Afr Med J 2015;105(4):287-291. https://doi.org/10.7196/SAMJ.9531 [ Links ]
7. Sarris I, Bewley S, Sangeeta A, Oxford Specialty Training in Obstetrics and Gynecology. New York: Oxford University Press, 2009:298, Maternal collapse, box 10.1. [ Links ]
8. Mantel GD, Buchmann E, Rees H, Pattinson RC. Severe acute maternal morbidity: A pilot study of a definition of a near miss. Br J Obstet Gynaecol 1998;105(9):985-990. [ Links ]
9. Fitzpatrick C, Halligan A, Phelan D. Near miss maternal mortality. Ir Med J 1992;85(1):37. [ Links ]
10. Ronsmans C. Severe acute maternal morbidity in low income countries. Best Pract Res Clin Obstet Gynecol 200933(3):305-331. https://doi.org/10.1016/j.bpobgyn.2009.01.001 [ Links ]
11. Kuklina EV, Meikle SF, Jamieson DJ, Whiteman MK, Barfield WD, Hills SD. Severe obstetric morbidity in the United States 1998 - 2005. Obstet Gynecol 2009;113(2 pt 1):293-299. https://doi.org/10.1097/AOG.0b013e3181954e5b [ Links ]
12. Olufemi T Oladapo, Adewale O, Adetola O, Olusoji J. Near-miss obstetric events and maternal deaths in Sagamu, Nigeria. Reprod Health 2005;2:9. https://doi.org/10.1186/1742-4755-2-9 [ Links ]
13. World Health Organization. Evaluating the quality of care for severe pregnancy complications: The WHO near-miss approach for maternal health. 2011. http://www.who.int/reproductivehealth/publications/monitoring/9789241502221/en/ (accessed 14 February 2018). [ Links ]
14. Souza JP, Cecatti JG, Haddad SM, et al. The WHO maternal near miss approach and the maternal severity index model: Tools for assessing the management of severe maternal morbidity; PLoS One 2012;7(8):e44129. https://doi.org/10.1371/journal.pone.0044129 [ Links ]
15. Hinton L, Locock L, Knight M. Experience of quality of care of women with near miss maternal morbidities in the UK. Br J Obstet Gynecol 2014;121(Suppl 4):20-23. https://doi.org/10.1111/1471-0528.12800 [ Links ]
16. Fawcus SR, van Coeverden de Groot HA, Isaacs S. A 50 year audit of maternal mortality in the Peninsula maternal and neonatal service, Cape Town (1953 - 2002). BJOG 2005;112(9):1257-1263. https://doi.org/10.1111/j.1471-0528.2005.00601.x [ Links ]
17. Van den Akker T, Beltman J, Leyten J, Mwagomba B Meguid T. The WHO maternal near miss approach: Consequences at Malawian district level. PLoS One 2013;8(1):e54805. https://doi.org/10.1371/journal.pone.0054805 [ Links ]
18. Nelissen E, Mduma E, Broerse J, et al. Applicability of WHO maternal miss criteria in a low-resource setting. PLoS One 2013;8(4):e61248 https://doi.org/10.1371/journal.pone.0061248 [ Links ]
19. Mushtapha R, Hashmi H. Near miss obstetrical events and death. J Coll Physicians Surg Pak 2009;19(12):781-785. https://doi.org/12.2009/JCPSP.781785 [ Links ]
20. Chhabra P. Maternal near miss, an indicator for maternal health and maternal care. Indian J Community Med 2014;39(3):132-137. https://doi.org/10.4103/0970-0218.137145 [ Links ]
21. Jabir M, Abdul-Salam I, Suheil DM, et al. Maternal near miss and quality of maternal Care in Baghdad. BMC Pregnancy Childbirth 2013;13:11. https://doi.org/10.1186/1471-2393-13-11 [ Links ]
22. Soma-Pillay P, Pattinson RC, Langa-Mlambo L, Nkosi BSS, Macdonald AP. Maternal near miss and maternal death in the Pretoria Academic Complex, South Africa: A population-based study. S Afr Med J 2015;105(7):578-583. https://doi.org/10.7196/SAMJnew.8038 [ Links ]
23. Maswine TS, Buchmann E, Near-miss maternal morbidity from severe haemorrhage at caesarean section: A process and structure audit of system deficiencies in South Africa. S Afr Med J 2017;107(11):1005-1009. https://doi.org/10.7196/SAMJ.2017.v107i11.12340 [ Links ]
24. Soma-Pillay P, Pattinson RC. Barriers to obstetric care by maternal near-misses: A descriptive study. S Afr Med J 2016;106(11):1110-1113. https://doi.org/10.7196/SAMJ.2016.v106i11.10726 [ Links ]
 Correspondence:
Correspondence:
IA Iwuh
paurasi.iwuhl@gmail.com
Accepted 6 November 2017














